48 Interventional Approaches for Peripheral Arterial Disease
Cerebrovascular and Cardioembolic Disease
Carotid Artery Stenosis
More than 600,000 strokes occur annually in the United States, and disability as a consequence of stroke is estimated to affect more than 1 million Americans. An important cause of preventable stroke is large-vessel or carotid atherosclerosis. The risks and therapies for carotid atherosclerosis have been examined in a number of clinical trials. The Asymptomatic Carotid Atherosclerosis Study reported a 5-year risk of stroke ipsilateral to an asymptomatic carotid artery stenosis (of 60% or greater) to be approximately 11%, despite aspirin therapy. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) demonstrated a 2-year stroke risk of 26% in the presence of a previous transient ischemic attack (TIA) or stroke. Both trials reported significant reductions in stroke with carotid endarterectomy (CEA) (see Chapter 49). The perioperative death and stroke risks of CEA approximate 2% and 6% in asymptomatic and symptomatic carotid disease, respectively. However, the advancement of technology and the desire for developing a less morbid and minimally invasive approach to this disease have led to consideration of percutaneous approaches for the treatment of carotid artery stenosis.
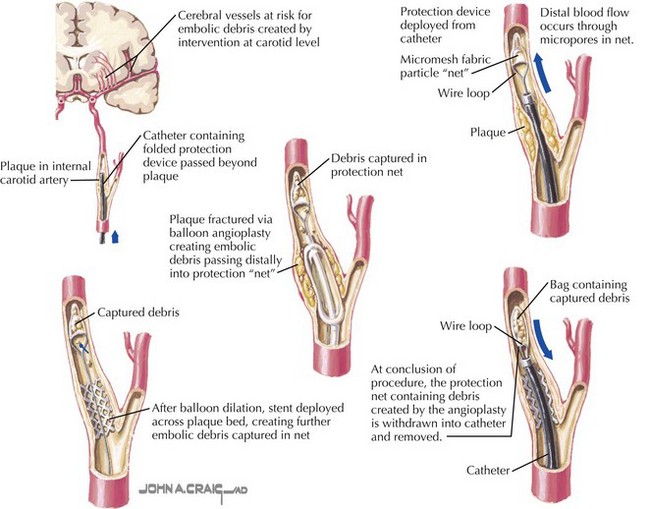
The Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS) was the first randomized trial to establish the general equivalency of endovascular therapy for carotid stenosis. The 3-year death and stroke rates in the predominantly balloon angioplasty group (only 24% received stents) were similar to those in the CEA group. The tradeoff was a higher rate of incidentally detected restenosis: 18% in the balloon angioplasty group compared with 5% for CEA. Since CAVATAS, improvements in the technology available for percutaneous carotid artery revascularization have reduced procedural risks and improved outcomes. In particular, the development and improvements in devices to protect against embolization represent an important step toward improving outcomes in carotid artery stenting (Fig. 48-1). The Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Study demonstrated that carotid stenting in conjunction with cerebral emboli protection was comparable (using “noninferiority” as an end point) with CEA in high-risk patients. Indeed, at 30 days, the primary composite end point of death, stroke, or myocardial infarction was higher in the CEA group than in the stented group (12.6% vs. 5.8%, P < 0.05). The Carotid Revascularization Endarterectomy vs. Stenting Trial (CREST), which has completed enrollment of 2500 patients, will be the largest randomized controlled study comparing stenting and CEA. The results of CREST will address a multitude of issues still being debated and, hopefully, will allow health care providers and patients to better inform their decisions on revascularization for carotid artery stenoses.
Cardioembolic Stroke
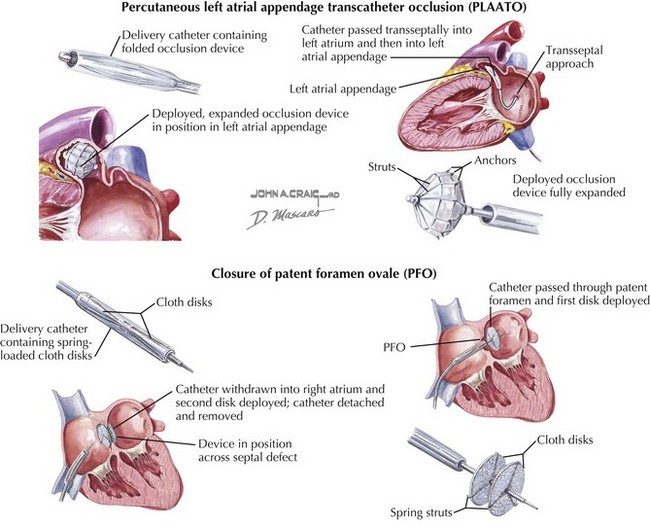
As many as 120,000 strokes per year are attributed to atrial fibrillation. In people 80 years of age and older, atrial fibrillation accounts for nearly 40% of strokes. Although the efficacy of long-term warfarin therapy is established for stroke prevention, a significant number of individuals have contraindications to or complications with anticoagulation or have breakthrough events despite therapeutic concentrations of warfarin. Emerging nonpharmacologic options have focused on maintaining sinus rhythm and include percutaneous ablation of arrhythmogenic atrial foci, implantable atrial defibrillators, and percutaneous left atrial appendage transcatheter occlusion (Fig. 48-2, upper).
In younger people (under 55 years of age), causes of stroke are more variable and approximately 40% of strokes are of undetermined origin. It has been proposed that venous-to-systemic (or paradoxical) embolization through a patent foramen ovale (PFO) may account for a significant number of these cryptogenic strokes. Evidence in support of this hypothesis includes the finding that the 4-year risk of idiopathic recurrent stroke or TIA in patients found to have a PFO is estimated to be 2% to 15%, even with anticoagulation therapy, whereas the risk is virtually none after surgical closure of the PFO. Features that predispose patients with PFO to neurologic events are concurrent atrial septal aneurysm, hypercoagulable states, fat or air embolism (e.g., during or following orthopedic surgery or at parturition), and conditions that increase right atrial pressures (e.g., chronic obstructive pulmonary disease, recurrent pulmonary embolism). Other high-risk markers for subsequent stroke include previous TIA or stroke, large PFO, and higher transatrial bubble counts on echocardiography. Low rates of stroke recurrence have been observed in relatively large case series with transvenous PFO closure devices (Fig. 48-2, lower), and randomized controlled trials comparing this strategy to anticoagulation therapy are in progress.