Most population-based estimates of incident hospitalized heart failure (HF) have not differentiated acute decompensated heart failure (ADHF) from chronic stable HF nor included racially diverse populations. The Atherosclerosis Risk in Communities Study conducted surveillance of hospitalized HF events (age ≥55 years) in 4 US communities. We estimated hospitalized ADHF incidence and survival by race and gender. Potential 2005 to 2009 HF hospitalizations were identified by International Classification of Diseases, Ninth Revision, Clinical Modification , codes; 6,168 records were reviewed to validate ADHF cases. Population estimates were derived from US Census data; 50% of eligible hospitalizations were classified as ADHF, of which 63.6% were incident ADHF and 36.4% were recurrent ADHF. The average incidence of hospitalized ADHF was 11.6 per 1,000 persons, aged ≥55 years, per year, and recurrent hospitalized ADHF was 6.6 per 1,000 persons/yr. Age-adjusted annual ADHF incidence was highest for black men (15.7 per 1,000), followed by black women (13.3 per 1,000), white men (12.3 per 1,000), and white women (9.9 per 1,000). Of incident ADHF events with heart function assessment (89%), 53% had reduced the ejection fraction (heart failure with reduced ejection fraction [HFrEF]) and 47% had preserved ejection fraction (heart failure with preserved ejection fraction [HFpEF]). Black men had the highest proportion of acute HFrEF events (70%); white women had the highest proportion of acute HFpEF (59%). Age-adjusted 28-day and 1-year case fatality after an incident ADHF was 10.4% and 29.5%, respectively. Survival did not differ by race or gender. In conclusion, ADHF hospitalization and HF type varied by both race and gender, but case fatality rates did not. Further studies are needed to explain why black men are at higher risk of hospitalized ADHF and HFrEF.
Estimates of incident heart failure (HF) rates are often based on hospital discharge diagnoses codes that include chronic HF cases and possibly non-HF cases and, thus, may not reflect the actual number of hospitalizations for acute decompensated heart failure (ADHF). Because most HF patients are likely to be hospitalized within 5 years, 17% because of acute decompensation, reliable estimates are needed to better understand and track the risk, burden, and outcomes of HF. To assess the impact of clinical management on survival of HF, and the effect of risk factors and their control on HF incidence, it is important to obtain community-based estimates of ADHF events and monitor their changes. Previous studies reported that approximately half of overt HF cases are heart failure with preserved ejection fraction (HFpEF), but it is unclear if this distribution exists in diverse communities or in similar proportions across race-gender groups. The Atherosclerosis Risk in Communities (ARIC) study monitors prevalence and incidence of hospitalized ADHF in 4 communities. We describe here our first 5-year estimates of validated hospitalized acute decompensated HF events and case fatality (CF) by race, gender, and HF types.
Methods
The 4 ARIC study communities include Forsyth County, North Carolina; Jackson, Mississippi; Minneapolis, Minnesota; and Washington County, Maryland. Average gender- and race-specific population estimates for each study community were computed for 2005 to 2009 by extrapolations from the 2000 and 2010 US censuses. The estimated population size aged ≥55 years were Forsyth County, 395,782 (20.8% black); Jackson, 171,241 (60.9% black); Minneapolis suburbs, 253,225; and Washington County, 174,414. Because the Minneapolis suburbs and Washington County were predominately white, blacks from these 2 communities were not included in the final analysis.
Community surveillance of hospitalized ADHF began on January 1, 2005. Methods of event ascertainment and classification have been described previously. Briefly, a stratified random sample of eligible hospitalizations in 2005 to 2009 for HF was selected based on 3 criteria: (1) International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ) discharge diagnosis codes for HF or HF-related condition (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 415.0, 416.9, 425.4, 428.x, 518.4, and 786.0x) in any position; (2) age ≥55 years at the time of hospital discharge; and (3) home address within boundaries of the ARIC communities. The sampling varied by ICD-9-CM discharge codes (428 and non-428), field center, gender, and race (by race in Forsyth County and Jackson only) to achieve similar SEs across these groups ( https://www2.cscc.unc.edu/aric/surveillance-manuals ).
