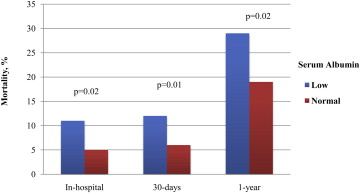
Risk assessment for transcatheter aortic valve replacement (TAVR) patients is challenging, and surgical scores do not optimally correlate with outcome. The aim of this study was to assess the correlation between serum albumin and survival of patients with symptomatic severe aortic stenosis undergoing TAVR. Patients with severe aortic stenosis who underwent TAVR were categorized into 2 groups according to low and normal preprocedural serum albumin (<3.5 and ≥3.5 g/dl, respectively). The all-cause mortality rates at hospital discharge, at 30-day and 1-year follow-up were compared across the groups. Additionally, a Cox proportional-hazards model was generated to assess the independent effect of serum albumin at 1-year follow-up. Among 567 consecutive patients who underwent TAVR, 476 (84%) had documented preprocedural serum albumin measurements. Of these, 50% had low serum albumin levels, and 50% had normal serum albumin levels. Baseline and procedural characteristics, including age, gender, and transapical access, were similar among the groups. Prevalence of left ventricular ejection fraction <40% was higher in patients with low albumin (29% vs 20%, p = 0.02), and risk assessment according to Society of Thoracic Surgeons score tended to be higher in the low-albumin group (10 ± 4.7 vs 9.4 ± 4.4, p = 0.09). Patients presenting with low albumin had higher in-hospital mortality (11% vs 5%), as well as at 30-day (12% vs 6%, p = 0.01) and 1-year (29% vs 19%, p = 0.02) follow-up. Serum albumin was independently associated with 1-year mortality (adjusted hazard ratio per 0.1 g/dl decrease 1.64, 95% confidence interval 2.50 to 1.75, p = 0.02), along with body mass index <20 kg/m 2 (hazard ratio 1.89, 95% confidence interval 3.33 to 1.75, p = 0.03). In conclusion, preprocedural serum albumin level and low body mass index are independently associated with mortality in patients who undergo TAVR. Patients with severe aortic stenosis and low albumin levels should undergo careful evaluation before and after TAVR.
Serum albumin has been previously associated with poor prognosis, including high mortality from cardiovascular disease and cancer, and is considered a marker for poor outcomes in different patient subsets. Indeed, serum albumin has been previously incorporated into intensive care unit scores such as the Acute Physiology, Age, and Chronic Health Evaluation III score. Moreover, serum albumin is considered a part of the frailty criteria, as a marker of malnutrition. Albumin level is a simple marker, is easy to measure, and is not subject to inter- or intraobserver bias. Data regarding the prognostic role of serum albumin are scarce, and it remains unclear whether serum albumin independently influences outcomes in patients who undergo transcatheter aortic valve replacement (TAVR).
We aimed to evaluate the predictive value of serum albumin on outcomes and complication rates of TAVR patients at a high-volume single center in the United States.
Methods
This was a retrospective study of 567 consecutive patients with severe symptomatic aortic stenosis (AS) treated with TAVR from May 2007 to July 2014. Prespecified clinical, procedural, and laboratory data were prospectively collected for all patients during screening, on admission, immediately after the procedure and during hospitalization, and on follow-up. During screening, blood was collected for biochemistry analysis, which included renal function markers and protein levels including serum albumin. Serum albumin was measured by the bromocresol purple method, as previously described. The study was approved by the local institutional review board.
Data collected were from demographic information, medical history, and clinical information, including echocardiographic indexes, baseline electrocardiography, and laboratory indexes. The Society of Thoracic Surgeons (STS) score was calculated for every patient. Procedural data collected in the database included the access site, amount of contrast injected, procedural length, and immediate complications according to the Valve Academic Research Consortium 2 criteria. Postprocedural data used the hospital’s documents as a primary source for laboratory results, length of stay, and in-hospital complications.
For the present study, the patient population was divided into 2 groups on the basis of pre-TAVR serum albumin levels, which were determined during the screening process, according to a cutoff of 3.5 g/dl. The primary end point for the study was mortality rates at 1-year follow-up as determined by the US Social Security Administration’s death index linkage database.
Continuous variables are expressed as mean ± SD for normally distributed variables and were compared using Student’s t test. Categorical variables are expressed as numbers and percentages and were compared using the chi-square or Fisher’s exact test. Kaplan-Meier analysis with the log-rank test was used to evaluate mortality rates of TAVR patients according to the albumin level cutoff. Univariate Cox proportional-hazards regression analysis was performed, with mortality at 1 year as the dependent variable. Variables with p values <0.10 were selected to enter the multivariate survival analysis and included age, gender, African-American race, serum albumin, body mass index (BMI) <20 kg/m 2 , STS score, chronic lung disease, previous percutaneous or surgical revascularization, admission hemoglobin level, ejection fraction <40%, and aortic valve area. A p value <0.05 was considered statistically significant. All analyses were performed using SAS version 9.2 (SAS Institute Inc, Cary, North Carolina).
