Right ventricular (RV) infarction is associated with increased mortality. Functional mitral regurgitation (FMR) may complicate inferoposterior infarction with RV involvement leading to pulmonary hypertension and increased RV afterload, potentially exacerbating RV remodeling and dysfunction. We studied 179 patients with inferior wall left ventricular (LV) ST-elevation myocardial infarction and RV infarction. The presence and severity of FMR and RV function were assessed by echocardiography. FMR was diagnosed based on echocardiographic criteria and when the severity of regurgitation was ≥moderate. Eighteen patients (10.0%) had ≥moderate FMR. Estimated pulmonary artery systolic pressure was higher in patients with FMR than in patients without FMR (43 ± 10 vs 34 ± 10 mmHg, respectively, p = 0.002). RV systolic dysfunction was present in 76 patients (42.5%). FMR was a strong predictor of RV dysfunction (odds ratio 5.35, 95% confidence interval [CI] 1.65 to 17.48, p = 0.005) independent of reperfusion therapy. During a median follow-up of 4.1 years, 20 (12.4%) and 10 (55.6%) deaths occurred in patients with and without FMR, respectively (p <0.001). In a multivariable Cox regression model, compared with patients without FMR and with normal RV function, the adjusted hazard ratio for mortality was 1.02 in patients without FMR and with RV dysfunction (95% CI 0.39 to 2.69, p = 0.97) and 3.62 in patients with FMR with RV dysfunction (95% CI 1.33 to 9.85, p = 0.01). In conclusion, in patients with RV infarction, the development of concomitant hemodynamically significant FMR is associated with RV dysfunction. The risk for mortality is increased predominantly in patients with both RV dysfunction and FMR.
Functional mitral regurgitation (FMR) is a common complication of myocardial infarction, and it is associated with increased risk of heart failure and mortality. FMR often occurs due to bulging of the inferior and posterior left ventricular (LV) base and midventricle after inferior and posterior infarction. When right ventricular (RV) infarction and FMR occur concomitantly in the context of inferior myocardial infarction, mitral regurgitation-induced pulmonary hypertension can potentially increase afterload on the RV during acute ischemia, impair RV recovery, and worsen clinical outcome. However, no data are available on the impact of FMR on the clinical outcome of patients with RV infarction. In the present study, we tested the hypothesis that hemodynamically significant FMR worsens RV function and the clinical outcome of patients with RV infarction.
Methods
The study participants were obtained from a cohort that consisted of patients enrolled in a prospective longitudinal observational study designed to determine predictors of postinfarction heart failure, with data collection starting in 2000. RV infarction was diagnosed in patients with acute inferior myocardial infarction (ST segment elevation ≥1 mV in 2 or more of leads II, III, and aVF) with ST-segment elevation of ≥0.1 mV in lead V4R at admission. The infarct-related artery was subsequently identified by coronary angiography to be the right coronary artery (RCA) in all patients.
All echocardiographic studies were performed during hospital stay at a median of 2 days from admission (interquartile range 1 to 3 days). FMR was quantified by an integrated approach. First, mitral regurgitation was graded qualitatively using color Doppler flow mapping integrating jet expansion within the left atrium (jet area/atrial area) and jet eccentricity as previously described. When mitral regurgitation severity was more than mild, other parameters were used, including vena contracta and calculation of mitral regurgitant volume and effective regurgitant orifice area when possible. In assessing the severity of the FMR, we also considered the coaptation distance and tenting area of the mitral valve. Systolic leaflet deformation was quantified by measuring tenting area and mitral leaflet coaptation height. Tenting area was equal to the area enclosed between the annular plane and mitral leaflets at midsystole from a parasternal long-axis view. Coaptation height was the distance between leaflet coaptation point and the mitral annulus plane. Mitral regurgitation was classified into 2 categories: (1) <moderate and (2) ≥moderate (moderate or severe FMR).
The estimated pulmonary artery systolic pressure (PASP) was calculated as the sum of the peak systolic pressure gradient across the tricuspid valve and the right atrial pressure. Right atrial pressure was estimated according to the size and respiratory variation of the inferior vena cava diameter in the subcostal view using established criteria. Pulmonary hypertension was defined as an estimated PASP >35 mm Hg. LV wall motion score index (WMSI) was calculated according to a 16-segment model.
RV systolic function and RV size were qualitatively estimated by visual assessment as previously described and by calculating the RV fractional area change. An RV fractional area change <35% was defined as abnormal. RV dysfunction was considered to be present if at least mild systolic dysfunction was observed.
The primary end point of the study was all-cause mortality. Following hospital discharge, clinical end point information was acquired by reviewing the national death registry and by reviewing the hospital records for major clinical events if the patient had been rehospitalized.
