This study was conducted to investigate the prognostic value of heart block among patients with acute myocardial infarction (AMI) treated with drug-eluting stents. A total of 13,862 patients with AMI, registered in the nation-wide AMI database from January 2005 to June 2013, were analyzed. Second- (Mobitz type I or II) and third-degree atrioventricular block were considered as heart block in this study. Thirty-day major adverse cardiac events (MACE) including all causes of death, recurrent myocardial infarction, and revascularization were evaluated. Percutaneous coronary intervention with implantation of drug-eluting stent was performed in 89.8% of the patients. Heart block occurred in 378 patients (2.7%). Thirty-day MACE occurred in 1,144 patients (8.2%). Patients with heart block showed worse clinical parameters at initial admission, and the presence of heart block was associated with 30-day MACE in univariate analyses. However, the prognostic impact of heart block was not significant after adjustment of potential confounders (p = 0.489). Among patients with heart block, patients with a culprit in the left anterior descending (LAD) coronary artery had worse clinical outcomes than those of patients with a culprit in the left circumflex or right coronary artery. LAD culprit was a significant risk factor for 30-day MACE even after controlling for confounders (odds ratio 5.28, 95% confidence interval 1.22 to 22.81, p = 0.026). In conclusion, despite differences in clinical parameters at the initial admission, heart block was not an independent risk factor for 30-day MACE in adjusted analyses. However, a LAD culprit was an independent risk factor for 30-day MACE among patients with heart block.
A number of studies have reported that heart block is a common complication of acute myocardial infarction (AMI) and is associated with worse clinical outcomes. However, most of these studies were conducted in the prethrombolytic or thrombolytic era. To date, the prognostic impacts of heart block complicating AMI have not yet been reported in the drug-eluting stent (DES) era. Therefore, the aim of this study was to investigate the clinical outcomes of patients with AMI who developed heart block in the DES era. A large series of patients with AMI from a nation-wide AMI registry in Korea were analyzed in this study. Most of the study patients received DES implantation.
Methods
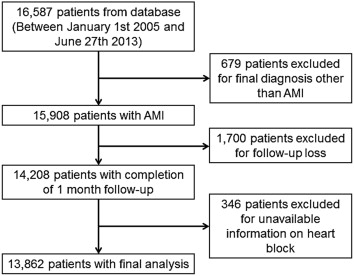
Detailed study methods, including patient enrollment, have been described recently in previous studies. In brief, the Korea Acute Myocardial Infarction Registry and the Korea Working Group on Myocardial Infarction registry were established in November 2005, with support from the Korean Society of Cardiology, for prospective, open, observational, multicenter studies of AMI, including assessment of clinical outcomes. Fifty-five cardiac centers in Korea participated in establishing the database. From January 2005 to June 2013, 16,587 patients with AMI were identified from the Korea Acute Myocardial Infarction Registry and Korea Working Group on Myocardial Infarction database. Of these patients, 679 who had a final diagnosis other than AMI, 1,700 who did not have a clinical follow-up after discharge, and 346 who had no available information on atrioventricular block (AVB) were excluded. Finally, the remaining 13,862 patients were analyzed. The flow chart for patient enrollment is shown in Figure 1 . AMI was diagnosed based on patient’s symptoms, cardiac enzyme elevation, and changes in the electrocardiogram. Demographic and clinical characteristics, including age, gender, body mass index, smoking status, a history of hypertension, dyslipidemia, and ischemic heart disease, were collected prospectively and stored on an electronic database. Systolic and/or diastolic blood pressure and heart rate were checked by trained nurses, and left ventricular (LV) ejection fraction was determined by 2-dimensional echocardiography. The Killip classification was applied based on the presence of heart failure, acute pulmonary edema, and shock at the initial admission. Blood samples for baseline laboratory tests other than lipid measurement were collected at admission before initial treatment. Overnight fasting blood was also sampled for lipid levels. The initial treatment strategy for patients with AMI was determined by the attending physicians based on guideline’s recommendations. Multivessel disease was defined as ≥70% stenosis in at least 2 major epicardial coronary arteries or ≥50% stenosis of the left main coronary artery. Successful percutaneous coronary intervention was defined as residual stenosis of target vessel <50% with Thrombolysis In Myocardial Infarction flow 2 or 3. The study protocol was approved by the institutional review board of each hospital, and informed consents were obtained from all study participants.
