Renal impairment frequently accompanies heart failure (HF) and is a recognized independent risk factor for morbidity and mortality. Few data are available assessing the impact of worsening renal function (WRF) during hospitalization on health care resource use in patients with HF. Health Insurance Portability and Accountability Act–compliant, de-identified, clinical, laboratory, and economic data for patients admitted to a tertiary care medical center with a primary diagnosis of HF were extracted by MedMining and reviewed retrospectively by the authors. Patients were excluded if they had no previous HF or were admitted for acute coronary syndrome or coronary artery bypass grafting within 30 days of index hospitalization. WRF was defined as ≥0.3 mg/dl increase in serum creatinine from baseline at any time during hospitalization. Of 5,803 hospitalized patients with primary HF diagnosis, 827 patients (14%) fulfilled all prespecified inclusion and exclusion criteria (74 ± 14 years of age, 43% men, 98% white, admission serum creatinine 1.4 ± 0.9 mg/dl, estimated glomerular filtration rate <90 ml/min/1.73 m 2 at admission in 83%). During index hospitalization, WRF was identified in nearly 33%. Compared to patients without WRF, those with WRF had greater prevalence of diabetes (54% vs 43%), lower estimated glomerular filtration rate (44 ± 30 vs 62 ± 35 ml/min/1.73 m 2 ), higher serum potassium (4.3 ± 0.7 vs 4.2 ± 0.7 mEq/L), and higher B-type natriuretic peptide (845 ± 821 vs 795 ± 947 pg/ml) at baseline (all p values <0.05). Patients developing WRF incurred higher total inpatient costs ($10,977, range 671 to 212,819, vs $7,820, range 697 to 269,797, p <0.001) and longer hospital stay (8.2 ± 6.8 vs 5.7 ± 5.5 days, p <0.001). In conclusion, occurrence of WRF during HF-related hospitalization is associated with higher hospitalization costs and longer hospital stay.
Worsening renal function (WRF) during hospitalization, defined as an increase in serum creatinine (SCr) value ≥0.3 mg/dl, has been reported in nearly 30% of acute heart failure (HF) admissions. This has been associated with inpatient length of stay exceeding 10 days (adjusted risk ratio 3.2, confidence interval 2.2 to 4.9) and increased in-hospital mortality (adjusted risk ratio 7.5, confidence interval 2.9 to 19.3). This study evaluated the costs and resource usage associated with WRF in a group of patients admitted with HF and a wide range of renal function in a single integrated health care system.
Methods
Data were prepared by MedMining (Danville, Pennsylvania), a Geisinger business unit that licenses Health Insurance Portability and Accountability Act–compliant, de-identified patient clinical, laboratory, and economic data to promote research based on data from a real-world setting. After an approved process for de-identifying the data, MedMining’s honest broker linked the following data together: (1) clinical and laboratory data from the electronic medical record system (Epic Systems Corporation, Madison, Wisconsin) used by Geisinger Health System (GHS) and (2) actual encounter-level cost data, including direct and indirect costs, from Geisinger’s financial data warehouse. The GHS consists of 3 hospitals located primarily in rural Pennsylvania with 791 beds and nearly 2 million yearly outpatient visits among its 41 community practice sites. These rural communities mostly consist of Caucasian/European-descent inhabitants.
All electronic health record patient-level data were captured for a period of ≥12 months before the index hospitalization, throughout the index hospitalization, and for up to 60 days after hospital discharge to examine preindex hospitalization health care usage, costs and resource use related to inpatient care, and short-term follow-up health care resource use and mortality.