Continuous variables are presented as mean (SD) or median (with interquartile range), and categorical variables as numbers and percentages. For normally distributed variables, a comparison of means between 2 groups was made using Student t test. In cases of non-normally distributed variables, the Mann-Whitney U test was applied. Comparisons among proportions were carried out by chi-square statistic.
The association between the potential predictors and RV dysfunction was determined by fitting logistic regression models with stepwise backward selection. Results are reported as odds ratios, together with 95% confidence intervals (CIs). The following baseline clinical characteristics were considered in the multivariate procedure: age, gender, history of previous infarction, history of diabetes, history of hypertension, serum creatinine, Killip class on admission, reperfusion therapy, and WMSI. In addition, we included in the model individual LV regional wall motion abnormalities (WMAs) in the RCA territory, as they may reflect ineffective recanalization of the artery even in the presence of reperfusion therapy.
In a supporting analysis, PASP was also considered in the multivariate analysis as a predictor of RV dysfunction. However, PASP was missing in 34 patients (19%). Therefore, for this analysis, PASP was coded as ≤35 mm Hg (no PH), >35 mm Hg (PH), and “missing.”
Survival curves were constructed using the Kaplan-Meier method, and comparisons were made using the log-rank test. Stepwise Cox proportional hazards models with backward selection with retention at p <0.05 were used to construct a parsimonious model of the data. The following variables were considered in the multivariable procedure: age, gender, history of previous infarction, history of diabetes, history of hypertension, serum creatinine, Killip class on admission, reperfusion therapy, and WMSI. Variables with p <0.1 in the univariable Cox regression model were used in the multivariable model. Differences were considered statistically significant at the 2-sided p <0.05 level. Statistical analyses were performed using STATA version 12.0 (College Station, Texas).
Results
From January 2000 to December 2012, a total of 191 patients with acute inferior ST-elevation myocardial infarction and electrocardiographic evidence of RV infarction were admitted. Twelve patients died within 24 hours of admission without proper echocardiographic evaluation. In the remaining 179 patients, moderate or severe FMR was present in 18 patients (10.0%). Table 1 lists the clinical characteristics of the study population according to the presence or absence of FMR.
| Variable | Mitral Regurgitation Grade | ||
|---|---|---|---|
| None/Trivial/Mild (n = 161) | Moderate/Severe (n = 18) | p Value | |
| Age (years) | 62 ± 12 | 71 ± 9 | 0.002 |
| Women | 36 (22%) | 10 (56%) | 0.008 |
| Serum creatinine (mg/dL) ∗ | 1.1 ± 1.0 | 1.6 ± 1.7 | 0.27 |
| Prior myocardial infarction | 37 (23%) | 4 (22%) | 0.99 |
| Hypertension | 80 (50%) | 12 (67%) | 0.23 |
| Diabetes mellitus | 35 (22%) | 5 (28%) | 0.56 |
| Smoker | 18 (11%) | 0 (0%) | 0.45 |
| Killip class >I on admission | 22 (14%) | 6 (33%) | 0.04 |
| Primary PCI | 102 (63%) | 7 (39%) | 0.07 |
| Thrombolysis | 40 (25%) | 3 (17%) | 0.57 |
| Any reperfusion therapy | 142 (88%) | 10 (56%) | 0.002 |
| Medications | |||
| Antiplatelet agents | 159 (99%) | 17 (94%) | 0.27 |
| ACE inhibitors or ARBs | 137 (85%) | 11 (61%) | 0.046 |
| β-blockers | 140 (87%) | 13 (73%) | 0.15 |
| Statins | 136 (85%) | 7 (41%) | <0.0001 |
Patients with FMR were older and more likely to be women. They presented with higher Killip class and were less likely to receive reperfusion therapy and to be treated with angiotensin-converting enzyme inhibitors. LV systolic function, as assessed by WMSI, was similar between the 2 study groups ( Table 2 ). However, patients with FMR had higher PASP and higher rates of RV dysfunction. Several FMR mechanistic variables were different among the groups including the leaflet tenting area and leaflet tenting height ( Table 2 ).
