14 Intermittent Positive-Pressure Breathing
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE)
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will simply be shown as: (Code: …). If an item is only testable on the ELE, it will be shown as: (ELE code: …). If an item is only testable on the WRE, it will be shown as: (WRE code: …).
MODULE A
1. Description
Shapiro and associates (1991) list the following as the physiologic effects of IPPB:
a. Increased mean airway pressure
By definition of IPPB, the patient is receiving a positive airway pressure instead of generating a negative intrathoracic pressure to create the VT. Most authors recommend that patients with heart disease be monitored closely for the effects of increased mean airway pressure. Decreasing the normal return of venous blood to the heart, thereby decreasing the cardiac output, is possible. Shapiro and associates (1991) recommend an expiratory time that is long enough to allow for normal venous return before the next positive-pressure breath is given. The patient’s heart rate and blood pressure can be monitored to ensure that they stay in the normal range.
d. Alteration of the inspiratory/expiratory ratio
Patients with high airway resistance or low lung compliance often change their breathing patterns to reduce the WOB (see Chapter 1). These new breathing patterns may lead to worsening of the patient’s condition. Alteration of normal ventilation and perfusion ratios in the lungs may worsen hypoxemia. Properly administered and coached IPPB can be used to adjust the inspiratory/expiratory (I:E) ratio to the benefit of the patient. The patient can be taught how to breathe in a more physiologically normal pattern.
2. Indications
The following indications and guidelines are listed in the American Association for Respiratory Care (AARC) Clinical Practice Guidelines (1991, 2003) on IPPB:
a. To treat atelectasis when other deep breathing methods are ineffective
Patients who are uncooperative, unconscious, or physically incapable of being coached in deep-breathing and coughing techniques or in performing incentive spirometry (IS) may be helped by IPPB. An inspiratory pause at the end of the IPPB breath helps to better distribute the gas to open areas of atelectasis. As has been discussed in Chapter 7, a patient would benefit from IPPB rather than IS if any of the following apply:
c. To enhance the patient’s cough effort and sputum clearance
The following additional indications were listed in the Guidelines for the Use of Intermittent Positive Pressure Breathing (IPPB) published by the Respiratory Care Committee of the American Thoracic Society (1980).
d. To treat impending ventilatory failure as seen by an increased arterial carbon dioxide partial pressure (PaCO2)
It may be possible to delay or avoid intubation and mechanical ventilation in the deteriorating chronic obstructive pulmonary disease (COPD) patient. The patient is able to relax and reduce the work of breathing (WOB) during a passive IPPB treatment. It may be necessary to give IPPB for 5 to 10 minutes as often as every 30 minutes to 1 hour. The treatment should also be given with the intention of helping the patient’s cough and sputum clearance. (An alternative to frequent IPPB treatments is noninvasive positive-pressure ventilation. This is discussed in Chapter 15.)
e. To help manage the patient with acute pulmonary edema
IPPB can help in the management of this patient by temporarily increasing mean airway pressure. This reduces the venous return to the heart, which may reduce pulmonary edema. The IPPB procedure does not correct the underlying cardiac problem, which must be treated by other means.
f. To induce a sputum sample for culture and sensitivity or other diagnostic studies
Inducing a sputum sample by IPPB is indicated only if simpler methods have failed.
4. Hazards and precautions
The AARC guidelines list the following hazards and precautions for IPPB therapy:
5. Initiation of therapy
a. Steps in the basic procedure
c. Giving an active treatment
Welch and colleagues (1980) have found that the patient’s posttreatment IC is greatest when the practitioner (1) uses as high a peak pressure as the patient can tolerate and (2) coaches the patient to inhale as deeply as possible with the IPPB machine. They and others believe that this is the best way to treat or prevent atelectasis. Monitor the patient for signs of barotrauma/volutrauma.