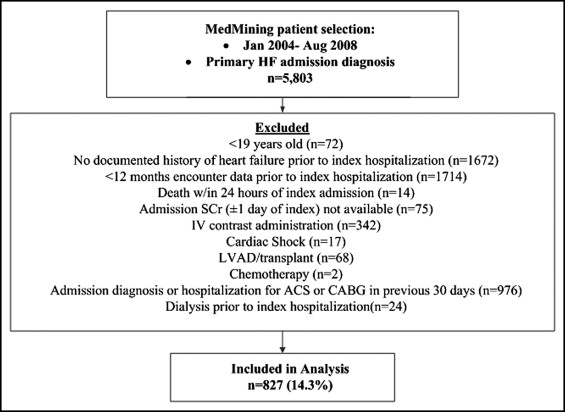
The database contained data of all patients admitted to a GHS facility with a primary or secondary inpatient HF diagnosis from January 2004 through August 2008. Patients were considered for inclusion in the study if they were ≥19 years of age and had ≥12 months of GHS encounter data before an index hospitalization with HF based on International Classification of Diseases, Ninth Revision, Clinical Modification codes. Patients were excluded if they had no documentation of HF before the index hospitalization (i.e., de novo HF), died within 24 hours of the index admission, or had no documented baseline (within 1 day of hospital admission) SCr. To limit the confounding effect of procedures or drug exposures known to be associated with acute renal dysfunction, additional criteria for exclusion included admission with a primary diagnosis of cardiogenic shock or acute coronary syndrome; exposure to radiographic contrast agents during the index hospitalization; current or previous use of a left ventricular assist device; chemotherapy or coronary artery bypass grafting surgery during or within 30 days of the index hospitalization; solid organ transplantation before or during the index hospitalization; or diagnosed end-stage renal disease on long-term dialysis.
Of the original 12,277 patients admitted with a primary or secondary diagnosis of HF during the prespecified period, 5,803 met all inclusion criteria ( Figure 1 ). Of the latter, 4,976 (85.7%) were also excluded due to the presence of ≥1 exclusion criterion. The remaining 827 patients (14.3%) who fulfilled all inclusion and exclusion criteria are the subjects of this evaluation.
The primary outcome measurement was total cost of the index hospitalization for patients stratified to the no-WRF and WRF groups. Costs are reported as the actual cost of care derived from the GHS Eclipsys cost accounting system database. All costs were adjusted to 2007 price levels using the medical care component of the consumer price index. Among inpatient costs, the following were evaluated: medication costs, costs for physician services, costs for procedures and laboratory tests, and costs for general hospital services. Inpatient usage variables included length of stay (total, intensive care unit, telemetric monitoring), number of procedures or laboratory tests performed, number of medication orders written, and total amount of intravenous loop diuretic (in furosemide equivalents) administered. The following doses of diuretics were considered equivalent: furosemide 40 mg, bumetanide 1 mg, and torsemide 10 mg. Hospital mortality and 30- and 60-day health care outcomes and usage were also evaluated.
The descriptive analysis includes population demographics, co-morbidities, information related to treatment such as the site where treatment was provided (e.g., inpatient, outpatient), medications, and select baseline laboratory values. Health care resource units (e.g., readmissions, emergency department visits, office visits, procedures, length of stay) and costs are stratified and compared by the presence of WRF defined as an increase in SCr ≥0.3 mg/dl from hospital admission to any time during the index hospitalization. Univariate analysis was conducted between the no-WRF and WRF groups for primary outcomes and secondary outcomes using chi-square test for categorical variables and t test or Mann-Whitney U test for continuous variables based on variable characteristics and data distribution. Comparison of continuous variables among ≥3 groups was performed by Kruskal-Wallis analysis of variance. Multivariable analysis was performed for the primary outcome. A generalized linear regression model with log-link function and γ distribution was performed to estimate total costs associated with the WRF and no-WRF groups. Variables that were found to have a difference at the significance level ≤0.10 during univariate analysis and those identified as clinically important from the relevant literature were included in the model to adjust for baseline differences. Correlations between variables were evaluated before modeling. If the correlation coefficient for 2 variables was >0.65 and statistically significant, then only 1 variable was included in the model to avoid multicollinearity. In addition, we used the general linear regression model for sensitivity analysis by looking at the association between level of SCr change and cost. The level of significance for all comparisons was set at a p value ≤0.05. All analyses were performed using SAS 9.1 (SAS Institute, Cary, North Carolina) and STATA 9 (STATA Corp. LP, College Station, Texas).
