1 Introduction to the Catheterization Laboratory
Cardiac catheterization is the insertion and passage of small plastic tubes (catheters) into arteries and veins to the heart to obtain x-ray pictures (angiography) of coronary arteries and cardiac chambers and to measure pressures in the heart (hemodynamics). The cardiac catheterization laboratory performs angiography to obtain images not only to diagnose coronary artery disease but also to look for diseases of the aorta and pulmonary and peripheral vessels. In addition to providing diagnostic information, the cardiac catheterization laboratory performs catheter-based interventions (e.g., angioplasty and stents, now called percutaneous coronary intervention [PCI]) or catheter-based treatments of structural heart disease for both acute and chronic cardiovascular illness. Table 1-1 lists procedures that can be performed with coronary angiography. Figure 1-1 shows common access routes for cardiac catheterization.
Table 1-1 Procedures That May Accompany Coronary Angiography∗
| Procedure | Comment |
|---|---|
| Used as IV access for emergency medications (femoral, internal jugular, subclavian) or fluids, temporary pacemaker (pacemaker not mandatory for coronary angiography) | |
| Routine for all studies (aorta, left ventricle) | |
| Not routine for coronary artery disease; combined pressures; mandatory for valvular heart disease; routine for CHF, right ventricular dysfunction, pericardial diseases, cardiomyopathy, intracardiac shunts, congenital abnormalities | |
| Routine for all studies; may be excluded with high-risk patients, left main coronary or aortic stenosis, severe CHF, renal failure | |
| Not routine unless used as coronary bypass conduit | |
| Routine for all coronary angiography | |
| Routine for aortic insufficiency, aortic dissection, aortic aneurysm, with or without aortic stenosis, routine to locate bypass grafts not visualized by selective angiography | |
| Arrhythmia evaluation | |
| Available for patients prone to access site bleeding |
CHF, congestive heart failure; IV, intravenous; NTG, nitroglycerin; PTCA, percutaneous transluminal coronary angioplasty.
∗ See Table 1-2 for indications.
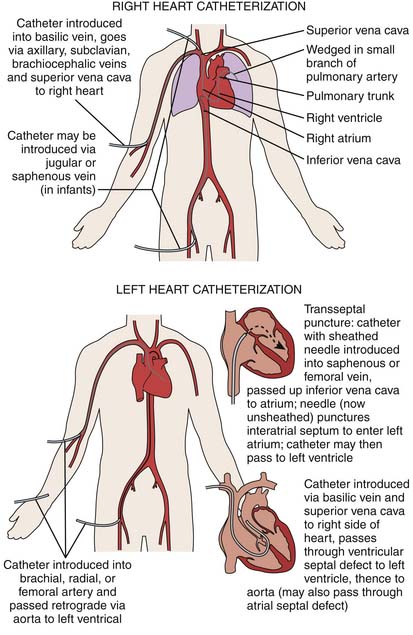
Figure 1-1 Vascular access routes for cardiac catheterization (also see Chapter 2). Radial and femoral arteries are the most common approaches.
Indications for Cardiac Catheterization
Cardiac catheterization is used to identify structural cardiac diseases such as atherosclerotic artery disease, abnormalities of heart muscle (infarction or cardiomyopathy), and valvular or congenital heart abnormalities. In adults the procedure is used most commonly to diagnose coronary artery disease. Other indications depend on the history, physical examination, electrocardiogram (ECG), cardiac stress test, echocardiographic results, and chest radiograph. Indications for cardiac catheterization are summarized in Table 1-2.
Table 1-2 Indications for Cardiac Catheterization
| Indications | Procedures |
|---|---|
| LV, COR | |
| LV, COR | |
| LV, COR | |
| LV, COR, ±ERGO | |
| LV, COR, ±ERGO | |
| LV, COR, ±ERGO | |
| LV, COR | |
| LV, COR, ±RH | |
| LV, COR, RH | |
| LV, COR, L+R | |
| LV, COR, R + L | |
| LV, COR, R + L, ±AO | |
| LV, COR, R + L, ±AO | |
| AO, COR | |
| LV, COR, R + L | |
| LV, COR, R + L, ±BX | |
| LV, COR, R + L, BX |
AO, aortography; BX, endomyocardial biopsy; COR, coronary angiography; ERGO, ergonovine malate,; LV, left ventriculography; RH, right heart oxygen saturations and hemodynamics (e.g., placement of Swan-Ganz catheter); R + L, right and left heart hemodynamics; ±, optional.
