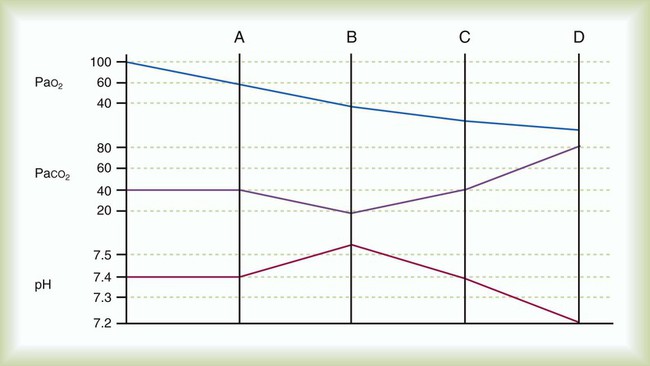
After reading this chapter you will be able to: The goals of mechanical ventilatory support are to maintain adequate alveolar ventilation and oxygen (O2) delivery, restore acid-base balance, and reduce the work of breathing (WOB) with minimum harmful side effects and complications.1 Mechanical ventilation also may reduce increased myocardial work secondary to hypoxemia and an increased WOB.1 Other physiologic objectives of mechanical ventilatory support include increasing or maintaining lung volume with positive end expiratory pressure (PEEP) and continuous positive airway pressure (CPAP) for promotion, improvement, or maintenance of lung recruitment.1 A lung protective ventilatory strategy is an approach to mechanical ventilation that includes the use of small tidal volume (VT) and appropriate levels of PEEP.2 This approach is usually employed in patients with acute lung injury (ALI) or the acute respiratory distress syndrome (ARDS). However, the concept of lung protection should be applied to all patients requiring ventilatory support for acute respiratory failure. Lung injury is primarily caused by an elevated transpulmonary pressure during positive pressure ventilation.3 Transpulmonary pressure is the difference between alveolar pressure and pleural pressure. A safe transpulmonary pressure during mechanical ventilation is not firmly established, but most clinicians would agree that the lower the transpulmonary pressure, the less likely the development of ventilator-induced lung injury.4 High transpulmonary pressures are associated with alveolar overdistention and lung injury.3 Plateau pressure (Pplat), the end inspiratory equilibration pressure, measures the mean peak alveolar pressure and is the best bedside clinical reflection of transpulmonary pressure.2,4,5 Although Pplat is not an accurate measurement of transpulmonary pressure, the transpulmonary pressure never exceeds the Pplat.4 Pplat provides an excellent bedside assessment of the level of potentially dangerous ventilating pressure. Limiting Pplat reduces the likelihood of ventilator-induced lung injury. Generally, the lower the Pplat, the better the patient outcome.2,5 Ideally, Pplat should be less than 30 cm H2O.5 However, a Pplat greater than 30 cm H2O may be applied in patients with a decreased thoracic compliance without resulting in overdistention5 because a decrease in chest wall compliance (obesity, massive fluid resuscitation, abdominal distention, elevated bladder pressure) increases the pleural pressure, decreasing the transpulmonary pressure. Generally, the lowest possible Pplat is maintained by selecting a VT of 4 to 8 ml/kg of ideal body weight (IBW). The higher the Pplat, the smaller the VT should be. Generally, VT greater than 10 ml/kg IBW is never indicated in critically ill patients. Lung injury can also be caused by repetitive opening and closing of unstable lung units.6 The application of an appropriate level of PEEP ensures that unstable lung units are maintained in the open position reducing the likelihood of additional lung injury. Specific clinical objectives of mechanical ventilation include reversal of hypoxemia, hypercapnia, and associated respiratory acidosis and prevention or reversal of ventilatory muscle dysfunction. The general trajectory of pH, PCO2, and PO2 during the progression of acute respiratory failure is depicted in Figure 44-1. Mechanical ventilation may be used to allow sedation or paralysis for certain procedures, to decrease myocardial and ventilatory muscle O2 consumption to maximize O2 delivery to the tissues, to decrease intracranial pressure acutely in the presence of closed head injury or cerebral edema (by reducing PaCO2 to 25 to 30 mm Hg for a short period and promoting cerebral vasoconstriction), to prevent or reverse atelectasis, and to stabilize the chest wall in the case of a massive flail or chest wall resection. Table 44-1 lists the most common causes of acute respiratory failure leading to ventilatory support in the United States and Canada. Hazards of mechanical ventilation include decreased venous return and cardiac output, patient-ventilatory asynchrony, and ventilatory muscle dysfunction owing to inappropriate ventilator settings, ventilator-associated pneumonia, and ventilator-induced lung injury.1 Box 44-1 lists the goals of ventilatory support, and Box 44-2 lists specific objectives of mechanical ventilation. TABLE 44-1 Modified form Esteban A, Anzueto A, Alia I, et al: How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 161:1450, 2000. When the decision to begin mechanical ventilatory support is made, one must choose the mode of ventilation, select an appropriate device, and establish the initial ventilator settings. In the selection of initial ventilator settings, the goal is to optimize the patient’s oxygenation, ventilation, and acid-base balance, while avoiding harmful side effects. This goal is achieved by choosing an appropriate mode of ventilation, fractional inspired oxygen (FiO2), VT (volume ventilation) or pressure level (pressure ventilation), rate, peak flow and flow waveform, inspiratory time, and PEEP level. Appropriate trigger sensitivity, pressure limit, alarms, backup ventilation, and humidification must be selected. After initial ventilator setup, adjustments must be made on the basis of the patient’s response and the patient-specific clinical objectives of ventilatory support. Most patients who need mechanical ventilatory support receive invasive positive pressure ventilation; however, an increasing number of patients are being ventilated noninvasively (see Chapter 46). Next, the clinician must choose the mode of ventilation (e.g., volume assist/control [VA/C], pressure assist/control [PA/C], pressure support ventilation [PSV], pressure regulated volume control [PRVC], volume support, adaptive support ventilation, proportional assist ventilation [PAV], or neurally adjusted ventilatory assist [NAVA]) and initial ventilator settings (e.g., rate, VT or pressure level, FiO2, PEEP). Finally, the clinician must choose appropriate alarm and apnea settings. Box 44-3 summarizes key decisions that must be made as a part of initial ventilator setup. Although more than 75% to 80% of all patients receiving ventilatory assistance receive it invasively, the use of noninvasive ventilation should be considered in select patients requiring ventilatory assistance. Noninvasive ventilation is preferred in some patients because the outcomes are better. Chapter 46 provides details on all aspects on noninvasive ventilation. Conventional mechanical ventilatory support requires the establishment of an artificial airway. Initially, nearly 100% of patients receiving positive pressure ventilation are intubated, and of these, 99% have oral endotracheal tubes, and only about 1% are intubated nasally.7 Approximately 5% to 10% of patients receiving mechanical ventilation have a tracheotomy performed at some point.7 Airway management is described in detail in Chapter 33. The next decision to be made regarding initiation of mechanical ventilation is whether to use a primarily pressure-targeted or volume-targeted mode of ventilation. Volume-targeted ventilation essentially includes VA/C and synchronized intermittent mandatory ventilation (SIMV). Pressure ventilation includes PA/C, SIMV, PRVC, volume support, and airway pressure release ventilation. In addition, the clinician can select the patient controlled modes PAV or NAVA. However, most patients are initially ventilated with pressure or volume forms of ventilation. The operational capabilities of these modes are described in detail in Chapter 42, and the indications, benefits, and concerns regarding these modes are discussed in Chapter 43. Full ventilatory support can be defined as the application of mechanical support such that all or most of the energy necessary for effective alveolar ventilation is provided by the ventilator.8 When a ventilator is set to deliver full ventilatory support, the patient is either passive or simply triggers the breath to initiate inspiration allowing the ventilator to perform most of the work of breathing. However, it is very difficult to set the ventilator to assume all of the work of breathing without significantly sedating the patient. In most patient-triggered approaches to ventilatory support, patient-ventilatory synchrony is a major issue, and very careful titration of the ventilator settings is necessary to ensure synchrony and minimize patient WOB. Patient-ventilatory synchrony is discussed in detail later in the chapter. Partial ventilatory support implies that only a percentage of the WOB is provided by the ventilator.8 Normally, when partial ventilatory support is indicated, SIMV, PSV, volume support, PAV, and NAVA are the modes of choice. However, as with full ventilatory support, care in setting the ventilatory is critical to ensure that patient-ventilator synchrony is maximized. Partial ventilatory support strategies minimize the loss of ventilatory muscle function, require less sedation, assist in recruiting and stabilizing alveolar units, and generally move patients closer to ventilator discontinuance than full ventilatory support approaches. Assist-control ventilation can be delivered in either pressure-targeted or volume-targeted ventilation. Suggested initial settings for assist-control volume ventilation in the care of adults are listed in Box 44-4. Advantages of assist-control volume ventilation include the assurance that a minimum safe level of ventilation is achieved, yet the patient can still set his or her own breathing rate. In the event of sedation or apnea, a minimum safe level of ventilation is guaranteed by the selection of an appropriate backup rate, usually approximately 4 to 6 breaths/min less than the patient’s assist rate but not less than the rate necessary to provide a minimum safe level of ventilation (e.g., a backup rate of at least 12 to 14 breaths/min).8 Because assist-control ventilation usually provides full ventilatory support, it may