System delay (delay from emergency medical service call to reperfusion with primary percutaneous coronary intervention [PPCI]) is acknowledged as a performance measure in ST-elevation myocardial infarction (STEMI), as shorter system delay is associated with lower mortality. It is unknown whether system delay also impacts ability to stay in the labor market. Therefore, the aim of the study was to evaluate whether system delay is associated with duration of absence from work or time to retirement from work among patients with STEMI treated with PPCI. We conducted a population-based cohort study including patients ≤67 years of age who were admitted with STEMI from January 1, 1999, to December 1, 2011 and treated with PPCI. Data were derived from Danish population-based registries. Only patients who were full- or part-time employed before their STEMI admission were included. Association between system delay and time to return to the labor market was analyzed using a competing-risk regression analysis. Association between system delay and time to retirement from work was analyzed using a Cox regression model. A total of 4,061 patients were included. Ninety-three percent returned to the labor market during 4 years of follow-up, and 41% retired during 8 years of follow-up. After adjustment, system delay >120 minutes was associated with reduced resumption of work (subhazard ratio 0.86, 95% confidence interval 0.81 to 0.92) and earlier retirement from work (hazard ratio 1.21, 95% confidence interval 1.08 to 1.36). In conclusion, system delay was associated with reduced work resumption and earlier retirement. This highlights the value of system delay as a performance measure in treating patients with STEMI.
There is ample evidence that time from first contact with the health care system to initiation of reperfusion therapy (system delay) is associated with mortality in patients with ST-elevation myocardial infarction (STEMI). Approximately 45% of all patients admitted with acute myocardial infarction (AMI) are of the working age. In 2009, loss in production because of cardiovascular heart disease mortality and morbidity was estimated to cost the European Union around €18 billion, of which about 9% is due to illness among patients of working age. Only few studies have evaluated return-to-work rates and retirement in patients with STEMI treated with primary percutaneous coronary intervention (PPCI), and these have been based on small study samples. Shorter system delay is associated with lower risk of development of congestive heart failure after STEMI. Work outcome likely depends on left ventricular function (left ventricular ejection fraction), but it has not been evaluated whether shorter system delay affects the probability of return to the labor market or retirement from work. The aim of the present nationwide study was to examine the association between system delay and time to work resumption and time to retirement from work in patients with STEMI treated with PPCI.
Methods
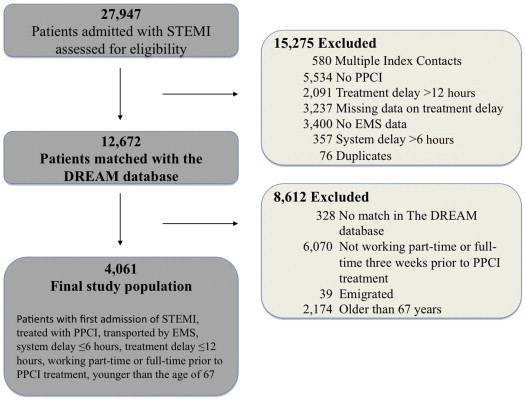
We conducted a population-based historical cohort study including all patients ≤67 years who were admitted with STEMI from January 1, 1999, to December 1, 2011. Only patients who were full-time or part-time employed, 3 weeks before STEMI were included, and for each patient only the first admission with STEMI during the study period was included. Eligible patients were transported by the emergency medical services (EMS), treated with PPCI within 12 hours of symptom onset at 1 of the 5 PCI-centers in Denmark (Aalborg, Gentofte, Odense, Rigshospitalet, and Aarhus University Hospital in Skejby), and had a maximal system delay of 360 minutes ( Figure 1 ). Patients with STEMI were identified from the Western Denmark Heart Registry (West Denmark) and the invasive cardiology (PATS) databases at Gentofte and Rigshospitalet (Eastern Denmark). These registries collect baseline characteristics and patient- and procedure-specific information on all angiographies and coronary interventions performed in all adult patients in Denmark since 1999. In 2008 the registration was 98% complete for PPCI.
The Danish health care system provides universal tax-supported healthcare, guaranteeing free access to general practitioners and hospitals, including EMS transportation for all inhabitants (5.5 million). The civil registration number, a 10-digit unique personal identifier number is assigned to all Danish residents at birth or immigration and used in all Danish healthcare registries, enabling unambiguous linkage on individual level of data from Western Denmark Heart Registry and PATS databases and other Danish registries.