Urgent Procedures
If the patient’s condition is unstable because of a suspected cardiac disorder, such as acute myocardial infarction, catheterization must proceed. In the event of decompensated congestive heart failure, rapid medical management is often needed. Although a patient must be able to lie flat for easy catheter passage, patients with acute cardiac decompensation may benefit more from aggressive management in the catheterization laboratory than from management in an intensive care unit. In the catheterization laboratory, intubation, intraaortic balloon pumping, and vasopressors can be instituted rapidly before angiography and a decision for revascularization.
Contraindications
Contraindications to cardiac catheterization include fever, anemia, electrolyte imbalance (especially hypokalemia predisposing to arrhythmias), and other systemic illnesses needing stabilization (Table 1-3).
Table 1-3 Contraindications to Cardiac Catheterization
| Absolute Contraindications |
| Inadequate equipment or catheterization facility |
| Relative Contraindications |
| Acute gastrointestinal bleeding or anemia |
| Anticoagulation (or known, uncontrolled bleeding diathesis) |
| Electrolyte imbalance |
| Infection and fever |
| Medication intoxication (e.g., digitalis, phenothiazine) |
| Pregnancy |
| Recent cerebrovascular accident (<1 month) |
| Renal failure |
| Uncontrolled congestive heart failure, high blood pressure, arrhythmias |
| Uncooperative patient |
Complications and Risks
For diagnostic catheterization, analysis of the complications in more than 200,000 patients indicated the incidence of risks as death, less than 0.2%; myocardial infarction, less than 0.05%; stroke, less than 0.07%; serious ventricular arrhythmia, less than 0.5%; and major vascular complications (thrombosis, bleeding requiring transfusion, or pseudoaneurysm), less than 1% (Table 1-4, Table 1-5). Vascular complications occurred more often when the brachial approach was used and least when the radial approach was used. Risks are increased in well-described subgroups (Table 1-6).
Table 1-4 Complications of Cardiac Catheterization
| Major |
| Cerebrovascular accident |
| Death |
| Myocardial infarction |
| Ventricular tachycardia, fibrillation, or serious arrhythmia |
| Other |
| Aortic dissection |
| Cardiac perforation, tamponade |
| Congestive heart failure |
| Contrast reaction (anaphylaxis, nephrotoxicity) |
| Heart block, asystole |
| Hemorrhage (local, retroperitoneal, pelvic) |
| Infection |
| Protamine reaction |
| Supraventricular tachyarrhythmia, atrial fibrillation |
| Thrombosis, embolus, air embolus |
| Vascular injury, pseudoaneurysm |
| Vasovagal reaction |
Table 1-5 Incidence of Major Complications of Diagnostic Catheterizations
| Number | Percent | |
|---|---|---|
| Death | 65 | 0.11 |
| Myocardial infarction | 30 | 0.05 |
| Neurologic | 41 | 0.07 |
| Arrhythmia | 229 | 0.38 |
| Vascular | 256 | 0.43 |
| Contrast | 223 | 0.37 |
| Hemodynamic | 158 | 0.26 |
| Perforation | 16 | 0.03 |
| Other | 166 | 0.28 |
| Total (patients) | 1184 | 1.98 |
Modified from Noto TJ, Johnson LW, Krone R, et al: Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I), Cath Cardiovasc Diagn 24:75-83, 1991; in Uretzky BF, Weinert HH: Cardiac catheterization: concepts, techniques, and applications, Walden, Mass, 1997, Blackwell Science.
