Although lipid-lowering therapy with statin and ezetimibe has been reported to provide greater reduction in low-density lipoprotein cholesterol levels than statin monotherapy, the effect of supplemental therapy on plaque stabilization is yet to be fully elucidated. Cap thickness of fibroatheroma evaluated by optical coherence tomography (OCT) is a major determinant of vulnerable plaque. The primary objective of this study is to evaluate the effect of ezetimibe in addition to fluvastatin on the progression of coronary atherosclerotic plaque evaluated by OCT. Sixty-three patients with angina pectoris with intermediate, nonculprit, lipid-rich plaque lesions evaluated by OCT were enrolled. The patients were divided into 2 groups: ezetimibe (10 mg/day) + fluvastatin (30 mg/day), and fluvastatin (30 mg/day) alone, and serial OCT examinations were performed at baseline and 9-month follow-up. A total of 57 patients (ezetimibe + fluvastatin, n = 31; fluvastatin alone, n = 26) underwent serial OCT examinations. The change in low-density lipoprotein cholesterol level was significantly larger in the ezetimibe + fluvastatin group compared with fluvastatin-alone group (−34.0 ± 32.0 vs −8.3 ± 17.4 mg/dl, p <0.001). Fibrous cap thickness was significantly increased and the angle of the lipid plaque was significantly decreased in both groups. The change in the fibrous cap thickness was significantly greater in the ezetimibe + fluvastatin group (0.08 ± 0.08 mm vs 0.04 ± 0.06 mm, p <0.001). In conclusion, lipid-lowering therapy by ezetimibe + fluvastatin could increase the fibrous cap thickness of lipid-rich plaque compared with fluvastatin monotherapy.
A reduction of low-density lipoprotein cholesterol (LDL-C) level in individuals with and without preexisting coronary heart disease has been shown to reduce cardiovascular and total mortality rates. The effect of lipid-lowering therapy with statins in reducing adverse cardiovascular events is well recognized. By inhibiting hydroxymethylglutaryl-coenzyme A reductase, statins block the pathway for synthesizing cholesterol in the liver and have a wide range of biological effects, including reductions in the levels of blood cholesterol and high-sensitivity C-reactive protein (hs-CRP) for stabilization of atherosclerotic plaque. Recently, it was reported that not only the synthesis but also the absorption of cholesterol was associated with cardiovascular events. Ezetimibe inhibits the absorption of biliary and dietary cholesterol from the small intestine and its addition to statin therapy leads to further decrease in LDL-C and hs-CRP levels. Although it is possible that ezetimibe addition to statin therapy might affect plaque stabilization, there are few studies regarding changes of atherosclerotic plaque vulnerability. The primary objective of this study is to evaluate the effect of ezetimibe addition to statin on progression of coronary atherosclerotic plaque evaluated by optical coherence tomography (OCT).
Methods
This was a prospective single-center study with a randomized and nonblinded design. Patients aged 30 to 80 years with clinically stable angina pectoris scheduled for percutaneous coronary intervention (PCI) were enrolled. All patients had significant 1- or 2-vessel diseases and were eligible candidates for PCI. The inclusion criteria consisted of patients with (1) hypercholesterolemia (total cholesterol level >220 mg/dl and/or LDL-C level >140 mg/dl, or previously receiving statin therapy), (2) the target vessel for intervention with >75% de novo luminal narrowing by visual estimation throughout the target segment, (3) the target vessel for OCT interrogation had not undergone angioplasty and had angiographic diameter stenosis from 25% to 75%, (4) the target vessel for OCT interrogation had mild-to-moderate vessel tortuosity and calcification for safe and accurate examination, and (5) left ventricular ejection fraction >30%. In addition, inclusion criterion for OCT imaging was the target vessel for OCT interrogation having a lipid-rich plaque with a measurable fibrous cap thickness. Exclusion criteria were (1) significant stenotic lesions in all coronary vessels, (2) myocardial infarction within the previous 4 weeks, (3) the target vessel for OCT interrogation had lesions with angiographically detected thrombus, (4) contraindications to OCT examination, (5) other concomitant diseases or medical condition that could impact patient and/or procedural outcomes such as a history of bleeding diathesis, stroke, or transient ischemic neurologic attacks within the past year or hypersensitivity to heparin, aspirin, ticlopidine, or x-ray contrast media, (6) secondary causes of hyperlipidemia or uncontrolled triglyceride level >500 mg/dl, and (7) a positive pregnancy test. After diagnostic catheterization, patients who met eligibility criteria were invited to participate in this study.