Results
This registry included 567 TAVR patients, 476 (84%) of whom had available preprocedural serum albumin levels. From this group, 238 patients (50%) had serum albumin levels <3.5 g/dl, while an equal number of patients had serum albumin levels ≥3.5 g/dl. Baseline characteristics of the 2 groups are listed in Table 1 .
| Variable | Low Albumin n=238 | Normal Albumin n=238 | p-value |
|---|---|---|---|
| Age (years) | 84±8 | 83±7 | 0.06 |
| Male | 157 (79%) | 190 (87%) | 1 |
| African American | 32 (16%) | 20 (9%) | 0.03 |
| Body Mass Index (Kg/m 2 ) | 27±6 | 28±7 | 0.09 |
| Hypertension | 211 (92%) | 217 (94%) | 0.56 |
| Diabetes Mellitus | 79 (35%) | 79 (34%) | 0.92 |
| Prior Cerebrovascular Disease | 32 (16%) | 41 (18%) | 0.49 |
| Chronic Obstructive Pulmonary Disease | 77 (34%) | 67 (29%) | 0.23 |
| Atrial Fibrillation | 101 (44%) | 88 (38%) | 0.18 |
| Pacemaker/Defibrillator | 37 (21%) | 43 (25%) | 0.35 |
| Peripheral Vascular Disease | 76 (34%) | 83 (36%) | 0.63 |
| Prior Malignancy | 50 (28%) | 50 (28%) | 0.95 |
| Prior Percutaneous Coronary Intervention | 60 (26%) | 74 (32%) | 0.17 |
| Prior Coronary Bypass | 67 (29%) | 86 (37%) | 0.07 |
| Prior Ischemic Heart Disease | 132 (74%) | 136 (74%) | 0.97 |
| New York Heart Association III/IV | 210 (94%) | 214 (95%) | 0.8 |
| Hemoglobin g/dL | 11±1.4 | 12±1.6 | <0.001 |
| Creatinine, mg/dL | 1.3±0.9 | 1.3±0.9 | 0.66 |
| Serum Albumin | 3.1±0.3 | 3.8±0.3 | <0.001 |
| STS | 10±4.7 | 9.4±4.4 | 0.09 |
| Echocardiographic | |||
| Ejection Fraction<40% | 67 (29%) | 46 (20%) | 0.02 |
| Aortic Valve Area cm 2 | 0.64±0.13 | 0.67±0.12 | 0.02 |
| Indexed Aortic Valve Area, cm 2 /Kg 2 | 0.35±0.07 | 0.37±0.07 | 0.05 |
| Mean Gradient, mmHg | 48±14 | 48±12.5 | 0.7 |
Procedural data are listed in Table 2 and exhibited no significant differences in approach (transapical vs transfemoral) and Valve Academic Research Consortium 2 procedural success. Although the rates of vascular complications were numerically higher in patients with low albumin, despite similar sheath-to-artery ratios, they did not reach statistical significance ( Table 3 ).
| Variable | Serum Albumin | p-value | |
|---|---|---|---|
| Low (n=238) | Normal (n=238) | ||
| Transfemoral approach | 181 (76%) | 174 (73%) | 0.4 |
| Sheath to Artery Ratio | 1.05±0.16 | 1.05±0.14 | 0.87 |
| Balloon Pre-dilatation | 223 (95%) | 223 (95%) | 1 |
| Rapid Pacing | 230 (98%) | 233 (98%) | 0.54 |
| Fluoroscopy time | 22±19 | 21±16 | 0.66 |
| Contrast Volume | 125±77 | 121±64 | 0.53 |
| Device Success | 222 (93%) | 230 (95%) | 0.53 |
| Balloon Post-Dilation | 12 (6%) | 14 (7%) | 0.66 |
| Second Valve | 6 (3%) | 3 (1.4%) | 0.50 |
| Variable | Serum Albumin | p-value | |
|---|---|---|---|
| Low (n=238) | Normal (n=238) | ||
| Vascular Complication | |||
| Major | 37 (16%) | 41 (18%) | 0.65 |
| Minor | 26 (11%) | 21 (9%) | 0.42 |
| Bleeding | |||
| Major | 6 (3%) | 1 (0.4%) | 0.07 |
| Minor | 31 (13%) | 37 (16%) | 0.45 |
| Aortic Regurgitation≥2 | 8 (4%) | 8 (4%) | 1.00 |
| Transfusion | 100 (43%) | 94 (40%) | 0.52 |
| Stroke | 11 (5%) | 12 (5%) | 0.84 |
| Acute kidney injury≥2 | 29 (13%) | 31 (14%) | 0.72 |
| Tamponade | 1 (0.4%) | 2 (0.8%) | 0.6 |
| Complete Heart Block | 12 (5%) | 16 (7%) | 0.43 |
| Pacemaker implantation | 12 (5%) | 18 (8%) | 0.09 |
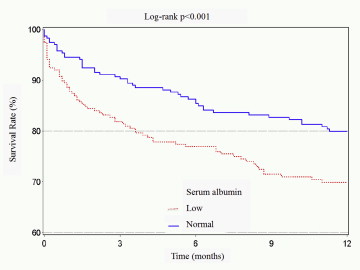
Unadjusted mortality rates were higher in the lower albumin group in the hospital and at 30-day and 1-year follow-up ( Figure 1 ). Survival curve analysis showed a significantly increased mortality rate among TAVR patients with low serum albumin in comparison with normal-range albumin patients ( Figure 2 ).
A univariate Cox proportional-hazards analysis for 1-year mortality revealed correlations with lower serum albumin, STS score, and low BMI, while chronic obstructive lung disease and left ventricular ejection fraction <40% reached only marginal significance ( Table 4 ). The interaction between BMI and serum albumin was found to be nonsignificant (p = 0.11). In a comparison of 1-year mortality rates across 3 BMI groups (<20, 20 to 30, and >30 kg/m 2 ), the significance of BMI as a predictor of mortality was pronounced mainly in the low-BMI group, while patients with normal and high BMIs had similar mortality rates at 1 year ( Figure 3 ).