result in less WOB than partial support modes. However, less WOB should not be assumed just because the patient is in assist-control ventilation. Trigger work may be significant if inappropriate sensitivity settings are selected. In addition, when a breath is triggered, inspiratory muscle activity persists.9,10 If the inspiratory flow rate during volume ventilation does not meet or exceed the patient’s inspiratory demand, or inspiratory time is too lengthy, the patient’s WOB may be greater, equaling or exceeding the work of a spontaneous unassisted breath.9,10 In pressure ventilation, lengthy inspiratory times, inadequate rise time, and improperly set pressure levels can also cause asynchrony. (See later sections focusing on patient-ventilator synchrony.) If properly applied and tolerated by the patient, assist-control ventilation may provide ventilatory muscle rest that allows the ventilatory muscles to recover from ventilatory muscle dysfunction. Disadvantages of assist-control mode include an increase in WOB.8,11 Assist control also may be poorly tolerated by awake, nonsedated patients. The patient may fight the ventilator, or asynchronous patient-to-ventilator breathing patterns may develop. Because flow is based on patient demand in pressure-targeted ventilation, synchrony is generally better achieved during PA/C than with VA/C ventilation. Advantages and disadvantages of pressure-controlled ventilation (PCV) are described in Box 44-5. Assist-control volume ventilation is the most common ventilator mode used throughout the world as the primary initial mode of ventilatory support.7,12 Regardless of the indication for ventilatory support or underlying disease, this mode is able when properly adjusted and the patient is properly managed to provide adequate ventilatory support for all indications for ventilatory support.6,12 Controlled ventilation, pressure, or volume is achieved using the assist-control mode when the patient is apneic because of a medical condition, anesthesia, or use of sedative drugs and paralytic agents. Ventilators in use today do not prevent a patient with sufficient effort from triggering the ventilator, a situation always to be avoided. Controlled ventilation can be achieved only with pharmacologic agents. Advantages of controlled ventilation include eliminating WOB and complete control over the patient’s ventilatory pattern. In cases in which WOB is high, controlled ventilation may allow for ventilatory muscle rest, reduce O2 consumption of the ventilatory muscles, and “free up” O2 for delivery to the tissues.8 Controlled ventilation is a common initial approach in situations of severe acute respiratory failure especially if the primary problem is hypoxemia. Figure 44-2 depicts the effects of inspiratory time on VT
Initiating and Adjusting Invasive Ventilatory Support
 Discuss the goals of ventilatory support.
Discuss the goals of ventilatory support.
 Describe how to choose an appropriate ventilator to begin ventilatory support.
Describe how to choose an appropriate ventilator to begin ventilatory support.
 Explain how to select an appropriate mode of ventilation given a patient’s specific condition and ventilatory requirements.
Explain how to select an appropriate mode of ventilation given a patient’s specific condition and ventilatory requirements.
 Choose appropriate initial ventilator settings, based on patient assessment.
Choose appropriate initial ventilator settings, based on patient assessment.
 Describe how to assess a patient after initiation of ventilation.
Describe how to assess a patient after initiation of ventilation.
 Discuss how to adjust ventilatory support based on oxygenation and ventilation status.
Discuss how to adjust ventilatory support based on oxygenation and ventilation status.
 Discuss how to ventilate using the concept of lung protective ventilation.
Discuss how to ventilate using the concept of lung protective ventilation.
 Discuss asynchrony and how ventilator adjustments in pressure and volume ventilation improve asynchrony.
Discuss asynchrony and how ventilator adjustments in pressure and volume ventilation improve asynchrony.
 Explain how to adjust the ventilator on the basis of the patient’s response.
Explain how to adjust the ventilator on the basis of the patient’s response.
Goals of Mechanical Ventilation
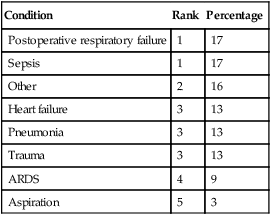
Condition
Rank
Percentage
Postoperative respiratory failure
1
17
Sepsis
1
17
Other
2
16
Heart failure
3
13
Pneumonia
3
13
Trauma
3
13
ARDS
4
9
Aspiration
5
3
Ventilator Initiation
Noninvasive Ventilation
Establishment of the Airway
Pressure-Controlled versus Volume-Controlled Ventilation
Full Ventilatory Support versus Partial Ventilatory Support
Initial Ventilator Settings
Choice of Mode
Assist-Control Ventilation (Patient-Triggered or Time-Triggered Continuous Mandatory Ventilation)
Controlled Ventilation (Time-Triggered Continuous Mandatory Ventilation)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Initiating and Adjusting Invasive Ventilatory Support