Eligible hospitalizations (unweighted n = 10,500) were abstracted by trained abstractors if the medical record documented any evidence of decompensation or new onset of HF symptoms or any mention by a physician that HF was the reason for hospitalization. Fully abstracted cases (unweighted n = 6,399) were independently classified by computer algorithm or 2 physicians of the ARIC Mortality and Morbidity Classification Committee into 1 of 5 categories as previously described : definite ADHF, possible ADHF, chronic stable HF, HF unlikely, or unclassifiable. Disagreements were adjudicated by the chair of the Mortality and Morbidity Classification Committee (HF specialist). Definite or possible ADHF required evidence from symptoms, signs, imaging, or treatment of an acute exacerbation, worsening or new onset of symptoms, or other decompensated circulatory state. For the purpose of this report, hospitalized HF classification was categorized as: ADHF (definite or possible ADHF), chronic HF, and no HF (HF unlikely or unclassifiable). ADHF events were further classified as heart failure with reduced ejection fraction (HFrEF; current or most recent left ventricular ejection fraction [LVEF] <50%), HFpEF (LVEF ≥50% or greater), or unclassifiable (unknown LVEF).
An incident ADHF event was defined as a hospitalization for ADHF with no previous hospitalization for HF noted in the medical record. Recurrent ADHF was defined as a hospitalized ADHF event with a previous hospitalization for HF. Vital status of hospitalized HF events within 1 year after discharge was determined by linkage with the National Death Index.
Population-based estimates for each community were computed by age, gender, and race on the basis of intercensal estimates derived by extrapolation from US Census data. After excluding a small number of nonblack minorities (n = 149), few blacks in 2 predominately white communities (Minnesota and Washington County; n = 81), and 1 with missing sampling information, the final sample included 6,168 hospitalizations with HF screening ICD-9-CM codes for the year 2005 to 2009. The weighted sample corresponded to 42,413 hospitalizations.
To account for the sampling design, all analyses were weighted by the inverse of the sampling probability. Age-specific rates and their SEs were calculated by Poisson regression. Rates were adjusted for age by direct standardization to the US population in 2000 and are reported as an average per year over the 5 years. Age-adjusted mortality curves were created based on Cox models with age as a covariate. The 28-day and 1-year CF percentages were computed by gender and race. All CF percentages were adjusted for age by the direct method using the ARIC combined hospitalized HF events as the standard; gender-specific percentages were also adjusted for race. Additional multivariable-adjusted regression analyses for CF included prevalent coronary heart disease, hypertension, diabetes, body mass index, asthma, or chronic obstructive pulmonary disease as covariates.
Results
Of the 42,413 HF-eligible hospitalizations, 41.2% were validated as ADHF, 9.0% as chronic HF, and 49.8% were classified as no HF; the most common ICD-9-CM discharge code was 428.xx (congestive HF, 89.1%). Of the validated hospitalized HF events, 82% were ADHF; 76.7% had either previous outpatient diagnosis of HF (73.4%) or treatment for HF (64.9%).
Of hospitalized ADHF events, 63.6% were incident hospitalized ADHF (53.2% of which had previous HF diagnosis) and 36.4% were recurrent events. Although 92.0% of those with ICD-9-CM code 428 listed as the primary diagnosis were validated ADHF, 42.3% of all ADHF events (37.3% of incident ADHF) had ICD-9-CM code 428 as the first listed diagnosis. Demographic and clinical characteristics were similar between all hospitalized ADHF events and the subset with incident hospitalized ADHF ( Table 1 ). Assessment of heart function either before or during the hospitalization was available in most patients. The most common co-morbidities were hypertension, coronary disease, chronic kidney disease (defined as stage 3 or worse), and diabetes. Of incident ADHF events, 12.3% were preceded by an acute myocardial infarction or unstable angina. Other possible precipitating factors of incident ADHF, in decreasing order, included atrial fibrillation or atrial flutter (10.7% of cases with a precipitating factor identified), pneumonia (9.4%), noncompliance with medications (9.4%), other infection (9.2%), noncompliance with diet (4.9%), excess fluid intake or administration (3.3%), and stroke or transient ischemic attack (1.2%).
