Cardiovascular risk persists despite intensive low-density lipoprotein cholesterol (LDL-C) reduction using statins. High-density lipoprotein (HDL-C) is inversely associated with coronary artery disease (CAD) that is independent of LDL-C levels. C-reactive protein (CRP) is an established marker of inflammation that can impair the protective function of HDL-C: however, the impact of inflammation on the association between HDL-C and long-term outcomes in patients with CAD under statin therapy remains uncertain. We prospectively enrolled 3,507 consecutive patients with CAD who underwent a first percutaneous coronary intervention (PCI) from 1997 to 2011 at our institution. We stratified 1,682 patients (48%) who had been treated with statin at the time of PCI into 4 groups according to HDL-C levels (cutoffs of 40 and 50 mg/dl for men and women, respectively) and a CRP cutoff of 2 mg/dl: (1) high HDL-C/low CRP, (2) high HDL-C/high CRP, (3) low HDL-C/low CRP, and (4) low HDL-C/high CRP comparing the rates of all-cause death among them. The median follow-up period was 1,985 days (interquartile range 916 to 3,183 days). During this period, 197 patients (11.7%) died because of cardiac death (n = 58), carcinoma (n = 61), stroke (n = 10), and other causes (n = 69). The rates of all-cause death significantly differed among the groups (log-rank test, p <0.0001). In multivariate Cox hazard regression analyses, low HDL-C with high CRP levels remained significantly associated with a higher rate of all-cause death even after adjustment for other co-variates (hazard ratio 2.38, 1.59 to 3.61, p <0.0001). Low HDL-C together with elevated CRP levels is significantly associated with long-term outcomes in patients who received statin therapy after PCI.
Clinical trials have shown that statins significantly reduce cardiovascular events in patients with coronary artery disease (CAD). However, cardiovascular risk persists despite intensive low-density lipoprotein cholesterol (LDL-C) reduction with statins. High-density lipoprotein (HDL-C) is inversely associated with CAD that is independent of LDL-C levels. Thus, low HDL-C is a residual risk factor for CAD independently of LDL-C even after statin therapy. Atherosclerosis is fundamentally an inflammatory condition and C-reactive protein (CRP) is an inflammatory biomarker and an independent predictor of adverse cardiovascular events in patients with CAD, and it adds to the risk conferred by LDL-C. Inflammation reduces the HDL-C concentration and possibly compromises the anti-inflammatory functions of HDL-C. Epidemiologic associations between CRP and HDL-C and CAD under statin therapy have not been evaluated and whether elevated CRP levels attenuate the protective feature of HDL-C against CAD is obscure. From this perspective, we evaluated whether interactions between HDL-C and CRP affect long-term clinical outcomes in patients with CAD after coronary intervention.
Methods
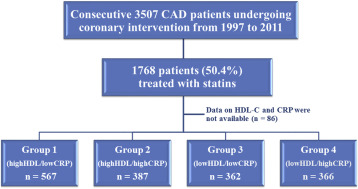
We analyzed data from a single-center, observational study of patients who underwent percutaneous coronary intervention (PCI) at our institution from January 1997 to December 2011. We included only data from patients with CAD who were treated with statin at the time of PCI. Missing HDL-C and CRP data were excluded from the study. Of 3,507 patients who underwent scheduled PCI during the study period, we analyzed data from 1,682 eligible patients with CAD who were treated with statins. The patients were assigned to 4 groups on the basis of preprocedural HDL-C levels and CRP values. The cutoffs for HDL-C were 40 mg/dl for men and 50 mg/dl for women and that for CRP was 2 mg/dl. Group 1 comprised those with higher HDL-C and lower CRP levels, and group 4 comprised those with lower HDL-C and higher CRP levels. Groups 2 and 3 comprised patients with higher and lower levels of both components, respectively ( Figure 1 ).
Demographic data and information about coronary risk factors, medications, revascularization procedure-related factors, and co-morbidities were prospectively collected and analyzed. Blood samples were collected during the early morning after an overnight fast, and blood pressure (BP) was measured at the time of admission. Patients with BP >140/90 mm Hg or under antihypertensive medication were considered hypertensive. Diabetes mellitus was defined as either hemoglobin A1c (HbA1c) ≥6.5% or under medication with insulin or oral hypoglycemic drugs. The estimated HbA1c (%) was calculated as the National Glycohemoglobin Standardization Program equivalent value (%) using the formula HbA1c (%) = 1.02 × HbA1c (JDS; %) + 0.25%. We defined chronic kidney disease (CKD) as an estimated glomerular filtration rate (eGFR) of <60 ml/min/1.73 m 2 and calculated the eGFR on the basis of the modification of diet in renal disease equation modified with a Japanese coefficient using baseline serum creatinine. Levels of serum high-sensitive CRP (hs-CRP) were measured using a validated immunoassay and an autoanalyzer. Other markers were determined by routine laboratory methods.