Results
Baseline clinical and demographic characteristics of the 827 patients and those of the 2 subgroups, without and with WRF, are presented in Table 1 . Approximately 55% of patients (n = 453) were ≥75 years of age at the index admission. Laboratory data obtained at admission are presented in Table 2 . All subjects had all laboratory values available on admission except where noted. Sixty subjects had no follow-up SCr value during the index admission and therefore are not represented within the no-WRF or WRF subgroup.
| Variable | Total | No WRF | WRF |
|---|---|---|---|
| (n = 827) | (n = 515) | (n = 252) | |
| Age (years) | 73 ± 14 | 74 ± 14 | 74 ± 14 |
| Men | 355 (43%) | 228 (44%) | 103 (41%) |
| White | 814 (98%) | 507 (99%) | 248 (98%) |
| Body mass index (kg/m 2 ) | 30 ± 8 | 30 ± 7 | 30 ± 8 |
| Current smoker | 81 (10%) | 53 (10%) | 23 (9%) |
| Admission through emergency department | 389 (72%) | 258 (73%) | 122 (76%) |
| Insurance coverage | |||
| Medicare | 434 (53%) | 289 (56%) | 123 (49%) |
| Medicaid | 29 (4%) | 15 (3%) | 9 (4%) |
| Commercial | 328 (40%) | 195 (38%) | 102 (41%) |
| Self/other | 35 (4%) | 16 (3%) | 18 (7%) |
| Preadmission health care use | |||
| Hospitalizations | 1.4 ± 0.8 | 1.5 ± 0.9 | 1.3 ± 0.7 |
| Hospital stay (days) | 9.6 ± 9.2 | 10.3 ± 9.7 | 8.5 ± 8.5 |
| Annual health care costs ($) | 13,518 ± 21,912 | 13,518 ± 21,912 | 14,280 ± 22,455 |
| Health care encounters | 49 ± 45 | 50 ± 46 | 46 ± 41 |
| β blocker | 461 (56%) | 288 (56%) | 136 (54%) |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 375 (45%) | 224 (44%) | 117 (46%) |
| Loop diuretics | 518 (63%) | 329 (64%) | 148 (59%) |
| Furosemide equivalent diuretic dose | 58 ± 56 | 55 ± 44 | 63 ± 78 |
| Co-morbidities | |||
| Cerebrovascular disease | 142 (17%) | 90 (18%) | 45 (18%) |
| Hypertension | 691 (84%) | 426 (89%) | 220 (87%) |
| Atrial fibrillation | 420 (51%) | 252 (49%) | 141 (56%) |
| Diabetes mellitus | 382 (46%) | 222 (43%) | 136 (54%) ⁎ |
| Myocardial infarction | 151 (18%) | 87 (17%) | 55 (22%) |
| Valvular disease | 418 (51%) | 250 (49%) | 141 (56%) |
| Renal insufficiency | 213 (26%) | 121 (24%) | 88 (35%) ⁎ |
| Serum creatinine increase ≥0.3 mg/dl in previous 3 months | 91 (11.0%) | 66 (12.8%) | 24 (9.5%) |
| Chronic pulmonary disease | 399 (48%) | 249 (48%) | 125 (50%) |
| Laboratory Variable | Total | No WRF | WRF |
|---|---|---|---|
| (n = 827) | (n = 515) | (n = 252) | |
| Serum creatinine (mg/dl) | 1.39 ± 0.93 | 1.36 ± 0.86 | 1.48 ± 1.01 ⁎ |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 57 ± 35 | 62 ± 36 | 44 ± 30 ⁎ |
| Serum urea nitrogen (mg/dl) | 32 ± 22 | 32 ± 23 | 33 ± 21 |
| Serum sodium (mEq/L) | 139 ± 4 | 139 ± 4 | 139 ± 4 |
| Serum potassium (mEq/L) | 4.2 ± 0.7 | 4.2 ± 0.7 | 4.3 ± 0.7 ⁎ |
| B-type natriuretic peptide (pg/ml) | 814 ± 901 (n = 422) | 795 ± 947 (n = 254) | 845 ± 821 ⁎ (n = 157) |
| ≤250 | 111 (26%) | 76 (30%) | 31 (20%) |
| 251–400 | 79 (19%) | 49 (19%) | 28 (18%) |
| >400 | 232 (55%) | 129 (51%) | 98 (62%) |
Prehospitalization SCr (within 3 months) was available in 337 patients and was acutely increased in 27% (n = 92). The percentage of the patients without or with WRF who had increased prehospitalization SCr was not significantly different (12.8% vs 9.5%, p = 0.183). A coded diagnosis of renal insufficiency before the index hospitalization was present in 26% of the total cohort. Overall, 36% presented with an increased SCr on admission to the hospital (defined as SCr >1.3 mg/dl) and 82% had an estimated glomerular filtration rate (eGFR) <90 ml/min as calculated by the Modification of Diet in Renal Disease method. Decreased eGFR at admission was significantly more prevalent in those who would eventually show WRF during the index hospitalization (203, 81%, vs 285, 55%). Of 767 patients with a follow-up SCr level during the index hospitalization, 252 (32.6%) had increased SCr ≥0.3 mg/dl anytime during hospitalization. Severity of WRF was proportional to the interval from admission to SCr measurement such that SCr increases of 0.30 to 0.39 mg/dl occurred in 3.0 ± 1.9 days and increases ≥0.5 g/dl occurred in 5.3 ± 5.9 days. Patients with an admission eGFR range of 30 to 59 ml/min represented the largest proportion of patients who developed WRF ( Figure 2 ).