| Variable | All ADHF (n = 3,695) | Incident ADHF (n = 2,252) | ||
|---|---|---|---|---|
| Mean or % | 95% CI | Mean or % | 95% CI | |
| Age (yrs) | 75.6 | 75.2–75.9 | 75.9 | 75.5–76.4 |
| Women | 53.6% | 52.2–55.1 | 55.3% | 53.3–57.3 |
| Caucasian | 72.4% | 71.2–73.5 | 78.5% | 77.0–80.0 |
| Black men | 15.2% | 14.3–16.2 | 12.2% | 11.0–13.4 |
| Black women | 12.4% | 11.7–13.2 | 9.3% | 8.4–10.3 |
| White men | 38.4% | 37.0–39.9 | 43.1% | 41.1–45.2 |
| White women | 33.9% | 32.6–35.3 | 35.4% | 33.5–37.4 |
| Heart function assessed ∗,† | 90.1% | 88.9–91.2 | 88.8% | 87.1–90.2 |
| LVEF before hospitalization (%) ∗,† | 40.7 | 39.9–41.6 | 44.2 | 43.1–45.4 |
| LVEF during hospitalization (%) ∗ | 41.9 | 41.1–42.7 | 43.4 | 42.5–44.3 |
| HFrEF | 58.3% | 56.4–60.2 | 53.0% | 50.5–55.5 |
| Previous diagnosis of HF | 70.1% | 68.4–71.8 | 53.2% | 50.8–55.6 |
| Body mass index (kg/m 2 ) ∗ | 29.0 | 28.6–29.4 | 29.2 | 28.8–29.7 |
| Obesity ∗ | 26.0% | 24.4–27.6 | 27.4% | 25.4–29.6 |
| Current smoker | 14.2% | 13.0–15.5 | 14.8% | 13.2–16.6 |
| Hypertension | 83.7% | 82.2–85.1 | 83.2% | 81.2–85.0 |
| Coronary heart disease | 67.5% | 65.8–69.1 | 63.1% | 60.8–65.3 |
| Acute MI or unstable angina pectoris | 10.7% | 9.6–12.0 | 11.7% | 10.3–13.4 |
| Atrial fibrillation or flutter | 35.8% | 34.1–37.6 | 31.9% | 29.7–34.2 |
| Valvular heart disease | 23.6% | 22.1–25.2 | 21.2% | 19.3–23.2 |
| Diabetes mellitus | 46.6% | 44.8–48.4 | 42.7% | 40.3–45.1 |
| Stroke or transient ischemic attack | 20.0% | 18.5–21.5 | 20.4% | 18.5–22.5 |
| Peripheral vascular disease | 13.9% | 12.7–15.2 | 13.2% | 11.7–14.9 |
| Asthma or chronic obstructive pulmonary disease | 37.7% | 35.9–39.5 | 36.0% | 33.8–38.4 |
| Sleep apnea | 9.1% | 8.1–10.2 | 8.6% | 7.4–10.1 |
| Chronic kidney disease ‡ | 66.1% | 64.3–67.8 | 63.8% | 61.5–66.0 |
∗ The percentage of all hospitalized ADHF and all incident ADHF, respectively, with available data for each of the following characteristics: heart function assessed: 90.1%, 88.8%; LVEF before hospitalization: 54.3%, 44.2%; LVEF during hospitalization: 59.9%, 64.9%; and body mass index and obesity: 73.1%, 74.0%.
† Assessment of heart function (ventricular systolic and diastolic function) was documented in the medical records (historical reference) or in reports of cardiac imaging (echocardiography, cardiac catheterization, and nuclear or other cardiac imaging tests). If there was more than 1 assessment of LVEF, the lowest value was used.
‡ Chronic kidney disease was defined as history of dialysis dependence and/or estimated glomerular filtration rate (using the Modification of Diet in Renal Disease method) of <60 ml/min/1.73 m 2 .
