The coronary vasodilatory effect of dipyridamole is competitively blocked by caffeine. The purposes of this study were to (1) assess the incidence of having detectable serum caffeine and (2) evaluate whether an intensive caffeine history screening strategy was superior to routine history screening before dipyridamole myocardial perfusion imaging. One hundred ninety-four patients who were randomized to an intensive or a routine screening history strategy were prospectively evaluated. Serum caffeine levels were determined in all patients. Outcomes data, including death, nonfatal myocardial infarction, and history of revascularization, were obtained at 24 months. Nearly 1 in 5 patients (19%) who screened negative by history had detectable serum caffeine. In patients who screened negative by history, there was no statistically significant difference in the percentage of caffeine seropositivity between the intensive and routine arms (16% vs 22%, respectively, p = 0.31). The incidence of combined end points of death, myocardial infarction, or revascularization was 22.9% and 7.3% in patients with and without detectable serum caffeine, respectively (p = 0.01). In conclusion, despite initial negative results on screening by history, a considerably high percentage of patients had positive serum caffeine levels. These results do not support the use of an intensive screening strategy. Detectable serum caffeine was associated with a higher incidence of adverse outcomes.
Caffeine is found in routinely consumed beverages and foods such as coffee, tea, soda, and chocolate. Eighty percent of the United States adult population drinks coffee, with an average caffeine consumption of 200 to 300 mg/day. Caffeine is also a constituent of many other food products, herbal medicines, and prescription and over-the-counter medications, which may not be readily recognized to contain caffeine by patients or their physicians. The inadvertent use of caffeine before vasodilator stress testing can potentially lead to false-negative results, greatly compromising the sensitivity of the test. This study was designed to determine the incidence of detectable serum caffeine in patients who screened negative by history and also assess whether an intensive caffeine history screening strategy is superior to routine history screening in identifying patients who consumed caffeine products 24 hours before dipyridamole myocardial perfusion imaging (MPI). The study was also aimed at examining dipyridamole MPI results and clinical outcomes with regard to serum caffeine level.
Methods
We prospectively enrolled 194 consecutive patients who were referred to our stress laboratory for dipyridamole MPI. Patients were referred for the detection of coronary artery disease, evaluation of known coronary artery disease, or preoperative risk assessment. No patients were excluded from the study. All outpatients were instructed by scheduling office personnel to avoid the consumption of coffee, tea, caffeinated soda, and chocolate in the 24 hours before the test. In the case of hospitalized patients, an electronic reminder was given to the ordering physician to ensure that the patient did not ingest any caffeinated beverages or foods within the 24-hour period before the patient was to undergo a stress study. Upon presentation to the stress laboratory, patients who were scheduled for dipyridamole stress MPI were randomized to either a routine or an intensive caffeine history screening strategy. All patients underwent comprehensive assessments, including complete histories and physical examinations, baseline electrocardiography, and serum caffeine level measurements. The study protocol was approved by the local institutional review board.
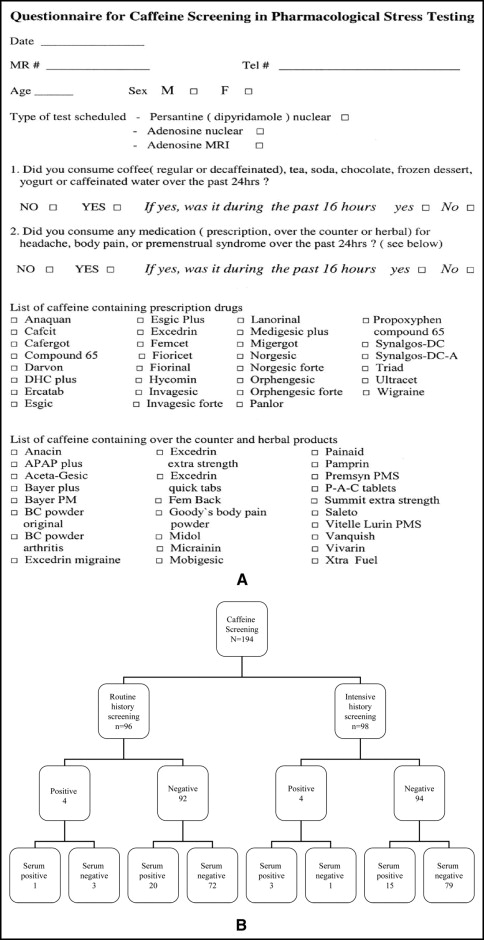
The routine caffeine history screening strategy, which is the standard assessment in the stress laboratory, constitutes inquiring about coffee, tea, soda, and/or chocolate consumption in the 24 hours before stress testing. The intensive caffeine history screening strategy involved a comprehensive evaluation, which used a questionnaire with a comprehensive list of beverages, foods, and herbal and pharmacologic agents that contain caffeine ( Figure 1 ). Patients who admitted to having consumed products containing caffeine in the 24 hours before the test were switched to dobutamine MPI and were excluded from the study.