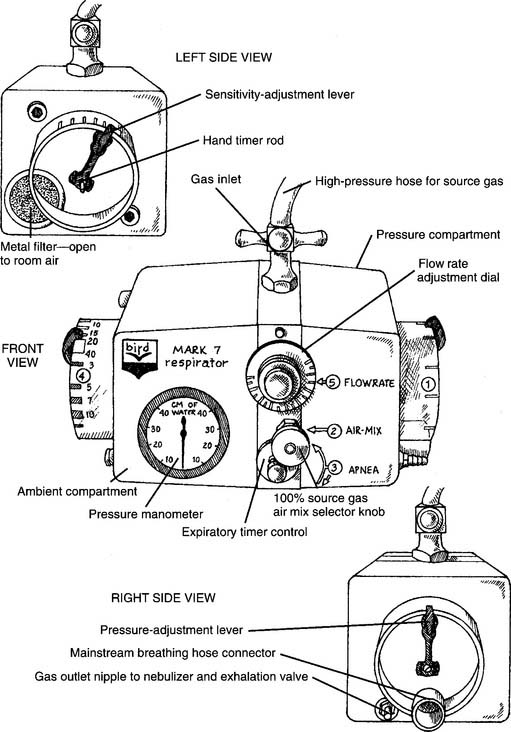
6. Initial settings on the Bird Mark 7
The older version of the Mark 7 is used as the model respirator of the Bird series. The current Mark 8 has similar features. Other Bird units have slightly different controls and features. Refer to Figure 14-1 for the following:
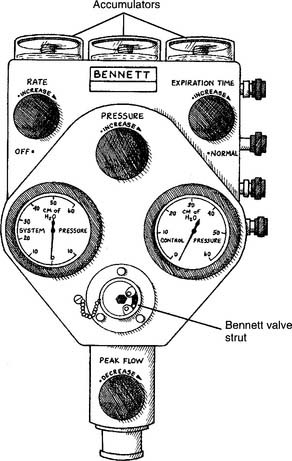
7. Initial settings on the Bennett PR-2
The PR-2 is used as the model respirator of the Bennett series. (Although the PR-2 is no longer being manufactured, many are still in clinical use.) Other Bennett units have slightly different controls and features. Refer to Figures 14-2 and 14-3 for the following:
MODULE B
1. Change the patient-machine interface
a. Mouthpiece
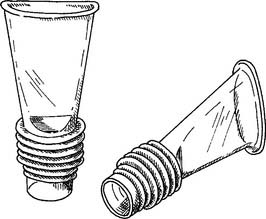
A conscious, cooperative patient can take a treatment with a mouthpiece. He or she must be instructed to place the mouthpiece between the teeth (or gums) and seal the lips around it so that there is no leak. Instruct the patient to sip gently on it to turn on the IPPB machine. As long as the lips are sealed and there are no other leaks, the positive-pressure breath will stop when the preset pressure is reached. Nose clips are often helpful to prevent a leak through the nose as the patient is learning how to take the treatment. The nose clips can be removed after the patient has learned how to seal the nasopharynx with the soft palate.
A variety of mouthpieces are available. All share two common features: a raised edge so that the teeth do not slip off; and a 22-mm outer diameter (OD) connector end to insert into the IPPB circuit (Figure 14-4).
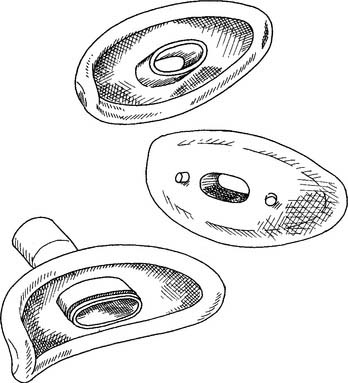
b. Mouth seal (Bennett seal)
An unconscious, uncooperative, or aged patient who cannot seal his or her lips can be aided by placing a soft rubber seal around the mouthpiece. The practitioner gently holds the seal around the patient’s lips to seal the airway so that the patient can trigger the breath and cycle the machine off (Figure 14-5). Nose clips are also commonly needed.