Patients with diabetes mellitus (DM) presenting with acute myocardial infarction (AMI) have worse outcomes versus those without DM. Comparative contemporary data in patients presenting with AMI with insulin-requiring diabetes mellitus (IRDM), noninsulin-requiring diabetes mellitus (NIRDM), and newly identified DM (hemoglobin A1C level >6.5%) versus patients without DM are limited. This observational study from the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network—Get with the Guidelines (ACTION Registry-GWTG consisted of 243,861 patients with AMI from 462 US sites identified from January 2007 to March 2011 entered into the registry. Clinical characteristics, management, and in-hospital outcomes were analyzed. Patients with DM with non–ST-segment elevation myocardial infarction (NSTEMI; n = 53,094, 35%) were less likely to undergo diagnostic angiography or revascularization, whereas those with ST-segment elevation myocardial infarction (STEMI) (n = 21,507, 23%) were less likely to undergo reperfusion therapy compared with patients without DM. There was an increased adjusted risk of in-hospital mortality in the DM group in both the NSTEMI (odds ratio [OR] 1.14, 95% confidence interval [CI] 1.06 to 1.22) and STEMI (OR 1.17, 95% CI 1.07 to 1.27) population. In patients with DM, the risk-adjusted in-hospital mortality was higher in patients with IRDM than those with NIRDM in the NSTEMI group (OR 1.12, 95% CI 1.01 to 1.24) but not in the STEMI group (OR 1.12, 95% CI 0.95 to 1.32). Newly diagnosed patients with DM presenting with AMI had similar unadjusted in-hospital outcomes compared with patients without DM. In conclusion, patients with DM presenting with AMI have a higher mortality risk than patients without DM. In patients with DM, those with IRDM presenting with NSTEMI had an increased mortality than those with NIRDM.
Highlights
- •
Patients with diabetes with myocardial infarction have higher mortality than patients without diabetes.
- •
Mortality was higher in insulin-requiring patients with diabetes in non-ST elevation MI.
- •
Newly diagnosed patients with diabetes had similar in-hospital outcomes compared with patients without diabetes.
Previous studies conducted over 10 years ago including the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO-I), the Organization to Assess Strategies for Ischemic Syndromes (OASIS) registry, and the Global Registry of Acute Coronary Events (GRACE) registry revealed that patients with diabetes mellitus (DM) presenting with acute coronary syndrome were at increased risk of in-hospital morbidity and mortality. In 2010, the American Diabetes Association (ADA) added hemoglobin A1C [HA1C] level >6.5% as another criteria for diagnosis of DM. No relevant information exists about this group of patients when presenting with acute myocardial infarction (AMI). Thus, the aim of this study was to compare the clinical characteristics, management, and in-hospital outcomes of patients with versus without DM, insulin-requiring diabetes mellitus (IRDM) versus noninsulin-requiring diabetes mellitus (NIRDM), and newly diagnosed DM versus without DM presenting with AMI in contemporary practice.
Methods
Data for this study were obtained from the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network—Get with the Guidelines (ACTION Registry-GWTG), a nationwide, ongoing, voluntary quality improvement registry sponsored by the American College of Cardiology and the American Heart Association (AHA) that focuses exclusively on patients with ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation myocardial infarction (NSTEMI). Details of the design and conduct of the ACTION Registry-GWTG have been previously described. Definitions for the data elements of ACTION Registry-GWTG are available at https://www.ncdr.com/webncdr/action/home/datacollection . The Duke Clinical Research Institute serves as the data coordinating center to analyze de-identified data for research purposes. The individual institutional review boards of each reporting hospitals approved participation in ACTION Registry-GWTG. Because all data are abstracted retrospectively and anonymously without unique patient identifiers, institutional review boards by policy waive the need for patient’s informed consent.
Data include patients enrolled from January 1, 2007, to March 31, 2011. The original study population included 289,322 patients with AMI enrolled at 609 hospitals across the United States. A total of 45,461 patients were excluded, and exclusions were (listed sequentially) as follows: (1) patients in centers using limited data collect form (n = 21,717), (2) patients in hospitals without percutaneous coronary intervention (PCI) capability (n = 12,164 in 80 sites), (3) patients with missing shock status or shock on presentation (n = 11,202), and (4) patients with missing diabetes status (n = 378). Our final analysis population consisted of 243,861 patients from 462 sites (150,292 patients with NSTEMI and 93,569 patients with STEMI).