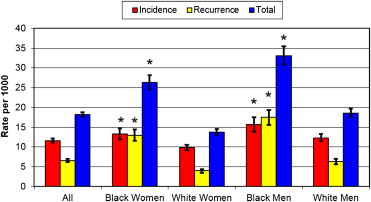
The incidence of hospitalized ADHF was 11.6 per 1,000 persons, aged ≥55 years, per year, and the rate of recurrent hospitalized ADHF was 6.6 per 1,000 persons per year. Incidence increased with advancing age in the overall population and in each race-gender group (p <0.001; Table 2 ). The incidence was higher in men than women overall (age-adjusted p <0.001) and for each age group (all p <0.001). The rate in blacks was significantly higher than the rates in whites, overall and for all age groups except those ≥75 years (p ≤0.005). The age-adjusted incidence of hospitalized ADHF was highest in black men, followed by black women, white men, and white women. Age-adjusted recurrence rates of hospitalized ADHF and age-adjusted hospitalization rates of ADHF showed similar patterns ( Figure 1 ). Rates did not differ significantly by community. When the definition of incident events excluded those with a previous diagnosis of HF (56%), the incidence estimates were lower, as expected, but the race-gender patterns were unchanged except that differences in rates between all men and all women and between men and women ≥75 years were no longer statistically significant ( Supplementary Table 1 ).
| Characteristics | Rate per 1,000 Persons (95% CI) | ||||
|---|---|---|---|---|---|
| Age Group (yrs) | |||||
| 55–64 | 65–74 | 75+ | All ∗ | ||
| All | 4.3 (3.8–4.7) | 9.6 (8.7–10.4) | 25.1 (23.7–26.5) | 11.6 (11.11–12.11) | |
| Race | Black | 8.6 (7.5–9.6) † | 13.4 (11.5–15.2) † | 23.6 (20.7–26.6) | 14.3 (13.19–15.39) † |
| White | 3.1 (2.6–3.5) | 8.7 (7.8–9.7) | 25.3 (23.8–26.9) | 10.9 (10.35–11.45) | |
| Women | Black | 7.2 (5.7–8.6) † | 13.0 (10.4–15.5) † | 23.2 (19.5–26.9) | 13.3 (11.92–14.72) † |
| White | 2.6 (2.0–3.2) | 7.7 (6.4–8.9) | 24.0 (22.0–25.9) | 9.9 (9.17–10.54) | |
| All | 3.7 (3.1–4.2) | 8.7 (7.6–9.8) | 23.8 (22.1–25.6) | 10.6 (9.97–11.22) | |
| Men | Black | 10.4 (8.8–12.0) † | 14.0 (11.3–16.6) † | 24.5 (19.6–29.4) | 15.7 (13.90–17.47) † |
| White | 3.6 (2.9–4.3) | 10.0 (8.6–11.5) | 27.7 (25.0–30.3) | 12.3 (11.42–13.25) | |
| All | 5.0 (4.3–5.6) ‡ | 10.7 (9.4–12.0) ‡ | 27.3 (24.9–29.6) ‡ | 13.0 (12.21–13.87) ‡ | |
∗ Adjusted for age by the direct standardization method, according to the distribution of the US population in 2000.
† p Value <0.05 for the gender-specific comparison between black and white groups.
‡ p Value <0.05 for the age group–specific comparison between all men and all women.
Among incident ADHF cases, mean LVEF was 42.4% (SE 0.4%; i.e., mean of the lowest LVEF estimates available), with 53.0% having HFrEF and 47.0% having HFpEF ( Table 1 ). For most incident ADHF cases, the etiology of HF was not specifically identified in the chart; however, 15.4% were ischemic cardiomyopathy, 7.1% systolic HF/other cardiomyopathy, 5.5% idiopathic dilated cardiomyopathy, 2.3% hypertensive cardiomyopathy, 2.3% diastolic HF, 1.0% cor pulmonale, and 0.2% hypertrophic cardiomyopathy. The overall age-adjusted incidence was higher for ADHF from HFrEF (8.31, 95% confidence interval [CI] 7.35 to 9.28 per 1,000 persons, aged ≥55 years, per year) than for ADHF from HFpEF (6.22, 95% CI 5.38 to 7.06 per 1,000 persons, aged ≥55 years, per year).
Black men had the highest proportion of incident acute decompensated HFrEF events followed by white men, black women, and white women (p <0.001; Table 3 ). White women had the highest proportion of incident acute HFpEF events followed by black women, white men, and black men (p <0.001). However, black women had similar or slightly higher proportion of incident HFrEF compared with HFpEF (p = 0.22). All validated ADHF events showed similar patterns although black women had more acute HFrEF (p = 0.002).



