Pulse-wave velocity (PWV), a measure of arterial stiffness, is a known independent risk factor for cardiovascular events. Patients with single ventricle who undergo aortic to pulmonary anastomosis (recon) have noncompliant patch material inserted into the neoaorta, possibly increasing vessel stiffness and afterload. The purpose of this study is to determine if PWV in patients with single ventricle differed between those who did and those who did not undergo aortic reconstruction (nonrecon). We retrospectively reviewed cardiac magnetic resonance anatomic, cine, and phase contrast evaluations in the ascending aorta and descending aorta (DAo) at the level of the diaphragm data from 126 patients with single ventricle (8.6 ± 8.0 years) from January 2012 to May 2013. Significance = p <0.05. Seventy-five patients underwent recon and 51 did not. PWV in recon was significantly higher than in nonrecon (3.9 ± 0.9 m/s vs 3.2 ± 1.0 m/s, p = 0.008); in recon, patients >13 years old had a higher PWV than those <7 years (4.5 ± 0.6 vs 3.5 ± 0.7 m/s, p = 0.004). Whether <7 or >13 years old, PWV of those with recon was higher than nonrecon DAo distensibility was similar between both groups. There was no difference in age, body surface area, or cardiac index between recon and nonrecon. No correlations between various hemodynamic and ventricular function parameters with PWV were noted. In conclusion, PWV in recon is higher than in nonrecon with similar DAo distensibility implicating the aortic reconstruction as a possible cause of increased afterload; older recon patients have stiffer aortas than younger ones, possibly imposing an additional cardiovascular risk in the future. Other biomaterials may potentially moderate PWV if clinical outcome is adversely affected.
Highlights
- •
Pulse-wave velocity (PWV) is a measure of aortic stiffness.
- •
PWV is higher in patients with reconstructed aortas than those without.
- •
Within patients who have reconstructed aortas, those >13 years old had a higher PWV than those <7 years old.
- •
Descending aorta distensibility was similar between both groups.
The purpose of this study is to compare aortic stiffness using pulse-wave velocity (PWV) and distensibility of the descending aorta (DAo) at the level of the diaphragm in patients with single ventricle with and without an aortic reconstruction of all types (e.g., Damus-Kaye-Stansel or Norwood stage I procedures). We used cardiac magnetic resonance (CMR), which has successfully been used for years to assess single ventricle function, blood flow, and PWV. In a small study, PWV in the neoaorta of patients undergoing the Norwood procedure was compared with that of normal subjects and was found not statistically different from each other. Because of the variability in the amount and placement of patch material along with the inability to noninvasively identify all areas of patch, the utility of distensibility in the ascending aorta (AAo) was limited as the cross section of the AAo in some patients may contain all native tissue and in others may contain variable amounts of graft material; as a result of this, PWV was used. To determine the effect of aortic reconstruction on native aortic tissue, this study used distensibility of the DAo at the level of the diaphragm. Aortic PWV has been demonstrated to be an independent risk factor for cardiovascular events in adults such as all-cause cardiovascular mortality and coronary artery disease including myocardial infarction and stroke. We hypothesized that insertion of patch and suture material in the aortic wall will increase PWV.
Methods
A search of CMR database at our institution was performed for all patients with single ventricle who were studied from January 2012 to May 2013. Studies needed to include a stack of cine short-axis slices for ventricular function, a cine of the candy cane view of the aorta, and phase-encoded velocity mapping in the AAo and DAo at the level of the diaphragm. All patients who underwent CMR were enrolled making this series consecutive. Demographics obtained included age, body surface area, blood pressure, diagnosis, and the stage of surgical reconstruction. Patients <12 years of age underwent general anesthesia or sedation per hospital protocol. This study was approved by the institutional review board of the hospital.
CMRs were performed on a Siemens 1.5 T Avanto Magnetic Resonance Imaging (MRI) system (Siemens Medical Solutions, Malvern, Pennsylvania) with data analyzed using the standard Siemens’ analysis package (ARGUS) on a Leonardo workstation. A stack of static steady-state free precession images were obtained from the diaphragm to the neck to assess cardiovascular anatomy and to use as localizers for cine imaging and phase-encoded velocity mapping. Three-dimensional reformatting of this stack was used to obtain the “3-chamber view” of the single ventricle, ventricular short axis, and candy cane view of the aorta used in cine imaging as well as slice positions and orientation for phase-encoded velocity mapping. If the patient was under general anesthesia or sedation, multiple excitations were used to offset the effects of respiratory motion.
A stack of 8 to 12 steady-state free precession cine images using contiguous slices were obtained across the ventricle from atrioventricular valve to apex to obtain end-diastolic volume and ejection fraction. Volumes were obtained by contouring the endocardial borders at end-diastole and end-systole and summing the product of the area by the slice thickness across the entire ventricle; ejection fraction was calculated by the usual method. Ventricular mass was obtained by contouring the epicardial borders and subtracting the ventricular volume.
A candy cane view of the aorta was obtained by aligning a plane through the AAo and DAo on the stack of static bright blood axial images and angling this plane axially through the apex of the aortic arch; the parameters were similar to cine imaging for ventricular function.
Retrospective, electrocardiographic gated phase-encoded velocity mapping was obtained in the AAo and DAo. Velocity encoding was set between 150 to 200 cm/s for the aorta.
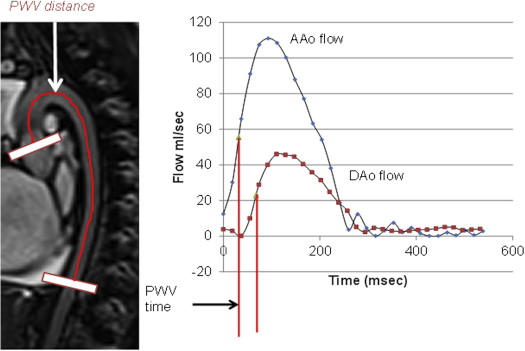
PWV was calculated by measuring the distance between the AAo and DAo phase-encoded velocity map planes and the time delay between the AAo and DAo flow-time curves ( Figure 1 ). The distance between the AAo and DAo phase-encoded velocity map planes was obtained from the candy cane view of the aorta (Δ x) and taken in the midsection of the vessel throughout its length. AAo and DAo flow-time curves were superimposed on each other, and midpoints of the systolic upslope of AAo and DAo were determined; the time delay between these 2 was used as the time for the pulse wave to travel from one imaging plane to the other (Δ t). PWV was calculated simply as Δ x/Δ t.
Distensibility was measured from 2-dimensional phase-encoded velocity mapping images in the DAo at the level of the diaphragm to determine the effect of the AAo patch and suture material distally. This was not calculated in the AAo because the variable amount of patch and suture material along with the variable placement of these materials would make distensibility determination in the AAo highly variable and an unreliable measure of stiffness. Distensibility of the DAo was calculated as follows :
Distensibility ( 10 − 3 mm Hg − 1 ) = ( A max − A min ) / [ A min × ( P max − P min ) ] ,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