History of DM status was identified using the data collect form as “no” for absent and “yes” for present and was defined as patients who had DM in their medical history and also those on any anti-DM therapy. DM therapy was defined as none, diet, oral medications, insulin requiring, and other before hospital presentation. IRDM was defined as patients with DM on insulin therapy, and NIRDM was defined as patients with DM on oral medications. Newly diagnosed DM was defined as patients who did not have a history of DM but were found to have an initial HA1C level >6.5% on presentation, whereas the comparison group, no-DM, was defined as patients without DM having an initial HA1C level ≤6.5%. Major bleeding was defined as a decrease of ≥4 g/dl of absolute hemoglobin (Hb) (baseline to nadir), intracranial hemorrhage, documented or suspected retroperitoneal bleed, any red cell blood transfusion with a baseline Hb ≥9 g/dl, or any red cell transfusion with a baseline Hb <9 g/dl and a suspected bleeding event. Bleeding in patients with coronary artery bypass surgery (CABG) was included as a bleed only if it occurred before surgery. Bleeding during or after surgery was not included in the bleeding definition.
Patient baseline characteristics, treatment pattern, and in-hospital clinical outcomes were compared between (1) patients with and without DM, (2) NIRDM and IRDM, and (3) HA1C levels ≤6.5% and >6.5% stratified by NSTEMI and STEMI. Continuous variables were presented as medians with 25th and 75th percentiles, and categorical variables were expressed as percentages. The Wilcoxon rank-sum test was used to compare continuous variables, and the chi-square test was used to compare categorical variables.
To evaluate the relation between in-hospital mortality and DM in the STEMI and NSTEMI cohort, logistic generalized estimating equation method with exchangeable working correlation matrix was used to account for within-hospital clustering because patients at the same hospital are more likely to have similar outcomes relative to patients at other hospitals (i.e., within-center correlation for outcomes). This method produces estimates similar to those from ordinary logistic regression, but variances are adjusted for the correlation of outcomes within a hospital. Variables used for in-hospital mortality adjustment were derived from the validated ACTION Registry-GWTG in-hospital mortality model. Adjustments included age, gender, race, weight, previous peripheral arterial disease, hypertension, current/recent smoking, dyslipidemia, previous PCI, previous CABG, previous MI, previous heart failure (HF), previous stroke, insurance status, home medications use (aspirin, clopidogrel, warfarin, β blocker [BB], statin, angiotensin-converting enzyme inhibitor [ACE-I], angiotensin-II receptor blocker, aldosterone receptor antagonist, and non-statin lipid-lowering drugs), systolic blood pressure on presentation, heart rate on presentation, HF on admission, electrocardiographic findings, initial Hb, initial troponin ratio, and initial serum creatinine. In addition, a test interaction between DM and electrocardiographic findings (e.g., STEMI and NSTEMI) was explored. Furthermore, same analyses were repeated for IRDM and NIRDM in patients with a history of DM. A p value <0.05 was considered statistically significant for all tests. All statistical analyses were performed using SAS, version 9.3, software (SAS Institute, Cary, North Carolina).
Results
In patients with NSTEMI and STEMI, 53,094 (35%) and 21,507 (23%) patients had DM, respectively. Patients with DM in both AMI groups were older women, had a higher BMI, and tended to have more cardiac risk factors than patients without DM. More patients in the DM group had a history of MI, stroke, and HF than patients in the no-DM group. Patients with DM were less likely to be current/recent smokers than patients without DM in both AMI groups, and they presented with lower initial low-density lipoprotein (LDL) levels; however, they had a lower high-density lipoprotein (HDL) and higher triglyceride levels. Patients with DM with NSTEMI and STEMI were more likely to be on aspirin, clopidogrel, BB, ACE-I, angiotensin-II receptor blocker, and statins at home than patients without DM ( Table 1 ).
