Besides poor clinical outcomes, female gender has been known as a high-risk factor for bleeding complications. This study aimed to investigate the impact of gender on clinical outcomes and bleeding complications after transradial coronary intervention (TRI). The Korean TRI registry is a retrospective multicenter registry with 4,890 patients who underwent percutaneous coronary intervention in 2009 at 12 centers. To compare clinical outcomes and bleeding complications between the male and female groups, we performed a propensity score matching in patients who received TRI. A total of 1,194 patients (597 in each group) were studied. The primary outcome was 1-year major adverse cardiac events, including all-cause mortality, myocardial infarction, target vessel revascularization, and stroke. The secondary outcome was major bleeding (composite of bleeding requiring transfusion of ≥2 units of packed cells or bleeding that was fatal). The proportion of major adverse cardiac events was similar between the 2 groups (6.2% vs 4.7%, p = 0.308). The female group had a greater incidence of major bleeding (0.3% vs 3.2%, p <0.001). On multivariate analysis, female gender (odds ratio [OR] 7.748, 95% confidence interval [CI] 1.767 to 13.399), age ≥75 years (OR 5.824, 95% CI 2.085 to 16.274), and chronic kidney disease (OR 7.264, 95% CI 2.369 to 12.276) were independent predictors of major bleeding. In conclusion, the female gender had a tendency for more bleeding complications than male gender after TRI without difference in the clinical outcome.
Female gender has been associated with poorer clinical outcomes after percutaneous coronary intervention (PCI). Also, it is known as an independent risk factor for vascular complications. Vascular complications have been associated with increased morbidity and mortality in transfemoral coronary intervention (TFI). The use of smaller sheaths and vascular closure devices and improved antithrombotic therapies have led to reduced access site–related bleeding. Transradial coronary intervention (TRI) has been associated with fewer vascular complications and bleeding complications than transfemoral coronary intervention. However, there is a paucity of data addressing the impact of gender on TRI. The objective of this study was to investigate the impact of female gender on clinical outcomes and bleeding complications after TRI.
Methods
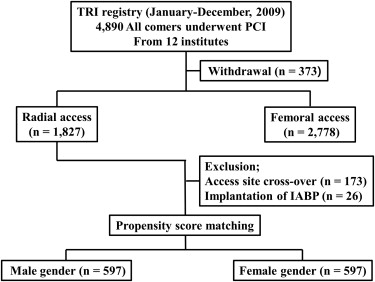
The Korean TRI registry was used for this retrospective observational study. A total of 4,890 patients from 12 centers were enrolled in this study from January to December of 2009. This study was based on 1,827 patients who underwent PCI by way of TRI. We excluded the patients who had access site crossover and implantation of intra-aortic balloon pump. Because the baseline characteristics between male and female patients were not matched, propensity score analysis was performed using a logistic regression model for male and female genders to adjust for differences in baseline characteristics. The variables used in propensity score matching included age, hypertension, diabetes mellitus, acute coronary syndrome (ACS), and chronic kidney disease (CKD). Male and female patients were matched one to one on the basis of the estimated propensity score of each patient. After all the propensity score matches were performed, a total of 1,194 patients (597 in each group) were studied ( Figure 1 ). Detailed data on demographics, medical history, coronary anatomy, procedural process, procedural events, pharmacotherapy, and 1-year outcome from the index procedure were collected using a standardized reporting form. This study received approval from each institutional review board.
We assessed clinical outcomes and safety outcomes at 1 year after the index procedure, which were determined before the registry was started. Clinical outcomes were major adverse cardiac events (MACE) composed of all-cause mortality, myocardial infarction (MI), target vessel revascularization, and stroke. All-cause mortality consisted of cardiac and noncardiac deaths. MI was defined as a creatine kinase myocardial band value of ≥3 times the upper normal limit. Target vessel revascularization was defined as any repeated PCI or bypass surgery of any segment of the target vessel. Stroke was defined as a clinical neurologic deficit from a hemorrhagic or ischemic neurologic insult.