At randomization, blood samples were obtained from all patients and analyzed for serum caffeine levels. An immunoassay technique (Dade Behring GmbH, Mannheim, Germany; Siemens Healthcare Diagnostics, Deerfield, Illinois) was used to measure caffeine levels. The assay had a detection limit of 1 mg/L. The stress test was done independent of serum caffeine measurement, because the result was not readily available.
After obtaining informed written consent, patients with negative results on initial screening underwent rest MPI with 3 mCi of thallium-201. Patients weighing >300 lb underwent rest MPI with technetium-99m. Once rest MPI was performed, dipyridamole was infused intravenously at a dose of 0.57 mg/kg over a period of 4 minutes. Eight minutes from the start of the test, approximately 30 mCi of technetium-99m (using a weight-based algorithm) was administered intravenously. Patients who reported chest discomfort, shortness of breath, or headache were given 100 mg of aminophylline intravenously 4 minutes after the radiopharmaceutical injection. Forty-five to 60 minutes after the administration of the radiopharmaceutical agent, gated MPI was performed using a GE Millennium MyoSIGHT rotating gamma camera (GE Healthcare, Milwaukee, Wisconsin). Patients were placed in supine position with the arms extended above the heads. They were advised to avoid any movement during the 20-minute scan period to ensure optimal image quality. If the cine image revealed excessive motion, the single photon-emission computed tomographic scan was repeated.
All gated single-photon emission computed tomographic data were submitted to the nuclear cardiology laboratory for reconstruction and preparation of images for uniform display. All images were interpreted without knowledge of the patient’s serum caffeine status. For each patient, stress images were interpreted in comparison with rest images. The test result was considered positive if a vasodilator-induced reversible myocardial perfusion defect was found.
Follow-up data were obtained by telephone and medical record review. For patients with outcomes or questionable outcomes, their medical records were reviewed. The mean follow-up period was 24 months. Outcomes data included death, nonfatal myocardial infarction, and history of revascularization after stress testing. The Social Security Death Index was used for patients whom we were unable to reach by telephone.
Mean comparisons for age and ejection fraction for the routine and intensive groups were performed with independent-samples Student’s t tests. Proportion comparisons for the routine and intensive groups and also the other proportion comparisons were performed using either Pearson’s chi-square test or Fisher’s exact test as appropriate. The nonparametric Mann-Whitney U test was used to compare the skewed caffeine serum level data for the routine and intensive groups. In those screening negative by history, logistic regression was used to calculate the odds ratios for the adverse outcome of death, myocardial infarction, or revascularization. First, all 27 baseline characteristics (see Table 1 ) and also serum caffeine (negative vs positive) were independently tested to determine if there was a relation to the outcome variable. Second, only the significant variables or variables approaching significance were simultaneously entered into a multivariate logistic regression analysis to determine the relations of these variables to the outcome variable of death, myocardial infarction, or revascularization. Because of the possible significance of stress test findings, additional univariate and multivariate logistic regression analyses were conducted that incorporated stress test results. SPSS version 11.5 (SPSS, Inc., Chicago, Illinois) was used for all analyses, except for the Fisher’s exact test analyses, which were performed using Stata version 9.2 (StataCorp LP, College Station, Texas).