| Variable | Mitral Regurgitation Grade | ||
|---|---|---|---|
| None/Trivial/Mild (n = 161) | Moderate/Severe (n = 18) | p Value | |
| Wall motion score index | 1.6 ± 0.3 | 1.7 ± 0.3 | 0.49 |
| Left atrial dimension (cm) | 4.0 ± 0.5 | 4.5 ± 0.6 | <0.001 |
| Estimated PASP | 34 ± 10 | 43 ± 10 | 0.002 |
| RV dysfunction | 61 (38%) | 15 (83%) | 0.001 |
| Estimated right atrial pressure (mm Hg) | 7 ± 4 | 11 ± 6 | 0.02 |
| RVFAC | 40 (33–48) | 24 (20–36) | <0.001 |
| RV dysfunction | 61 (38%) | 15 (83%) | 0.001 |
| Mitral leaflet tenting area (cm 2 ) | 1.2 (1.0–1.5) | 2.4 (2.2–2.6) | <0.001 |
| Leaflet tenting height (cm) | 0.7 (0.6–0.8) | 1.2 (1.1–1.4) | <0.001 |
| Posterolateral angle (degrees) | 19 (16–23) | 34 (31–43) | <0.0001 |
| Let ventricular sphericity index | 2.1 (1.9–2.3) | 1.8 (1.7–2.1) | 0.12 |
Although all patients had electrocardiographic evidence of RV ischemia at admission, echocardiography performed at a median of 2 days (interquartile range 1 to 3 days) revealed that RV systolic dysfunction was present in 76 patients (42.5%). FMR was present in only 3 of the patients with normal RV function (3.0%) and in 15 of the 78 patients with RV dysfunction (19.2%, p = 0.0003). The association of clinical variables and RV dysfunction was further evaluated using a logistic regression model.
Univariable analysis demonstrated that reperfusion therapy was associated with reduced risk for RV dysfunction, whereas moderate or severe FMR and WMAs in the RCA territory were associated with increased risk for RV dysfunction ( Table 3 , Model 1). In a multivariable logistic regression model with a stepwise backward elimination method, reperfusion therapy, FMR, and WMA in the basal posterior segment remained independently associated with RV dysfunction ( Table 3 , Model 1). A forward selection procedure resulted in the same model.
| Characteristics | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Model 1 | ||||
| Wall motion score index | 5.12 (1.95–13.47) | 0.001 | — | — |
| Basal inferior WMA | 3.74 (1.44–9.70) | 0.007 | — | — |
| Mid inferior WMA | 2.34 (1.25–4.38) | 0.008 | — | — |
| Basal posterior WMA | 3.11 (1.57–6.19) | 0.001 | 2.84 (1.32–6.10) | 0.008 |
| Mid posterior WMA | 2.23 (1.11–4.48) | 0.025 | — | — |
| Moderate/severe FMR | 8.49 (2.25–31.92) | 0.002 | 5.35 (1.65–17.48) | 0.005 |
| Reperfusion therapy ∗ | 0.13 (0.04–0.37) | 0.001 | 0.18 (0.07–0.51) | 0.001 |
| Model 2 | ||||
| PASP >35 mm Hg | 3.09 (1.53–6.24) | 0.002 | 2.77 (1.36–6.03) | 0.006 |
| Wall motion score index | 5.12 (1.95–13.47) | 0.001 | — | — |
| Basal inferior WMA | 3.74 (1.45–9.68) | 0.007 | — | — |
| Mid inferior WMA | 2.34 (1.26–4.37) | 0.008 | — | — |
| Basal posterior WMA | 3.11 (1.57–6.19) | 0.001 | 2.50 (1.13–5.56) | 0.02 |
| Mid posterior WMA | 2.23 (1.11–4.47) | 0.024 | — | — |
| Moderate/severe FMR | 8.49 (2.25–31.92) | 0.002 | 3.71 (1.01–13.62) | 0.048 |
| Reperfusion therapy ∗ | 0.13 (0.04–0.37) | 0.001 | 0.88 (0.06–0.52) | 0.002 |
When PASP was also used in the model, both FMR and PASP >35 mm Hg remained independent predictors of RV dysfunction ( Table 3 , Model 2). The c-statistic of models 1 and 2 was 0.71 (95% CI 0.63 to 0.78) and 0.75 (95% CI 0.68 to 0.82), respectively, indicating adequate discrimination.
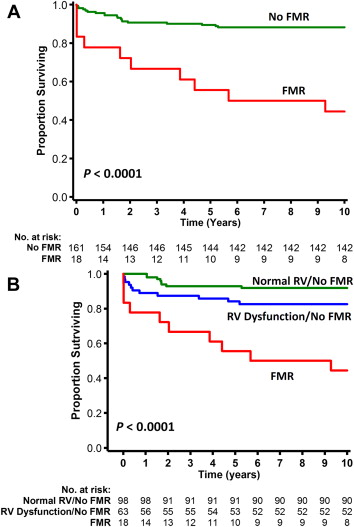
During a median follow-up of 4.1 years, 30 patients (16.8%) died, with 20 deaths (12.4%) occurring in patients without FMR and 10 (55.6%) in patients with FMR (p <0.001). The Kaplan-Meier survival curves of the study groups demonstrate a marked increase in the risk of mortality in patients with FMR ( Figure 1 ).