| Characteristics | NSTEMI ( n = 150,292) | STEMI ( n = 93,569) | ||
|---|---|---|---|---|
| No DM ( n = 97,198) | DM ( n = 53,094) | No DM ( n = 72,062) | DM ( n = 21,507) | |
| Age (years) † | 66 (55, 78) | 68 (59, 77) | 59 (51, 70) | 62 (54, 72) |
| Male | 63.6% | 58.1% | 72.3% | 64.5% |
| Hypertension ‡ | 69.6% | 89.3% | 57.1% | 82.4% |
| Current/recent smoker | 33.9% | 23.3% | 46.2% | 34.9% |
| Dyslipidemia ‡ | 56.0% | 74.9% | 47.0% | 69.4% |
| Prior myocardial infarction | 24.1% | 37.1% | 16.9% | 26.8% |
| Prior stroke | 7.3% | 13.7% | 4.0% | 8.2% |
| Prior heart failure | 11.4% | 26.1% | 3.5% | 9.8% |
| Home medications | ||||
| Aspirin | 43.8% | 57.5% | 30.0% | 43.3% |
| Clopidogrel | 13.1% | 25.8% | 7.3% | 14.7% |
| Beta-blocker | 37.1% | 56.3% | 23.5% | 38.8% |
| Angiotensin converting enzyme inhibitor | 25.4% | 42.9% | 17.6% | 36.7% |
| Angiotensin II receptor blocker | 9.7% | 16.3% | 6.8% | 12.7% |
| Statin | 35.8% | 57.9% | 25.2% | 45.8% |
| Initial glomerular filtration rate among non-dialysis patients (MDRD) | 72.0 (55.6, 88.5) | 60.5 (42.4, 80.3) | 74.9 (61.1, 90.5) | 71.3 (53.3, 90.0) |
| Initial hemoglobin A1C (%) | 5.8 (5.5, 6.2) | 7.3 (6.4, 8.7) | 5.8 (5.5, 6.2) | 7.6 (6.6, 9.5) |
| Total cholesterol (mg/dL) | 167 (140, 199) | 153 (125, 186) | 170 (143, 199) | 160 (130, 193) |
| High density lipoprotein (mg/dL) | 38 (31, 47) | 35 (29, 43) | 36.0 (30.0, 44.0) | 34.0 (29.0, 41.0) |
| Low density lipoprotein (mg/dL) | 100.7 (76.0, 128.0) | 84 (62, 112) | 104 (81, 130) | 91 (67, 119) |
| Triglycerides (mg/dL) | 114 (79, 170) | 131 (88, 202) | 119 (82, 176) | 137 (92, 210) |
| Characteristics | NSTEMI ( n = 150,292; 62%) | STEMI ( n = 93,569; 38%) | ||
|---|---|---|---|---|
| No DM ( n = 97,198) | DM ( n = 53,094) | No DM ( n = 97,198) | DM ( n = 53,094) | |
| Medications within 24 hrs | ||||
| Aspirin | 97.2% | 96.3% | 98.7% | 98.5% |
| Clopidogrel | 58.0% | 56.2% | 84.8% | 82.1% |
| Beta-blockers § | 89.0% | 88.9% | 93.5% | 93.1% |
| Angiotensin converting enzyme inhibitor | 40.2% | 46.2% | 54.6% | 56.3% |
| Angiotensin II receptor blocker | 7.1% | 12.4% | 4.0% | 7.8% |
| Statin | 59.3% | 62.4% | 72.0% | 70.5% |
| Glycoprotein IIb/IIIa inhibitor | 38.0% | 28.9% | 67.7% | 63.4% |
| Discharge medications | ||||
| Aspirin | 97.4% | 96.7% | 98.8% | 98.1% |
| Clopidogrel | 71.6% | 71.7% § | 85.6% | 83.5% |
| Beta-blocker | 95.2% | 95.7% | 97.4% | 97.2% § |
| Angiotensin converting enzyme inhibitor | 60.6% | 65.1% | 74.0% | 75.3% |
| Angiotensin II receptor blocker | 9.8% | 16.6% | 6.5% | 12.1% |
| Statin | 88.5% | 88.8% § | 94.3% | 93.4% |
| In-hospital procedures | ||||
| Diagnostic cath | 81.3% | 74.6% | 95.1% | 93.2% |
| Three-vessel coronary artery disease | 31.0% | 43.5% | 25.2% | 34.9% |
| Left ventricular ejection fraction < 25% | 4.5% | 6.8% | 3.7% | 5.9% |
| In-hospital percutaneous coronary intervention (non ST segment elevation myocardial infarction) or primary percutaneous coronary intervention (ST segment elevation myocardial infarction) | 48.8% | 41.1% | 84.1% | 82.6% |
| Coronary artery bypass graft surgery | 10.8% | 11.5% | 6.1% | 7.8% |
| Reperfusion strategy | ||||
| Overall reperfusion (ST segment elevation myocardial infarction) or revascularization in (non ST segment elevation myocardial infarction) | 58.9% | 51.9% | 94.4% | 92.2% |
| Thrombolytic therapy (ST segment elevation myocardial infarction) | NA | NA | 11.7% | 10.9% |
| Medically managed (non ST segment elevation myocardial infarction) | 18.2% | 24.7% | NA | NA |
∗ All comparisons of diabetes mellitus versus no diabetes mellitus were statistically significant unless specified with “§.”