The safety outcome was based on the rate of major bleeding. Major bleeding was defined according to the radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL) trial as one of the following: bleeding requiring transfusion of ≥2 units of packed cells or bleeding that was fatal. Fatal bleeding included the following: (1) intracranial bleeding, (2) one that brought about a reduction in the hemoglobin level of ≥5 g/dl or led to substantial hypotension requiring the use of intravenous inotropic agents, (3) one that required surgical intervention, or (4) one that required transfusion of ≥4 units of packed cells. Vascular access-related bleeding was defined as one that was related to surgical or procedural interventions, such as access artery dissection, perforation, arteriovenous fistula, pseudoaneurysm, or local hematoma requiring transfusion.
Continuous variables are expressed as mean ± SD and were compared using the independent t test. Categorical variables are expressed as number and percentage and were compared using the Fisher’s exact test or chi-square test. For descriptive analysis, we compared baseline and procedural characteristics and clinical and safety outcomes between the male and female groups. Stepwise logistic regression analysis was performed to assess the relation between female gender and outcomes. For major bleeding, the following variables were tested as independent predictors with bidirectional entry and p <0.2 for initial entry and removal: age ≥75 years, gender, hypertension, diabetes, dyslipidemia, smoking, ACS, previous MI, CKD, use of glycoprotein IIb/IIIa inhibitor, left ventricular ejection fraction, and arterial sheath size. All reported p values are 2-sided, and p values of <0.05 were considered statistically significant. SPSS software, version 18.0 (SPSS Inc, Chicago, Illinois), was used for all statistical analyses.
Results
There were no significant differences between the male and female groups in baseline demographics and co-morbid variables except smoking and previous MI ( Table 1 ). Procedural characteristics were similar between the 2 groups, but the male group had more chronic total occlusion lesion than the female group (7% vs 4%, p = 0.025; Table 2 ).
| Variable | Male (n = 597) | Female (n = 597) | p Value |
|---|---|---|---|
| Age (years) | 69 ± 9 | 70 ± 9 | 0.071 |
| Hypertension | 407 (68%) | 423 (71%) | 0.346 |
| Diabetes mellitus | 208 (35%) | 229 (38%) | 0.230 |
| Smoker | 403 (68%) | 67 (11%) | <0.001 |
| Current | 218 (37%) | 50 (9%) | |
| Ex-smoker | 185 (31%) | 17 (3%) | |
| Dyslipidemia | 163 (27%) | 190 (32%) | 0.099 |
| Chronic kidney disease | 17 (3%) | 25 (4%) | 0.271 |
| Prior coronary bypass surgery | 5 (0.8%) | 2 (0.4%) | 0.452 |
| Prior myocardial infarction | 62 (10%) | 39 (7%) | 0.022 |
| Prior percutaneous coronary intervention | 124 (21%) | 102 (17%) | 0.121 |
| Family history of coronary artery disease | 8 (1%) | 12 (2%) | 0.379 |
| Prior cerebrovascular accident | 39 (7%) | 39 (7%) | 1.000 |
| Ejection fraction (%) | 59 ± 12 | 59 ± 12 | 0.840 |
| Diagnosis | |||
| ST-elevation myocardial infarction | 45 (7%) | 44 (7%) | 1.000 |
| Non-ST-elevation myocardial infarction | 87 (15%) | 91 (15%) | 0.807 |
| Unstable angina pectoris | 274 (46%) | 270 (45%) | 0.862 |
| Stable angina pectoris | 158 (27%) | 157 (26%) | 1.000 |
| Silent ischemia | 19 (3%) | 12 (2%) | 0.275 |
| Atypical chest pain | 6 (1%) | 8 (1%) | 0.784 |