The median of total cost of the index hospitalization was $8,826 (671 to 269,797) for the entire cohort ( Table 3 ) and was significantly lower in those without WRF compared to those with WRF ($7,820, 697 to 269,797, vs $10,977, 671 to 212,819, p <0.0001). Patients without WRF also had a shorter total length of stay; a smaller proportion remaining hospitalized >4 days; fewer procedures, medication orders, and laboratory tests; and lower usage of intravenous loop diuretics ( Table 4 ).
| Cost Variable ($) | Total | No WRF | WRF |
|---|---|---|---|
| (n = 827) | (n = 515) | (n = 252) | |
| Total | 8,825 (671–269,797) | 7,820 (697–269,797) | 10,977 (671–212,819) ⁎ |
| Mean ± SD | 16,195 ± 22,675 | 13,445 ± 20,392 | 20,829 ± 26,686 |
| Hospital services | 7,570 (1,154–246,067) | 6,878 (1,251–246,067) | 9,478 (1,866–183,872) ⁎ |
| Mean ± SD | 13,961 ± 19,735 | 11,532 ± 17,812 | 17,752 ± 22,791 |
| Physician services | 1,193 (12–29,850) | 1,071.53 (12–29,850) | 1,627.46 (46–28,947) ⁎ |
| Mean ± SD | 2,355 ± 3,532 | 2,030 ± 3,254 | 3,218 ± 4,327 |
| Medications administered | 393 (3–52,980) | 352.43 (3–52,980) | 680 (15–41,163) ⁎ |
| Mean ± SD | 1,396 ± 3,862 | 1,145 ± 3,532 | 2,184 ± 4,729 |
| Procedures | 552 (2–11,014) | 501 (2–9,333) | 911 (28–11,014) ⁎ |
| Mean ± SD | 900 ± 1,102 | 773 ± 858 | 1,309 ± 1,465 |
| Usage Variable | Total | No WRF | WRF |
|---|---|---|---|
| (n = 827) | (n = 515) | (n = 252) | |
| Total length of stay (days) | 6.2 ± 6.0 | 5.7 ± 5.5 | 8.2 ± 6.8 ⁎ |
| Intensive care | 5.1 ± 3.9 (n = 81) | 5.9 ± 4.3 (n = 36) | 4.5 ± 3.4 (n = 44) |
| Telemetry unit | 4.5 ± 3.5 (n = 351) | 4.0 ± 2.8 (n = 214) | 6.0 ± 4.2 ⁎ (n = 117) |
| Length of stay >4 days | 416 (50%) | 246 (48%) | 164 (65%) ⁎ |
| Total procedures performed | 33 ± 39 | 28 ± 29 | 48 ± 53 ⁎ |
| Medication orders | 37 ± 37 | 34 ± 36 | 47 ± 39 ⁎ |
| Laboratory results | 76 ± 79 | 66 ± 67 | 104 ± 94 ⁎ |
| Intravenous loop diuretic doses given | 0.97 ± 0.91 | 0.84 ± 0.86 | 1.42 ± 0.89 ⁎ |
| Total intravenous loop diuretic (mg) | 270.57 ± 1,085.21 | 190.62 ± 640.25 | 487.26 ± 1,719.53 ⁎ |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