Table 1-6 Conditions of Patients at Higher Risk for Complications of Catheterization∗
| Acute myocardial infarction |
| Advanced age (>75 years) |
| Aortic aneurysm |
| Aortic stenosis |
| Congestive heart failure |
| Diabetes |
| Extensive three-vessel coronary artery disease |
| Left ventricular dysfunction (left ventricular ejection fraction <35%) |
| Obesity |
| Prior cerebrovascular accident |
| Renal insufficiency |
| Suspected or known left main coronary stenosis |
| Uncontrolled hypertension |
| Unstable angina |
Catheterization Laboratory Data
Information gathered during the cardiac catheterization can be divided into two categories: hemodynamic (see Chapter 3) and angiographic (see Chapter 4). The term cineangiography describes the x-ray photography of cardiac structures. Use of this term persists even though the images are now stored electronically on digital computer imaging media (e.g., CD-ROM) rather than on cine film. The digital cineangiogram provides anatomic information about the chambers of the heart and the coronary arteries. Hemodynamic information is recorded from catheters inside the heart and consists of pressure measurements, cardiac outputs, and blood oxygen saturation measurements.
Preparation of the Patient
Consent for the Procedure
Consent is obtained by the operator or his or her assistant, usually a physician:
Laboratory Atmosphere: The Patient’s Confidence Builder
In-Laboratory Preparations and the “Time-Out”
Catheterization Suite Preparations
Before the start of the catheterization procedure, the staff performs the following tasks:
The “Time Out”
Who Should Participate in the “Time Out” Process?
The “time out” must involve the entire operative team. At a minimum, this includes active participation by the catheterization laboratory operator, any anesthesia provider, and circulating nurse. Participation with active (out-loud) communication by the other members of the team is required (“I concur” is the proper acknowledgment). In particular, there should be no barrier to anyone speaking up if there is concern about a possible error.
Sterile Preparations
Sterile Field Preparation and Patient Draping
A staff member assigned to assist the physician in the procedure puts on hair and shoe covers and surgical face mask and washes the hands and forearms as a surgical scrub. He or she then puts on a sterile surgical gown and gloves. An equipment stand is prepared in a sterile fashion to hold all the catheters and other equipment to be used during the procedure. At this time, a circulating staff member hands catheters and necessary equipment not included in the sterile catheter laboratory pack to the scrub nurse or technician. A sterile drape is placed over the patient, starting at the patient’s upper chest and extending to the foot, covering the entire examination table.
Preprocedural Assessment
Before the administration of sedative agents, the patient should have a complete assessment of his or her current physical condition. The clinician should pay particular attention to any preexisting conditions that would put the patient at risk for an adverse outcome if sedatives are administered. A preprocedural evaluation should include a review of the major organ systems, the time and type of the last oral intake, a history of drug and alcohol use, a history of smoking, and a history of previous experience with sedative agents.
American Society of Anesthesiologists Physical Status Classification
The American Society of Anesthesiologists Physical Status Classification (Table 1-7) is helpful in determining the patient’s eligibility for conscious sedation. It uses a 1 to 5 classification range, with 1 being a healthy patient and 5 being a moribund patient. Procedural sedation is appropriate for patients in Classes 1, 2, and 3. Patients in classes 4 and higher are better suited for general anesthesia. There are several contraindications to conscious sedation (CS) that include the following:
Table 1-7 American Society of Anesthesiologists Physical Status Classification
| Class | Description |
|---|---|
| 1 | A healthy patient (e.g., varicose veins in an otherwise healthy patient) |
| 2 | A patient with mild systemic disease that in no way interferes with normal activity (e.g., controlled hypertension, controlled diabetes, chronic bronchitis) |
| 3 | A patient with severe systemic disease that is not incapacitating (e.g., insulin-dependent diabetes, angina, pulmonary insufficiency) |
| 4 | A patient with severe systemic disease that is a constant threat to life (e.g., cardiac failure, major organ insufficiency) |
| 5 | A moribund patient who is not expected to survive for 24 hours with or without surgery (e.g., intracranial hemorrhage in coma) |
Monitoring Parameters
Level of Consciousness
The patient’s level of consciousness should be assessed often before and during the procedure. The level of consciousness can be assessed by the patient’s response to verbal commands or to light tactile stimulation. Once aroused, the patient should respond appropriately to verbal commands. The nurse or operator can assess this easily by periodically talking to the patient and listening to his or her response. When the patient’s only response is reflex withdrawal from painful stimuli, deep sedation is evident, and special care must be taken to ensure patency of the airway, proper ventilation, and hemodynamic stability.