| Heart failure | 8 (1%) | 18 (3%) | 0.072 |
| Use of glycoprotein IIb/IIIa inhibitor | 18 (3%) | 11 (2%) | 0.259 |
| Use of clopidogrel | 531 (89%) | 514 (86%) | 0.161 |
| Use of cilostazol | 59 (10%) | 43 (7%) | 0.120 |
| Use of low molecular weighted heparin | 127 (21%) | 126 (21%) | 1.000 |
| Discharge medication | |||
| Aspirin | 589 (98%) | 590 (99%) | 1.000 |
| Clopidogrel | 585 (98%) | 583 (98%) | 0.843 |
| Ticlopidine | 2 (0.3%) | 2 (0.3%) | 1.000 |
| Cilostazol | 116 (19%) | 94 (15%) | 0.110 |
| Angiotensin receptor blocker | 262 (44%) | 244 (41%) | 0.319 |
| Angiotensin II converting enzyme inhibitor | 140 (24%) | 158 (27%) | 0.256 |
| Beta blocker | 362 (61%) | 347 (58%) | 0.271 |
| Statin | 473 (79%) | 490 (82%) | 0.241 |
| Variable | Male (n = 597) | Female (n = 597) | p Value |
|---|---|---|---|
| No. of coronary arteries narrowed | |||
| 1 | 444 (74%) | 438 (73%) | 0.807 |
| 2 | 132 (22%) | 136 (23%) | 1.000 |
| 3 | 21 (4%) | 23 (4%) | 0.837 |
| Coronary narrowed | |||
| Left main | 22 (4%) | 27 (5%) | 0.560 |
| Left anterior | 335 (56%) | 347 (58%) | 0.520 |
| Left circumflex | 177 (30%) | 168 (28%) | 0.610 |
| Right | 219 (36%) | 223 (37%) | 0.857 |
| Coronary lesion character | |||
| De novo lesion | 562 (94%) | 559 (94%) | 0.809 |
| ACC/AHA type C lesion | 323 (54%) | 326 (55%) | 0.907 |
| Chronic total occlusion | 44 (7%) | 25 (4%) | 0.025 |
| Bifurcation lesion | 144 (24%) | 137 (23%) | 0.682 |
| Diffuse long lesion | 87 (15%) | 74 (12%) | 0.309 |
| Calcified lesion | 99 (17%) | 97 (16%) | 0.938 |
| Percutaneous coronary intervention | |||
| Balloon angioplasty only | 7 (1%) | 13 (1%) | 0.259 |
| Bare-metal stent implantation | 12 (2%) | 15 (3%) | 0.689 |
| First generation DES implantation | 138 (23%) | 136 (23%) | 0.945 |
| Second generation DES implantation | 440 (74%) | 432 (72%) | 0.648 |
| Procedural events | |||
| Slow flow | 8 (1%) | 15 (3%) | 0.206 |
| Acute thrombosis | 1 (0.2%) | 1 (0.2%) | 1.000 |
| Dissection | 13 (2%) | 16 (3%) | 0.708 |
| Distal embolization | 0 | 2 (1%) | 0.500 |
| Perforation | 2 (0.3%) | 2 (0.3%) | 1.000 |
| Sheath size | |||
| 4F | 1 (0.2%) | 0 | 0.500 |
| 5F | 79 (13%) | 85 (14%) | 0.674 |
| 6F | 477 (80%) | 472 (80%) | 0.720 |
| 7F | 35 (6%) | 30 (5%) | 0.572 |
| 8F | 1 (0.2%) | 2 (0.4%) | 1.000 |
| Procedure time (min) | 54 ± 32 | 52 ± 28 | 0.294 |
There was no significant difference in MACE at 1 year between the 2 groups (6.2% vs 4.7%, p = 0.308; Table 3 ). On multivariate analysis, independent predictors of MACE were age ≥75 years (odds ratio [OR] 2.387, 95% confidence interval [CI] 1.416 to 4.025, p = 0.001), presence of CKD (OR 2.255, 95% CI 0.970 to 7.413, p = 0.054), and major bleeding (OR 4.934, 95% CI 1.753 to 13.884, p = 0.002; Table 4 ).
| Variable | Male (n = 597) | Female (n = 597) | p Value |
|---|---|---|---|
| Clinical outcomes | |||
| Major adverse cardiac events | 37 (6.2%) | 28 (4.7%) | 0.308 |
| All-cause mortality | 13 (2.2%) | 17 (2.8%) | 0.580 |
| Cardiac death | 9 (1.5%) | 13 (2.2%) | 0.520 |
| Myocardial infarction | 3 (0.5%) | 1 (0.2%) | 0.374 |
| Target vessel revascularization | 22 (3.7%) | 11 (1.8%) | 0.076 |
| Stroke | 1 (0.2%) | 2 (0.3%) | 0.625 |
| Safety outcome | |||
| Major bleeding | 2 (0.3%) | 18 (3.2%) | <0.001 |
| Combination of safety and efficacy | 39 (6.5%) | 40 (6.7%) | 0.908 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