The study was registered and approved by the Danish Data Protection Agency (J # 2012-41-0043), the Danish Health and Medicines Authority (j.nr.3-3013-81/1), and the National Board of Health (J.nr. 6-8011-978/1).
System delay was defined as the time from first contact to the EMS (112 call) to first catheterization with a guiding catheter during PPCI. The Danish EMS system including time registration has been described in detail elsewhere. First catheterization with a guiding catheter during PPCI was derived from the Western Denmark Heart Registry and PATS. System delay was categorized into 2 groups, namely ≤120 minutes and >120 minutes.
Outcomes were time to return to labor market, time to work retirement, and length of sick-leave period. All data were derived from the Danish National Register on Public Transfer Payments (DREAM). DREAM was founded in 1991 and includes weekly registration on public transfer payments from any Danish authority given to all persons with a civil registration number. DREAM is maintained by the Danish Ministry of Employment and updated monthly. By 2012, about 5 million Danes were registered. Those not included should not have received any transfer income from any Danish authority during the last 20 years. Each patient’s work situation was evaluated 1 year before and up to 8 years after the index PPCI procedure.
We recoded the original 104 different transfer-payment codes into 4 variables, namely (1) employment, (2) retirement from work, (3) sick leave, and (4) death ( Supplementary Table 1 ). Work resumption was defined as return to full- or part-time work and required 4 full consecutive weeks with no registration in the DREAM database or 1 of the transfer-payment codes predefined as “employment” ( Supplementary Table 1 ).
Retirement included the following 3 categories: (1) persons who were granted disability pension, available for those aged 18 to 59; (2) voluntary early retirement pension, available for those aged 60 to 65; and (3) public retirement pension, available for those aged 65+. In Denmark, the general retirement age is 65 to 67 years for both genders depending on birth year, but in the private sector and some occupations a higher retirement age is applicable.
Sick leave was defined as 1 or more full weeks on sickness allowance. In Denmark, sick leave extending beyond 3 weeks must be sanctioned by the workers’ general practitioner. Workers are entitled to receive sickness allowance for a maximum period of 52 weeks within an 18 month period with full compensation.
We used the Danish National Registry of Patients to identify co-morbid conditions before STEMI. This registry holds records of all nonpsychiatric hospitalizations in Denmark since 1977 and outpatient visits since 1995, including the dates of admission and discharge, and up to 20 discharge diagnoses classified according to International Classification of Diseases (eighth edition until the end of 1993 and tenth edition thereafter). Based on the complete hospitalization history of each patient, we computed the Charlson Co-morbidity Index. We classified co-morbidity into 2 categories, namely no co-morbidity and 1 or more co-morbidities.
We obtained information on vital status until July 19, 2012, from the Danish Civil Registration System. This registry contains information on all Danish residents from 1968 onward and includes daily updated information on vital status and migration.
Follow-up ended on July 19, 2012, and median follow-up time was 239 weeks (interquartile range [IQR] 126 to 358 weeks). When looking at return to labor market, follow-up began on the day of PPCI and ended on the date of return to the labor market, work retirement, death, emigration, or after 208 weeks of follow-up (4 years, this to ensure that at least 10% of the study population remained at risk), whichever came first. When looking at work retirement, follow-up began on the day of PPCI and ended at the date of work retirement, death, emigration, or after 416 weeks of follow-up (8 years, this to ensure at least 10% of the study population remained at risk), whichever came first.
Continuous data are summarized as medians with IQR. Categorical variables are reported as frequencies and percentages. The chi-square test and Wilcoxon rank sum test were used for comparisons of categorical variables and continuous variables as appropriate. Missing values among covariates were replaced with their conditional means, obtained from multiple imputations by the Stata ICE (StataCorp, College Station, Texas) command. We imputed 10 data sets based on the covariates listed in Table 1 . However, Killip class and predisposition of ischemic heart disease were missing in >20% of patients, so we chose not to impute them, and these variables were therefore not included in the final analysis.