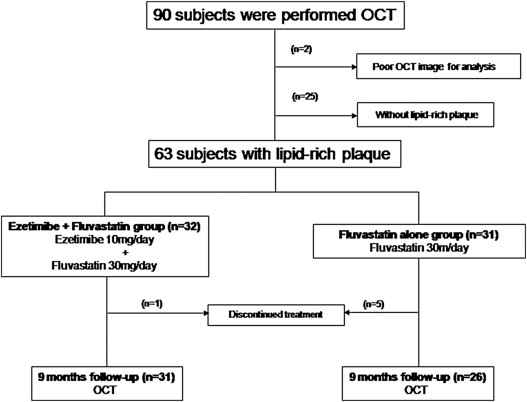
After OCT examination, the patients without OCT-evaluated lipid-rich plaque in the OCT target vessel were excluded from this study, and randomization was performed on a 1:1 ratio by envelope method into an ezetimibe + fluvastatin group: ezetimibe (10 mg/day) and fluvastatin (30 mg/day) and fluvastatin-alone (30 mg/day) groups ( Figure 1 ). No patients were receiving lipid-lowering therapy other than statins before enrollment into this study. Medications were open label for prescription and blinded for the imaging analysis. Angiographic and OCT follow-up were scheduled for the target vessel after 9 months. This study was approved by the institutional review board with written informed consent obtained from all patients.
All patients were given aspirin (100 mg/day) and ticlopidine (200 mg/day) or clopidogrel (75 mg/day) for at least 1 week before the procedure. During the procedure, heparin was given as a bolus of 150 U/kg with additional boluses to 2,000 U/hour. Before PCI procedure, OCT imaging was performed on the target vessel for OCT analysis after administration of 200 μg of nitroglycerin. OCT examination was performed as previously described. OCT imaging was performed using a time domain OCT imaging system (M2 OCT System; LightLab Imaging Inc., Westford, Massachusetts) with an occlusion-flushing balloon catheter (Helios; LightLab Imaging Inc.). Images were acquired at 15 frames/s and digitally archived.
OCT images were analyzed using proprietary off-line software provided by Lightlab Imaging Inc. Components of the plaque were classified as lipid, fibrous, and fibrocalcific using criteria for plaque characterization. Lipid-rich plaque was defined as lipid present in ≥2 quadrants within a plaque. Target plaques of OCT imaging were initially defined as lipid-rich plaque with a recognizable fibrous cap image. For each plaque, lumen area and fibrous cap thickness were evaluated at 1 mm longitudinal intervals with minimum–lumen area site and minimum–fibrous cap thickness site determined. At the minimum–fibrous cap thickness site, lumen area and lipid angle were also measured. The thickness of the fibrous cap was measured 3 times, and its average was defined as the minimum distance from the coronary artery lumen to inner border of the lipid pool, which was characterized by a signal-poor region in the OCT image. When there were 2 or more lipid-rich plaques, the plaque with the thinnest fibrous cap was selected for OCT analysis. At 9-month follow-up, the plaques were identified based on the distance from landmarks such as major branches. Intra- and interobserver analyses in random samples of 45 patients were performed by 2 experienced analysts. The first analyst repeated a blind analysis at least 2 weeks apart for intraobserver analysis. Intra- and interobserver differences in measurements of the fibrous cap thickness were 4.5 ± 1.2% and 4.3 ± 1.7%, respectively.
Laboratory data were obtained within 24 hours before the PCI procedure and at 9-month follow-up cardiac catheterization. All laboratory analyses were performed by SRL (Tokyo, Japan). Plasma total cholesterol, triglycerides, and high-density lipoprotein cholesterol concentrations were measured using standard enzymatic methods. LDL-C concentrations were calculated according to the Friedewald formula. Campesterol and sitosterol, cholesterol absorption markers, and lathosterol, a cholesterol synthesis marker, were quantified in plasma using a recently published gas chromatography and mass spectrometry–based method. In addition, apolipoprotein B and E levels were also measured. The following markers were also analyzed as proinflammatory markers: tumor necrosis factor α, hs-CRP, and interleukin-6.