† Median (25th and 75th percentiles).
‡ History of hypertension and dyslipidemia as reported by the patients on admission.
Patients with DM were more likely to have more extensive coronary artery disease (CAD) and lower left ventricular (LV) ejection fraction compared with patients without DM. Patients with DM were less likely to undergo cardiac catheterization (cath) or PCI but more likely to undergo CABG in both groups than patients without DM ( Table 1 ).
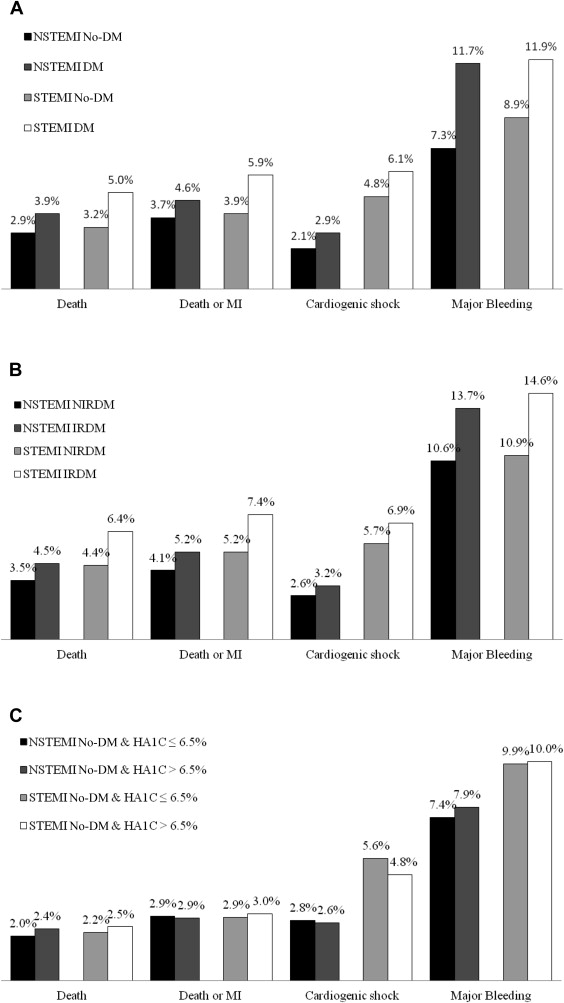
Patients with DM with NSTEMI and STEMI had a significantly higher incidence of in-hospital mortality and major bleeding compared with patients with no DM ( Figure 1 ). The multivariate analysis demonstrated an increased adjusted risk of in-hospital mortality in the DM group than in the no-DM group in both the NSTEMI (odds ratio [OR] 1.14, 95% confidence interval [CI] 1.06 to 1.22) and STEMI (OR 1.17, 95% CI 1.07 to 1.27) population ( Figure 2 ).