| Variable | Routine | Intensive | p Value |
|---|---|---|---|
| (n = 96) | (n = 98) | ||
| Age (years) | 67.1 ± 11.8 | 66.4 ± 10.9 | 0.69 |
| Men | 36 (37%) | 38 (39%) | 0.85 |
| White | 36 (38%) | 44 (45%) | 0.56 |
| Black | 39 (41%) | 31 (32%) | |
| Hispanic | 16 (17%) | 19 (19%) | |
| Asian | 5 (5%) | 4 (4%) | |
| Coronary artery disease | 27 (28%) | 41 (42%) | 0.04 |
| Myocardial infarction | 13 (13%) | 16 (16%) | 0.58 |
| Diabetes mellitus | 38 (40%) | 43 (44%) | 0.54 |
| Hypertension | 74 (77%) | 80 (82%) | 0.43 |
| Dyslipidemia | 53 (55%) | 68 (69%) | 0.04 |
| Smoking | 14 (15%) | 11 (11%) | 0.48 |
| Renal failure | 7 (7%) | 4 (4%) | 0.33 |
| Congestive heart failure | 3 (3%) | 4 (4%) | 0.72 |
| Peripheral vascular disease | 9 (9%) | 11 (11%) | 0.67 |
| Cerebrovascular accident | 5 (3%) | 12 (12%) | 0.08 |
| Coronary artery bypass surgery | 11 (11%) | 14 (14%) | 0.55 |
| Percutaneous coronary intervention | 13 (13%) | 12 (12%) | 0.78 |
| Mean ejection fraction | 59.0% | 58.3% | 0.75 |
| Presenting symptom | |||
| Chest pain | 47 (49%) | 53 (54%) | 0.47 |
| Dyspnea | 17 (18%) | 27 (28%) | 0.10 |
| Medications | |||
| Aspirin | 37 (38%) | 43 (44%) | 0.45 |
| Clopidogrel | 16 (17%) | 23 (23%) | 0.24 |
| β blocker | 36 (37%) | 46 (47%) | 0.18 |
| Angiotensin-converting enzyme inhibitor | 46 (48%) | 60 (62%) | 0.05 |
| Statin | 38 (40%) | 52 (54%) | 0.05 |
| Indication | |||
| Detection of CAD | 56 (58%) | 46 (47%) | 0.11 |
| Evaluation of known CAD | 23 (24%) | 33 (34%) | 0.14 |
| Preoperative risk assessment | 15 (15%) | 17 (17%) | 0.75 |
Results
Among the 194 patients enrolled in the study, 96 were randomized to the routine caffeine history screening strategy and the remaining 98 to the intensive caffeine history screening strategy ( Figure 1 ). All patients were included in the analysis. Baseline characteristics were similar in the 2 groups, except that the proportions of patients with coronary artery disease and with dyslipidemia were greater in the intensive arm ( Table 1 ).
Thirty-five of 186 patients (19%) had caffeine in their serum despite negative initial screening results by history: 22% (n = 20) in the routine arm and 16% (n = 15) in the intensive arm (p = 0.31; Figure 1 ). The mean serum caffeine level in patients in the routine arm was 0.38 mg/L (1 and 6 mg/L), compared to a mean of 0.28 mg/L (1 and 3 mg/L) in patients in the intensive arm (p = 0.53).
Four patients each screened positive by history for caffeine consumption in the routine and intensive arms (4.2% vs 4.1%, respectively, p = 0.54). Among patients who screened positive on initial interview, 4 of 8 had no detectable caffeine in their serum. In the routine arm, 3 of the 4 patients who admitted to having consumed caffeine-containing products actually had no detectable caffeine in their serum ( Figure 1 ).
The proportion of positive stress test results was not statistically different between patients with negative serum caffeine (43.7%) and those with detectable serum caffeine (54.3%) (p = 0.26; Table 2 ). Using a cut-off value of 2 mg/L, 40% of patients with serum caffeine levels ≥2 mg/L had positive stress test results compared to 71% of those who had serum levels <2 mg/L (p = 0.063; Table 3 ). The mean serum caffeine levels in patients with positive and negative stress test results were 1.82 and 1.60 mg/L, respectively.