Heart block was diagnosed based on standard 12-lead electrocardiographic findings at the time of initial admission. Experienced cardiologists interpreted the electrocardiogram. Second-degree AVB was defined when one or more atrial pulses did not conduct to the ventricle. Third-degree AVB was defined when no atrial activity was conducted to the ventricle, and P waves were completely dissociated with QRS complexes. Second- (Mobitz type I or II) and third-degree AVB were considered as heart block in this study.
Patients were followed up after hospital discharge. The primary outcome of this study was major adverse cardiac events (MACE), including all causes of death, nonfatal myocardial infarction (MI), and revascularization (coronary bypass surgery or percutaneous coronary intervention) within 30 days of AMI. When ≥2 events were recorded at the same hospitalization, the most serious event was considered as the event of the patient in the following order: death, nonfatal MI, and revascularization. Information on MACE was collected by medical record review or telephone interviews if necessary. Only the first MACE was considered as the MACE of a patient. All data were entered in an electronic web-based case-report form.
Data are presented as mean values with SDs or percentages. Continuous variables were compared using the Student t test and categorical variables were compared using the chi-square test. Binary logistic regression analysis was used to control for the influence of several potential confounders and identify independent risk factors of MACE. A 2-tailed p value <0.05 was considered statistically significant. All data were analyzed using SPSS for Windows 18.0 (IBM Co, Armonk, NY).
Results
Of the 13,862 patients in the study cohort, 378 (2.7%) had heart block at the time of initial admission for AMI. The baseline characteristics of the study patients according to the presence of heart block are listed in Table 1 . Patients with heart block were older, more often women, and had more unfavorable clinical factors, including diabetes, hypertension, lower blood pressure, high glucose level, and lesser renal function than those without heart block. As expected, the right coronary artery (RCA) was the culprit artery in most patients with heart block (83.8%), whereas the left anterior descending (LAD) coronary artery was the most frequent culprit site (48.4%) in patients without heart block. Percutaneous coronary intervention with DES was performed in 89.8% of patients. The rate of prescription of β-blocker at discharge was lower in patients with heart block than those without.
| Characteristic | Heart block | ||
|---|---|---|---|
| Yes (n = 378) | No (n = 13,484) | p value | |
| Age (years) | 67.4 ± 11.3 | 63.6 ± 12.7 | < 0.001 |
| Male sex | 237 (62.7%) | 9,516 (70.6%) | 0.001 |
| Body mass index (kg/m 2 ) | 2.39 ± 4.0 | 24.0 ± 3.3 | 0.684 |
| Diabetes mellitus | 133 (35.4%) | 3,760 (28.0%) | 0.002 |
| Hypertension | 218 (58.0%) | 6,560 (48.8%) | < 0.001 |
| Smoker | 193 (51.7%) | 7,843 (58.5%) | 0.009 |
| Systolic blood pressure (mm Hg) | 101 ± 31 | 128 ± 27 | < 0.001 |
| Diastolic blood pressure (mm Hg) | 64.0 ± 17.9 | 78.9 ± 16.2 | < 0.001 |
| Heart rate (per minute) | 55.5 ± 22.0 | 78.4 ± 19.3 | < 0.001 |
| Killip stage ≥ 2 | 201 (54.3%) | 3,495 (26.4%) | < 0.001 |
| Left ventricular ejection fraction (%) | 54.4 ± 10.6 | 52.0 ± 12.4 | 0.001 |
| Maximal CK-MB (ng/mL) | 132 ± 155 | 122 ± 211 | 0.368 |
| Maximal troponin I (ng/mL) | 38.8 ± 39.0 | 32.8 ± 40.1 | 0.011 |
| Total cholesterol (mg/dL) | 167 ± 43 | 182 ± 44 | < 0.001 |
| LDL cholesterol (mg/dL) | 103 ± 36 | 116 ± 37 | < 0.001 |
| HDL cholesterol (mg/dL) | 41.2 ± 11.0 | 43.9 ± 11.9 | < 0.001 |
| Triglyceride (mg/dL) | 123 ± 136 | 127 ± 99 | 0.433 |
| Glucose (mg/dL) | 222 ± 113 | 170 ± 81 | < 0.001 |
| Estimated GFR (mL/min/1.73m 2 ) | 52.1 ± 25.7 | 68.8 ± 29.7 | < 0.001 |
| Culprit coronary artery | < 0.001 | ||
| Left main | 1 (0.3%) | 282 (2.3%) | |
| Left anterior descending | 28 (7.6%) | 5,909 (48.4%) | |