In patients with DM with NSTEMI and STEMI, 20,051 (44%) and 5,811 (34%) patients were insulin requiring, respectively. Patients who were IRDM were younger women, nonwhite, and had a slightly higher BMI than patients who were NIRDM. Patients with IRDM also had more cardiac risk factors, were more likely to have HF on presentation, and had a lower initial glomerular filtration rate and a slightly higher HA1C level than patients with NIRDM. Patients with IRDM with NSTEMI and STEMI were more likely to be on aspirin, clopidogrel, BB, and statins at home than patients with NIRDM; ACE-I use at home was similar in both groups ( Table 2 ). Clopidogrel was prescribed similarly on discharge in the NSTEMI groups; however, it was used less frequently in patients with IRDM than in patients with NIRDM in the STEMI group ( Table 2 ).
| Characteristics | NSTEMI ( n = 45,415) | STEMI (n = 17,210) | ||
|---|---|---|---|---|
| NIRDM ( n = 25,364) | IRDM ( n = 20,051) | NIRDM ( n = 11,399) | IRDM ( n = 5,811) | |
| Age (years) † | 69 (60, 78) | 67 (58, 76) | 63 (55, 73) | 62 (53, 72) |
| Male | 60.6% | 54.5% | 67.1% | 57.5% |
| Hypertension ‡ | 89.0% | 90.9% | 83.0% | 85.3% |
| Current/recent smoker | 23.9% | 19.9% | 34.2% | 31.6% |
| Dyslipidemia ‡ | 74.7% | 77.5% | 70.1% | 73.0% |
| Prior myocardial infarction | 33.7% | 43.8% | 25.0% | 33.3% |
| Prior stroke | 12.0% | 16.5% | 7.1% | 11.4% |
| Prior heart failure | 20.5% | 35.4% | 7.7% | 16.0% |
| Home medications | ||||
| Aspirin | 56.1% | 62.9% | 43.8% | 50.1% |
| Clopidogrel | 22.6% | 32.9% | 13.2% | 21.6% |
| Beta-blocker | 53.7% | 64.0% | 38.8% | 47.1% |
| ACE-I § | 45.0% | 44.3% | 39.6% | 41.0% |
| ARB | 16.1% | 18.0% | 13.2% | 15.2% |
| Statin | 58.0% | 63.5% | 48.7% | 52.8% |
| Lab results † | ||||
| Initial glomerular filtration rate among non-dialysis patients (MDRD) | 63.8 (46.6, 82.6) | 52.9 (36.1, 74.3) | 72.2 (55.9, 90.4) | 65.3 (45.2, 86.0) |
| Initial hemoglobin A1C (%) | 7.1 (6.3, 8.2) | 7.9 (6.9, 9.3) | 7.4 (6.5, 9.0) | 8.4 (7.2, 10.1) |
| Total cholesterol (mg/dL) | 153 (126, 185) | 148 (120, 181) | 157 (129, 189) | 156 (127, 192) § |
| High density lipoprotein (mg/dL) | 35 (29, 43) | 35 (29, 43) | 34 (28, 41) | 35 (29, 42) |
| Low density lipoprotein (mg/dL) | 84 (63, 112) | 79 (58, 107) | 88 (66, 115) | 88 (46, 117) § |
| Triglyceride (mg/dL) | 134 (90, 205) | 127 (85, 198) | 139 (94, 213) | 132 (88, 201) |
| Medications within 24 hrs | ||||
| Aspirin | 96.5% | 95.9% | 98.8% | 97.9% |
| Clopidogrel | 56.1% | 56.2% § | 83.1% | 80.4% |
| Medications within 24 hrs | ||||
| Beta-blocker | 89.0% | 88.8% § | 93.4% | 92.1% |
| Angiotensin converting enzyme inhibitor | 47.5% | 44.8% | 57.5% | 53.3% |
| Angiotensin II receptor blocker | 12.1% | 13.8% | 7.9% | 9.6% |
| Statin | 62.9% | 62.7% § | 72.2% | 68.1% |
| Glycoprotein IIb/IIIa inhibitor | 31.0% | 24.8% | 64.7% | 59.9% |
| Discharge medications (%) | ||||