| Characteristics | System delay (minutes) ∗ | P Value | |||
|---|---|---|---|---|---|
| ≤120 (N 2,305) ∗ | >120 (N 1,756) ∗ | ||||
| Patients (%) | Valid Cases | Patients (%) | Valid Cases | ||
| Median system delay (IQR † ) (minutes) | 89.3 (73.3-104.5) | 2,305 | 157.9 (135.9-192.7) | 1,756 | <0.001 |
| Median age (IQR † ) (years) | 54 (48-59) | 2,305 | 55(49-59) | 1,756 | 0.04 |
| Women | 334 (15%) | 2,305 | 291 (17%) | 1,756 | 0.07 |
| Non-married | 626 (27%) | 2,305 | 418 (24%) | 1,756 | 0.02 |
| Comorbidity | |||||
| 0 | 1,913 (83%) | 2,305 | 1,446 (82%) | 1,756 | 0.59 |
| 1+ | 392 (17%) | 310 (18%) | |||
| Treated hypertension | 520 (24%) | 2,173 | 357 (22%) | 1,625 | 0.15 |
| Diabetes mellitus | 139 (6%) | 2,186 | 87 (5%) | 1,641 | 0.18 |
| Familiar disposition IHD ‡ | 730 (46%) | 1,586 | 606 (43%) | 1,393 | 0.17 |
| Active or previous smoker | 1,832 (89%) | 2,056 | 1,273 (85%) | 1,489 | 0.001 |
| Killip class | 1,660 | 1,505 | 0.09 | ||
| I | 1,572 (95%) | 1,404 (93%) | |||
| II-IV | 88 (5%) | 101 (7%) | |||
| Median duration (IQR † ) (weeks) of work absenteeism during 4-years of follow-up | 10 (0-27) | 2,305 | 12 (3-31) | 1,756 | <0.01 |
∗ System delay is the time from first contact with the 112 service system until Primary Percutaneous Coronary Intervention.
We performed 2 different types of analyses. (1) The 4-year probability of returning to the labor market was assessed by the cumulative incidence function with death and work retirement as competing risks. Cumulative incidence curves were stratified according to intervals of system delay. Associations between system delay, selected clinical and demographic data, and work resumption were assessed using multivariate competing-risk analysis estimating subhazard ratios with 95% confidence intervals. (2) We used Cox proportional hazards regression to compute adjusted incidence rates (hazard ratios) of work retirement during an 8-year period with 95% confidence interval. Cumulative incidences were stratified according to intervals of system delay with death as a competing risk.
Comparisons of groups were performed by including system delay as a categorical variable in both the competing risk analysis and the Cox proportional hazards regression. We included year of index PPCI in the multivariate models to reveal a possible time trend.
In the Cox regression analysis, the assumption of proportional hazards was assessed graphically and found appropriate. In the competing-risk regression analyses, the proportional hazards assumption was checked by evaluating whether the subhazard ratios for each covariate were time-varying.
A p value <0.05 was considered to indicate statistical significance. All statistical analyses were carried out using Stata 11.0 statistical software (StataCorp, College Station, Texas).
Results
Our final analytic sample included 4,061 patients with STEMI treated with PPCI and with a treatment delay of <12 hours. For a full description of patient flow and exclusion criteria see Figure 1 .
Baseline patient characteristics stratified according to system delay are listed in Table 1 . Compared with those with a system delay >120 minutes, patients with system delays of ≤120 minutes were more likely to be younger, not married, and active smokers ( Table 1 ). There were no differences between groups regarding co-morbidity and gender ( Table 1 ).
At 1 month, 29% (n = 673) of patients with a system delay of ≤120 minutes had returned to the labor market, 96% of whom to a full-time position ( Figure 2 ). In patients with a system delay of >120 minutes, 25% had returned to work at 1 month (n = 436) with 94% being employed full-time. At 1 year the proportion of patients being employed had increased to 87% (n = 2,017) and 83% (n = 1,456) in the 2 groups, respectively. During follow-up, 93% (n = 2,137) of patients with a system delay of ≤120 minutes had returned to the labor market, whereas this was true for 89% (n = 1,557) of patients with a system delay of >120 minutes ( Figure 2 ). Table 2 lists factors associated with return to the labor market. In this multivariate analysis, system delay of >120 minutes remained associated with a lower chance of returning to the labor market. Moreover, men had a lower chance of returning to work compared with women. The association between system delay and return to work did not change over years.