| Left circumflex | 30 (8.4%) | 2,072 (17.0%) | |
| Right | 298 (83.8%) | 3,938 (32.3%) | |
| Three-vessel coronary disease | 97 (26.9%) | 2,759 (21.6%) | 0.016 |
| Lesion type, B2 or C | 279 (83.0%) | 9,331 (80.8%) | 0.306 |
| PCI with DES | 270 (85.2%) | 9,540 (90.1%) | 0.004 |
| Stent number | 1.54 ± 0.84 | 1.55 ± 0.84 | 0.831 |
| Stent diameter (mm) | 3.24 ± 0.45 | 3.17 ± 0.42 | 0.007 |
| Stent length (mm) | 24.6 ± 6.4 | 24.7 ± 6.5 | 0.831 |
| Post-PCI TIMI flow III | 259 (89.6%) | 8,345 (92.2%) | 0.113 |
| PCI success | 275 (93.5%) | 8,780 (96.1%) | 0.028 |
| Discharge medication | |||
| Aspirin | 314 (98.4%) | 12,362 (97.8%) | 0.465 |
| Clopidogrel | 311 (97.5%) | 11,748 (92.9%) | 0.002 |
| Beta-blocker | 227 (71.2%) | 9,835 (77.8%) | 0.005 |
| ACE inhibitor or ARB | 265 (83.1%) | 10,383 (82.1%) | 0.669 |
| Statin | 228 (71.5%) | 9,502 (75.2%) | 0.130 |
Of the 13,862 patients in the study cohort, 1,144 (8.2%) had 30-day MACE. Comparisons of clinical events at 30 days after AMI between patients with and without heart block are listed in Table 2 . Patients with heart block had more MACE than patients without. This difference was mainly attributed to cardiac death.
| Event | Heart block | ||
|---|---|---|---|
| Yes (n = 378) | No (n = 13,484) | p value | |
| Death, non-fatal myocardial infarction and revascularization | 63 (16.7%) | 1,081 (8.0%) | < 0.001 |
| Cardiac death | 52 (13.8%) | 743 (5.5%) | < 0.001 |
| Non-fatal myocardial infarction | 1 (0.3%) | 69 (0.5%) | < 0.001 |
| Percutaneous coronary intervention | 5 (1.3%) | 128 (0.9%) | 0.463 |
| Coronary bypass surgery | 0 | 41 (0.3%) | 0.630 |
The results of a multiple logistic regression analysis showing independent risk factors of 30-day MACE are listed in Table 3 . Male gender, the presence of hypertension, high Killip stage, 3-vessel disease, lesser LV systolic function, and impaired renal function were independent risk factors for 30-day MACE. The presence of heart block was not a risk factor for 30-day MACE in this model (p = 0.489).
| Variable | OR | 95% CI | p value |
|---|---|---|---|
| Age ≥ 65 years | 1.20 | 0.82-1.74 | 0.332 |
| Male sex | 1.62 | 1.12-2.33 | 0.010 |
| Diabetes mellitus | 1.12 | 0.78-1.62 | 0.527 |
| Hypertension | 1.45 | 1.05-1.98 | 0.021 |
| Killip stage ≥ 2 | 1.67 | 1.20-2.31 | 0.002 |
| Triple-vessel coronary disease | 1.48 | 1.06-2.05 | 0.019 |
| Type B2 or C lesion | 1.29 | 0.86-1.92 | 0.213 |
| Successful PCI | 0.66 | 0.33-1.32 | 0.240 |
| Left ventricular ejection fraction ≤ 40% | 1.54 | 1.13-2.10 | 0.006 |
| Glucose ≥ 180 mg/dL | 1.03 | 0.72-1.48 | 0.843 |
| Estimated GFR < 60 mL/min/1.73m 2 | 1.85 | 1.28-2.68 | 0.001 |
| Beta-blocker | 0.83 | 0.58-1.18 | 0.299 |
| Heart block | 0.71 | 0.28-1.78 | 0.472 |
Of the 378 patients with heart block, 357 (94.4%) had available information on culprit lesion location. One patient with a culprit in the left main coronary artery was excluded, and 356 patients with heart block were analyzed. Table 4 lists the baseline characteristics of patients with heart block according to their culprit vessel (LAD vs RCA or left circumflex artery [LC]). Patients with a culprit lesion in the LAD had more unfavorable clinical features including higher Killip stage, lesser LV systolic function, lesser renal function, and smaller mean stent diameter than those of patients with a culprit lesion in the RCA or LC. Of the 356 patients with heart block, 54 (15.1%) had a 30-day MACE. Comparisons of clinical events at 30 days after AMI between patients with a culprit in the LAD and RCA or LC are listed in Table 5 . Patients with a culprit in the LAD had more MACE than patients with a culprit in the RCA or LC. This difference was mainly attributed to cardiac death. A multiple logistic regression analysis was performed to identify independent risk factor for 30-day MACE among patients with heart block ( Table 6 ). After adjustment for potential confounders, a culprit lesion in the LAD remained a significantly greater risk for a 30-day MACE (odd ratio 5.28, 95% confidence interval 1.22 to 22.81, p = 0.026).
