Interlobular Septal Thickening
Jonathan H. Chung, MD
DIFFERENTIAL DIAGNOSIS
Common
Cardiogenic Pulmonary Edema
Lymphangitic Carcinomatosis
Sarcoidosis
Usual Interstitial Pneumonitis
Less Common
Pulmonary Vein Stenosis
Pulmonary Alveolar Proteinosis
Venoocclusive Disease
Alveolar Septal Amyloidosis
Rare but Important
Erdheim Chester Disease
Leukemic Infiltration
Diffuse Pulmonary Lymphangiomatosis
Acute Eosinophilic Pneumonia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Most often due to pulmonary edema or lymphangitic carcinomatosis
Smooth thickening
Cardiogenic pulmonary edema
Lymphangitic carcinomatosis
Nodular or irregular thickening
Lymphangitic carcinomatosis or sarcoidosis
Helpful Clues for Common Diagnoses
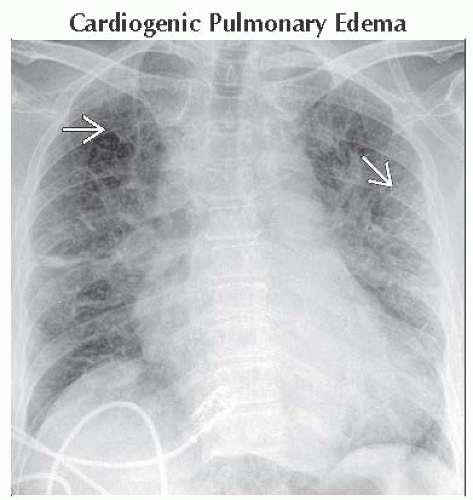
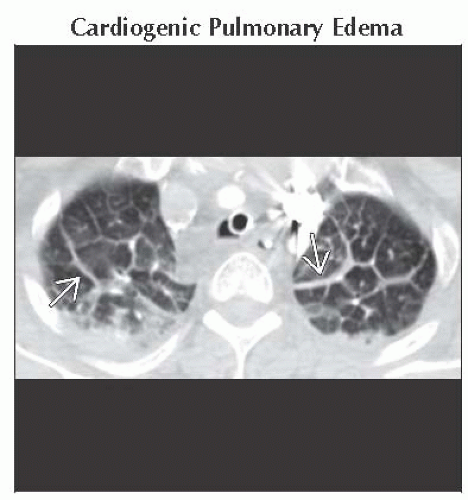
Cardiogenic Pulmonary Edema
Due to imbalances in Starling forces: Usually due to increased pulmonary venous pressure
Left-sided heart failure (myocardial infarct or ischemic cardiomyopathy)
Fluid overload or renal failure
Mitral valvular disease
Interlobular septal thickening; Kerley B and Kerley A lines on chest radiograph
Diffuse hazy, air-space opacities
Characteristically central predominant due to higher concentration of lymphatics in peripheral aspect of lungs
Cardiomegaly
Signs of coronary artery disease (coronary artery calcification, CABG, coronary artery stents, subendocardial fatty metaplasia)
Lymphangitic Carcinomatosis
Most common with primary lung adenocarcinoma
Also breast, stomach, pancreas adenocarcinoma
Asymmetric nodular (beaded) or smooth interlobular septal thickening
Peribronchial and peribronchovascular thickening
Pleural effusion and hilar/mediastinal lymphadenopathy common
Sarcoidosis
Upper and mid lung, small perilymphatic nodules (along interlobular septa, subpleural, peribronchovascular)
Subcentimeter centrilobular nodules
Air-trapping
Nodular interlobular septal thickening
Symmetric hilar and mediastinal lymphadenopathy; ± calcification
Perilymphatic nodules may coalesce into focal nodular consolidation or foci of ground-glass opacity
Low-density lesions in spleen and liver; hepatosplenomegaly, upper abdominal lymphadenopathy
Usual Interstitial Pneumonitis
Interlobular and intralobular septal thickening predominate in peripheral and basilar aspects of lungs
Costophrenic angles most severely affected
Traction bronchiectasis, honeycombing, and architectural distortion
Mild mediastinal lymphadenopathy not uncommon
Helpful Clues for Less Common Diagnoses
Pulmonary Vein Stenosis
Multiple etiologies
Extrinsic compression or invasion of pulmonary vein, thrombosis of pulmonary vein, post ablation stenosis
Asymmetric interlobular septal thickening, peribronchial thickening, and peribronchovascular thickening
In distribution of affected pulmonary vein
Ipsilateral pleural effusion
Pulmonary Alveolar Proteinosis
Diffuse or patchy airspace opacities often with geographic distribution
Interlobular and intralobular septal thickening common
Most often idiopathic
Much less often secondary to hematological malignancy, massive silica inhalation, drugs, infection, or congenital causes
Venoocclusive Disease
Rare cause of pulmonary arterial hypertension
Pulmonary arterial dilation
Smooth or nodular interlobular septal thickening
Centrilobular ground-glass nodules
Pericardial and pleural effusions
Alveolar Septal Amyloidosis
Respiratory involvement in amyloidosis common though respiratory symptoms uncommon
Alveolar septal subtype of amyloidosis least common
Interlobular and intralobular septal thickening with micronodules (often in subpleural distribution)
Affected areas may calcify; ossification less common
Helpful Clues for Rare Diagnoses
Erdheim Chester Disease
Non-Langerhans cell histiocytosis primarily involving long bones; up to 1/3 have pulmonary involvement
Smooth interlobular septal thickening
Smooth pleural thickening or pleural effusions
Soft tissue encasement of aorta, great vessels, and kidneys
Bilateral symmetric osteosclerosis of metaphyses and diaphyses of long bone
Leukemic Infiltration
History of leukemia
Asymmetric or symmetric interlobular septal thickening, may be nodular
Peribronchial and peribronchovascular thickening
Patchy, multifocal airspace opacities
Intrathoracic lymphadenopathy common
Diffuse Pulmonary Lymphangiomatosis
Congenital proliferation and dilatation of lymphatics
Diffuse interlobular septal and peribronchial thickening
Extensive infiltration of mediastinal fat
Pleural or pericardial effusions
Mild mediastinal lymphadenopathy
Acute Eosinophilic Pneumonia
Probable hypersensitivity reaction to inhaled agents; possible association with smoking
Imaging mimics pulmonary edema
Ground-glass opacities > consolidation
Interlobular septal thickening
Pleural effusions
Acute high fever, profound dyspnea, myalgia, pleuritic chest pain
Responds rapidly to corticosteroids
Image Gallery