| Aspirin | 97.0% | 96.4% | 98.4% | 97.5% |
| Clopidogrel | 71.9% | 72.3% § | 84.3% | 81.6% |
| Beta-blocker § | 95.9% | 95.7% | 97.4% | 97.1% |
| Angiotensin converting inhibitor | 66.4% | 63.2% | 76.0% | 72.4% |
| Angiotensin II receptor blocker | 16.1% | 18.5% | 12.2% | 14.8% |
| Statin | 89.1% | 88.8% § | 94.3% | 91.7% |
| In-hospital procedures (%) | ||||
| Diagnostic cath | 77.9% | 69.9% | 94.2% | 90.9% |
| Three-vessel coronary artery disease | 42.9% | 46.3% | 34.5% | 37.6% |
| Left ventricular ejection fraction <25% | 6.0% | 7.9% | 5.4% | 7.2% |
| In-hospital percutaneous coronary intervention (non ST segment elevation myocardial infarction) or primary percutaneous coronary intervention (ST segment elevation myocardial infarction) | 43.7% | 37.1% | 82.9% | 82.0% |
| Coronary artery bypass surgery graft surgery | 12.6% | 9.8% | 7.6% | 7.7% § |
| Reperfusion strategy | ||||
| Overall reperfusion (ST segment elevation myocardial infarction) or revascularization (non ST segment elevation myocardial infarction) | 55.6% | 46.4% | 92.9 | 90.3 |
| Thrombolytic therapy (ST segment elevation myocardial infarction) | NA | NA | 11.3 | 9.2 |
| Medically managed (non ST segment elevation myocardial infarction) | 21.5% | 29.3% | NA | NA |
∗ All comparisons of insulin-requiring versus noninsulin-requiring diabetes mellitus were statistically significant unless specified with “§.”
† Median (25th and 75th percentiles).
‡ History of hypertension and dyslipidemia as reported by the patients on admission.
Patients with IRDM were more likely to have 3-vessel CAD and LV ejection fraction <25% than patients with NIRDM in both the AMI groups. Patients with IRDM presenting with NSTEMI were more likely to be medically managed. More patients in the NIRDM group with STEMI received thrombolytics compared with the IRDM group, whereas they tended to undergo primary PCI with similar frequency. CABG surgery was performed more often in the patients with IRDM versus patients with IRDM in the NSTEMI group ( Table 2 ).
Regardless of the type of AMI, patients with IRDM had a higher in-hospital mortality rate and major bleeding events than patients with NIRDM ( Figure 1 ). The multivariate analysis showed that risk-adjusted in-hospital mortality was higher in IRDM than patients with NIRDM in the NSTEMI group (OR 1.12, 95% CI 1.01 to 1.24) but not in the STEMI group (OR 1.12, 95% CI 0.95 to 1.32; Figure 2 ).
In patients without DM presenting with NSTEMI and STEMI in whom HA1C levels were available, 3,252 (15%) and 2,591 (14%) patients were newly diagnosed with DM, respectively. Newly diagnosed patients with DM in both AMI groups were less likely to be of white race, had a higher BMI, and were less likely to have dyslipidemia compared with patients without DM. Patients with newly diagnosed DM presented with higher initial LDL levels, slightly lower HDL levels, and higher triglyceride levels than patients without DM ( Table 3 ).