| Characteristic | LAD culprit (n = 28) | Right or LCX culprit (n = 328) | p value |
|---|---|---|---|
| Age (years) | 68.5 ± 11.0 | 67.0 ± 11.2 | 0.503 |
| Male sex | 19 (67.9%) | 207 (63.1%) | 0.617 |
| Body mass index (kg/m 2 ) | 25.1 ± 9.2 | 23.9 ± 3.3 | 0.146 |
| Diabetes mellitus | 14 (50.0%) | 114 (34.8%) | 0.075 |
| Hypertension | 19 (70.4%) | 186 (56.7%) | 0.167 |
| Smoker | 9 (33.3%) | 178 (54.8%) | 0.032 |
| Systolic blood pressure (mm Hg) | 102 ± 36 | 100 ± 30 | 0.839 |
| Diastolic blood pressure (mm Hg) | 62.8 ± 22.6 | 64.1 ± 17.6 | 0.785 |
| Heart rate (per minute) | 58.3 ± 25.4 | 55.3 ± 21.4 | 0.479 |
| Killip stage ≥ 2 | 19 (70.4%) | 170 (53.0%) | 0.081 |
| Left ventricular ejection fraction (%) | 48.9 ± 15.4 | 55.0 ± 9.9 | 0.011 |
| Maximal CK-MB (ng/mL) | 120 ± 145 | 137 ± 159 | 0.585 |
| Maximal troponin I (ng/mL) | 39.2 ± 50.9 | 40.1 ± 38.4 | 0.939 |
| Total cholesterol (mg/dL) | 166 ± 41 | 166 ± 43 | 0.996 |
| LDL cholesterol (mg/dL) | 97 ± 34 | 103 ± 36 | 0.451 |
| HDL cholesterol (mg/dL) | 42.6 ± 10.7 | 41.1 ± 11.2 | 0.532 |
| Triglyceride (mg/dL) | 93 ± 43 | 122 ± 140 | 0.310 |
| Glucose (mg/dL) | 224 ± 131 | 221 ± 110 | 0.888 |
| Estimated GFR (mL/min/1.73m 2 ) | 39.0 ± 22.2 | 53.2 ± 25.7 | 0.017 |
| Triple-vessel coronary disease | 9 (32.1%) | 88 (27.0%) | 0.558 |
| Lesion type, B2 or C | 20 (76.9%) | 273 (83.5%) | 0.392 |
| PCI with DES | 18 (78.3%) | 279 (85.1%) | 0.337 |
| Stent number | 1.6 ± 0.9 | 1.5 ± 0.8 | 0.568 |
| Stent diameter (mm) | 3.0 ± 0.3 | 3.2 ± 0.4 | 0.032 |
| Stent length (mm) | 23.1 ± 7.5 | 24.7 ± 6.3 | 0.256 |
| Post-PCI TIMI flow III | 19 (86.4%) | 239 (89.8%) | 0.607 |
| PCI success | 22 (91.7%) | 253 (93.7%) | 0.697 |
| Discharge medication | |||
| Aspirin | 28 (100.0%) | 326 (99.4%) | 0.715 |
| Clopidogrel | 28 (100.0%) | 323 (98.5%) | 0.604 |
| Beta-blocker | 21 (75.0%) | 238 (72.5%) | 0.382 |
| ACE inhibitor or ARB | 23 (82.1%) | 272 (82.9%) | 0.885 |
| Statin | 17 (60.7%) | 243 (74.1%) | 0.275 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