Categorical variables are expressed as numbers or frequencies of occurrence (percentages). Continuous variables are expressed as mean ± SD. Comparisons between groups were performed with a 2-tailed Student t test for continuous variables and chi-square or Fisher’s exact test for categorical variables. Comparison of continuous variables between baseline and follow-up in each group was performed by a 2-tailed paired Student t test for normally distributed variables and Aspin-Welch t test for variables with heterogeneity of variance. The chi-square test or Fisher’s exact test for sparse data was used for comparing frequency of occurrence. Correlation between the change in fibrous cap thickness derived by OCT and the change in laboratory data was estimated using the Pearson correlation coefficient. The SPSS version 11.0 software (SPSS Inc., Chicago, Illinois) was used for data analysis. A p value of <0.05 was considered statistically significant.
Results
From April 2009 to December 2010, a total of 90 patients underwent PCI and OCT examination for this study. There was no periprocedural myocardial infarction in any patient. Lipid-rich plaque was detected in 63 patients and the patients were enrolled and randomized in this study ( Figure 1 ). One patient in the ezetimibe + fluvastatin group discontinued treatment due to a subdural hemorrhage. Comparatively, reasons for discontinued treatment in the fluvastatin-alone group were aortic dissection (n = 1), lung cancer (n = 1), and loss of follow-up (n = 3). Patients with other major adverse cardiac events including cardiac death, myocardial infarction, and stroke were not observed during the follow-up periods. Thus, both baseline and follow-up OCT examinations were evaluated for 31 patients with 31 vessels in the ezetimibe + fluvastatin group and 26 patients with 26 vessels in the fluvastatin-alone group. Baseline characteristics are summarized in Table 1 . The 2 groups were well matched for patient characteristics and medications.
| Characteristic | Ezetimibe + Fluvastatin (n = 32) | Fluvastatin Alone (n = 31) | p |
|---|---|---|---|
| Age (yrs) | 69.8 ± 7.8 | 68.8 ± 7.8 | 0.61 |
| Men | 21 (65) | 26 (83) | 0.1 |
| Body mass index (kg/m 2 ) | 24.5 ± 3.0 | 23.5 ± 4.0 | 0.27 |
| Body surface area (m 2 ) | 1.7 ± 0.2 | 1.6 ± 0.2 | 0.62 |
| Hypertension ∗ | 23 (71) | 18 (58) | 0.25 |
| Diabetes mellitus † | 11 (34) | 13 (41) | 0.54 |
| Current smoker | 7 (21) | 10 (32) | 0.35 |
| Medication at baseline | |||
| Oral hypoglycemic drugs | 9 (28) | 12 (38) | 0.37 |
| Insulin therapy | 1 (3.1) | 1 (3.2) | 0.98 |
| Calcium channel blockers | 14 (43) | 14 (45) | 0.91 |
| Angiotensin-converting enzyme inhibitors or angiotensin receptor antagonist | 10 (31.3) | 17 (54.8) | 0.06 |
| β Blocker | 2 (6) | 2 (7) | 0.97 |
| Nitrates | 6 (19) | 6 (19) | 0.95 |
| Statin | 13 (41) | 16 (51) | 0.38 |
| OCT target vessel | |||
| Left anterior descending artery | 9 (28) | 10 (32) | 0.19 |
| Left circumflex artery | 15 (47) | 8 (26) | |
| Right coronary artery | 8 (25) | 13 (42) | |
| Follow-up period (day) | 285.8 ± 54.4 | 291.3 ± 27.1 | 0.62 |
∗ Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of an antihypertensive drug.
† Diabetes was defined as diet controlled and oral agent or insulin treated.
Baseline and follow-up laboratory data including total cholesterol, LDL-C, high-density lipoprotein cholesterol, triglycerides, lathosterol, campesterol, sitosterol, and the campesterol/lathosterol ratio are shown in Figure 2 . Although total cholesterol and LDL-C levels were similar between the 2 groups at baseline and 9-month follow-up, the changes were significantly larger in the ezetimibe + fluvastatin group than the fluvastatin-alone group ( Figure 2 ). Campesterol and sitosterol absorption markers were significantly decreased in the Ezetimibe + Statin group from baseline to 9-month follow-up. On the other hand, those levels were significantly increased in the fluvastatin-alone group ( Figure 2 ). Other laboratory data including apolipoprotein B, apolipoprotein E, hs-CRP, interleukin-6, and tumor necrosis factor α levels are summarized in Table 2 . Although there was no significant difference in change in apolipoprotein E levels between the 2 groups, apolipoprotein B level was significantly decreased in the ezetimibe + fluvastatin group compared with the fluvastatin-alone group.



