Interstitial Pattern, Hyperinflation
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Emphysema with Superimposed Process
Asthma
Viral or Atypical Pneumonia
Less Common
Cystic Fibrosis (Mimic)
Sarcoidosis
Rare but Important
Lymphangiomyomatosis
Pulmonary Langerhans Cell Histiocytosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Age, gender, and clinical presentation are key discriminators
Helpful Clues for Common Diagnoses
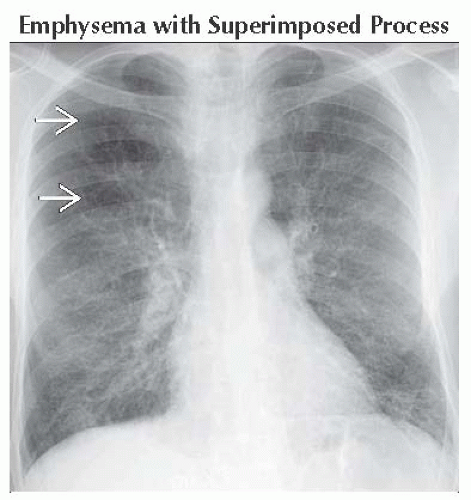
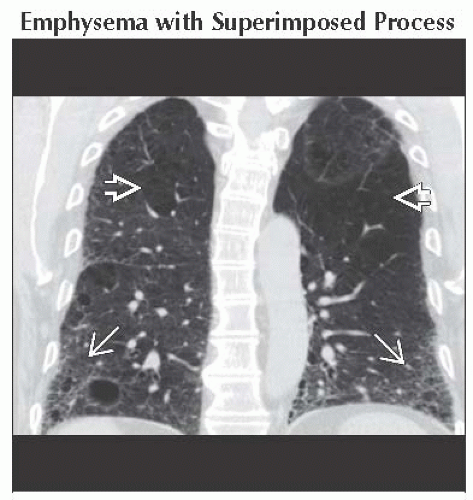
Emphysema with Superimposed Process
Chronic bronchitis with bronchial wall thickening
Pulmonary edema
Pneumonia involving interstitium
Interstitial lung disease
Usual interstitial pneumonia
Desquamative interstitial pneumonia
Respiratory bronchiolitis
Asthma
Normal radiograph is most common radiographic manifestation during acute attack
Radiographic findings slightly more common and more severe in children
Secondary to smaller diameter of bronchioles
Radiographs show
Hyperinflated lungs
Areas of atelectasis secondary to mucus plugging of small airways
Bronchial wall thickening
HRCT demonstrates
Bronchial wall thickening
Mosaic perfusion and air-trapping on expiratory images
Mucous plugging
May be complicated by allergic bronchopulmonary aspergillosis
Viral or Atypical Pneumonia
Discriminators are age and symptoms of infection
Causes hyperinflation in small children secondary to
Poorly developed collateral ventilation
Small airway diameter that easily plugs with mucus
More abundant mucus production
Less frequent to see hyperinflation in adults
Interstitial abnormality secondary to
Inflammation of small airways
Peribronchial edema
Radiographic findings (more common in children)
Course markings radiating from hila into lungs (busy or dirty lungs)
Hyperinflation
Subsegmental atelectasis
Helpful Clues for Less Common Diagnoses
Cystic Fibrosis (Mimic)
Common autosomal recessive disease
Causes recurrent infections in children
Early radiographic findings
Hyperinflation secondary to obstruction of small airways
Nodular or reticular opacities secondary to impaction of small airways
Tram-tracking indicating bronchial wall thickening or bronchiectasis
Upper lung predominant disease
Late radiographic findings
Pulmonary hypertension
Cystic bronchiectasis with more diffuse distribution
Mucoid impaction of larger airways
Atelectasis
HRCT findings
Bronchiectasis
Bronchial wall thickening
Tree-in-bud opacities secondary to mucoid impaction of small airways which ± indicate infection
Mucous plugging of larger airways
Mosaic perfusion and air-trapping on expiratory views indicates small airways involvement
Sarcoidosis
Systemic granulomatous disease
May involve almost any organ
90% have pulmonary involvement
Radiographs demonstrate
Hilar and right paratracheal lymphadenopathy ± calcification
Well- or ill-defined nodules with upper lung predominance
Lungs may be hyperinflated secondary to small airways involvement by noncaseating granulomas
HRCT findings
Upper lung predominance
Perilymphatic distribution of nodules (along fissures, subpleural lung, and bronchovascular bundles)
Uncommonly a random distribution of nodules
Nodular bronchial wall thickening
Small airways involvement demonstrated by mosaic perfusion or air-trapping
Helpful Clues for Rare Diagnoses
Lymphangiomyomatosis
Exclusively women of childbearing age
May exacerbate during pregnancy
Identical disease can be seen in tuberous sclerosis
Radiographic findings
Normal or large lungs
Normal radiograph early
Fine or coarse reticular opacities with diffuse distribution
Pneumothorax (up to 80%)
Pleural effusions (chylous)
HRCT findings
Diffuse distribution of round cysts
Cysts start small and increase in size with disease progression
± chylous pleural effusions (indistinguishable from simple pleural fluid)
± pneumothorax
10-15% have angiomyolipomas in kidneys
± mediastinal or retroperitoneal lymphadenopathy
Pulmonary Langerhans Cell Histiocytosis
20-40-year-old male Caucasian cigarette smoker presenting with cough and dyspnea
Peribronchiolar proliferation of Langerhans cells
Radiographic findings
Nodular or reticulonodular opacities in upper 2/3 of lung
Preserved or increased lung volumes
Spares lung bases
30% have pneumothoraces
HRCT findings
Centrilobular nodules ± central cavities
Cystic spaces ≤ 10 mm in diameter
Round or bizarrely shaped cysts
Spares costophrenic sulci
± pneumothorax
Rare association with lytic bone lesions
Disease progresses from nodules to cavitating nodules to cysts
Cysts thought to represent enlarged airway lumina (paracicatricial emphysema)
Image Gallery
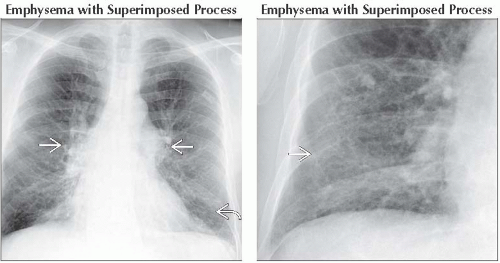 (Left) Frontal radiograph shows hyperinflated lungs and distended central pulmonary arteries
 , consistent with pulmonary arterial hypertension due to chronic hypoxia. Streaky opacities at the bases likely represent bronchial wall thickening , consistent with pulmonary arterial hypertension due to chronic hypoxia. Streaky opacities at the bases likely represent bronchial wall thickening  . (Right) Frontal radiograph shows emphysema complicated by DIP. Note slight increase in interstitial opacities in the lung bases . (Right) Frontal radiograph shows emphysema complicated by DIP. Note slight increase in interstitial opacities in the lung bases  from the chronic inflammation associated with smoking cigarettes. from the chronic inflammation associated with smoking cigarettes.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|