| Characteristics | NSTEMI (n = 22,166) | STEMI (n = 18,916) | ||
|---|---|---|---|---|
| HA1C ≤ 6.5% ( n = 18,914) | HA1C > 6.5% (n = 3,252) | HA1C ≤ 6.5% (n = 16,325) | HA1C > 6.5% (n = 2,591) | |
| Age (years) † | 63 (54, 74) | 63 (53, 73) | 59 (51, 68) | 58 (51, 66) |
| Male ‡ | 68.4% | 68.5% | 74.2% | 74.9% |
| Hypertension ‡ § | 67.7% | 67.5% | 56.2% | 55.6% |
| Current/recent smoker ‡ | 38.3% | 38.5% | 48.3% | 48.1% |
| Dyslipidemia § | 56.1% | 50.8% | 47.6% | 40.6% |
| Prior myocardial infarction ‡ | 20.5% | 20.5% | 14.3% | 14.1% |
| Prior stroke ‡ | 6.1% | 6.2% | 3.3% | 2.9% |
| Prior heart failure | 7.7% | 9.6% | 2.7% | 2.7% ‡ |
| Home medications (%) | ||||
| Aspirin ‡ | 40.1% | 39.0% | 27.6% | 26.0% |
| Clopidogrel ‡ | 9.8% | 10.4% | 5.3% | 6.0% |
| Beta-blocker ‡ | 31.4% | 32.9% | 20.9% | 20.8% |
| Angiotensin converting enzyme inhibitor ‡ | 23.6% | 22.4% | 16.1% | 15.7% |
| Angiotensin II receptor blocker | 9.0% | 9.0% | 6.6% | 6.0% ‡ |
| Statin | 32.3% | 30.5% ‡ | 22.9% | 19.1% |
| Lab results † | ||||
| Initial glomerular filtration rate among non-dialysis patients (MDRD) | 74 (58.5, 89.6) | 75.1 (58.6, 91.6) | 75.3 (62, 90.7) | 78.9 (64.5, 94.3) |
| Initial hemoglobin A1C (%) | 5.8 (5.5, 6.0) | 7.2 (6.8, 8.5) | 5.7 (5.5, 6.0) | 7.5 (6.8, 9.6) |
| Total cholesterol (mg/dL) | 170 (142, 201) | 181 (149, 215) | 171 (145, 201) | 182 (152, 215) |
| High density lipoprotein (mg/dL) | 37 (31, 46) | 34 (28, 41) | 36 (30, 44) | 33 (28, 40) |
| Low density lipoprotein (mg/dL) | 104 (79, 131) | 109 (80, 137) | 106 (83, 132) | 111 (85, 137) |
| Triglyceride (mg/dL) | 116 (80, 173) | 159 (104, 240) | 119 (81, 176) | 158 (107, 242) |
| Aspirin ‡ | 97.9% | 97.9% | 98.9% | 98.9% |
| Clopidogrel ‡ | 56.4% | 56.7% | 83.5% | 84.4% |
| Medications within 24 hrs (%) | ||||
| Beta-blocker | 90.8% | 92.0% | 94.3% | 95.3% |
| Angiotensin converting enzyme inhibitor | 42.2% | 45.3% | 57.1% | 61.5% |
| Angiotensin II receptor blocker ‡ | 6.2% | 6.8% | 3.7% | 3.9% |
| Statin | 63.5% | 62.2% ‡ | 76.7% | 74.6% |
| Glycoprotein IIb/IIIa inhibitor ‡ | 42.4% | 42.3% | 69.6% | 70.1% |
| Discharge medications (%) | ||||
| Aspirin ‡ | 98.1% | 98.1% | 99.0% | 98.8% |
| Clopidogrel | 66.1% | 68.3% | 81.8% | 83.4% |
| Beta-blocker ‡ | 96.3% | 96.5% | 97.8% | 98.0% |
| Angiotensin converting enzyme inhibitor | 62.4% | 66.3% | 75.9% | 78.6% |
| Angiotensin II receptor blocker ‡ | 8.3% | 8.6% | 5.8% | 6.5% |
| Statin | 92.5% | 91.9% ‡ | 95.9% | 94.8% |
| In-hospital procedures (%) | ||||
| Diagnostic cath | 90.0% | 87.2% | 97.9% | 97.3% ‡ |
| Three-vessel coronary artery disease | 40.4% | 41.3% ‡ | 29.4% | 32.2% |
| Left ventricular ejection fraction <25% | 4.0% | 5.7% | 3.5% | 4.2% ‡ |
| In-hospital percutaneous coronary intervention (non ST segment elevation myocardial infarction) or primary percutaneous coronary intervention (ST segment elevation myocardial infarction) | 45.5% | 47.6% | 82.9% | 83.4% ‡ |
| Coronary artery bypass graft surgery | 28.1% | 21.9% | 12.8% | 11.1% |
| Reperfusion strategy (%) | ||||
| Overall reperfusion in ST segment elevation myocardial infarction, revascularization in non ST segment elevation myocardial infarction | 71.9% | 68.4% | 94.4% | 94.7% ‡ |
| Thrombolytic therapy (ST segment elevation myocardial infarction) | NA | NA | 12.7% | 12.4% § |
| Medically managed (non ST segment elevation myocardial infarction) | 9.4% | 12.2% | NA | NA |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