Written informed consent was obtained from all patients before undergoing coronary intervention. This study proceeded under the approval of our institutional review board in accordance with the Declaration of Helsinki.
The primary outcome was all-cause death. Clinical follow-up comprised analyses of office visit charts and responses to questionnaires sent to patients or their families and telephone contact. Mortality data were collected from the medical records of patients who died or who were treated at our institution, and details and causes of death were obtained from other hospitals where patients had been admitted.
Quantitative data are expressed as means ± standard deviation, and categorical variables are presented as frequencies. The distribution of continuous variables was visually assessed from frequency histograms. Continuous variables across groups were compared using a one-way analysis of variance followed by post hoc analysis using Dunnett test for multiple comparisons. Group 1, comprising patients with higher HDL-C and lower CRP levels, served as a control group for post hoc analyses. Categorical variables were compared using the chi-square test or Fisher’s exact probability test. Unadjusted cumulative event rates were estimated using Kaplan–Meier curves and compared across the groups using log-rank test. Hazard ratios and 95% confidence intervals for each variable were calculated using a Cox proportional hazards model. Predictors of all-cause death were determined by multivariate Cox regression analysis. Variables with p <0.05 in the univariate model in addition to age and gender were included in the multivariate analysis. Values with p <0.05 were considered to indicate statistically significant difference. All data were analyzed using JMP version 9.0 for Windows (SAS Institute, Cary, North Carolina).
Results
Significant differences were present in gender, prevalence of metabolic syndrome, acute coronary syndrome, and CKD ( Table 1 ). Lower left ventricular ejection fraction (LVEF), higher LDL-C, and fasting blood glucose levels were observed in groups 2 and 4 compared with group 1. The median follow-up period was 1,985 (interquartile range 916 to 3183) days, and prognostic data were fully documented during the entire follow-up period. During the follow-up, 198 patients (11.7%) died because of cardiac death (n = 58), carcinoma (n = 61), stroke (n = 10), and other causes (n = 69). Figure 2 shows the cumulative event-free survival curves for all-cause death among the groups. The curves of each group significantly differed (log-rank test, p <0.0001). Variables with p <0.05 in univariate analysis comprised age, multivessel disease, acute coronary syndrome, CKD, low LVEF, body mass index, diastolic blood pressure, and fasting blood glucose. Low HDL-C with high CRP levels (group 4) remained significantly associated with higher rate of all-cause death even after adjustment for other covariates ( Table 2 ).
| HDL-C /hsCRP Variable | Group 1 high/low (n = 567) | Group 2 high/high (n = 387) | Group 3 low/low (n = 362) | Group 4 low/high (n = 366) | P value |
|---|---|---|---|---|---|
| Age (years) | 65.3±9.4 | 64.5±11.0 | 64.5±9.8 | 64.1±11.0 | 0.27 |
| Men | 485 (85.5%) | 336 (86.8%) | 279 (77.1%) | 263 (71.9%) | < 0.0001 |
| Hypertension | 398 (70.2%) | 269 (69.5%) | 266 (73.5%) | 267 (73.0%) | 0.52 |
| Diabetes mellitus | 245 (43.2%) | 180 (46.5%) | 187 (51.7%) | 178 (48.6%) | 0.08 |
| Metabolic syndrome | 233 (43.2%) | 145 (45.3%) | 202 (57.9%) | 174 (57.6%) | < 0.0001 |
| Current Smoking | 112 (19.8%) | 113 (29.2%) | 93 (25.7%) | 114 (31.2%) | 0.0003 |
| Family History | 169 (29.9%) | 108 (28.1%) | 124 (34.3%) | 118 (32.3%) | 0.26 |
| Triple vessel Disease | 144 (25.8%) | 80 (20.9%) | 93 (26.1%) | 91 (25.1%) | 0.29 |
| Multivessel Disease | 340 (60.9%) | 219 (57.2%) | 219 (61.3%) | 220 (60.6%) | 0.62 |
| Acute coronary syndrome | 118 (20.8%) | 162 (42.1%) | 56 (15.5%) | 101 (27.6%) | < 0.0001 |
| Chronic kidney disease | 129 (22.8%) | 104 (27.0%) | 103 (28.5%) | 130 (35.7%) | < 0.0001 |
| Low left ventricular ejection fraction | 62 (11.9%) | 74 (21.0%) | 41 (12.5%) | 82 (23.9%) | < 0.0001 |
| Left ventricular ejection fraction (%) | 63.0±10.6 | 58.9±13.5* | 62.7±11.1 | 59.7±14.8* | < 0.0001 |
| Body mass index (kg/m 2 ) | 24.0±3.1 | 24.4±3.5 | 24.9±3.2* | 25.0±3.7* | < 0.0001 |
| Systolic blood pressure (mmHg) | 132.3±20.9 | 133.2±21.8 | 133.1±24.6 | 131.3±22.4 | 0.61 |
| Diastolic blood pressure (mmHg) | 72.0±12.8 | 73.4±13.6 | 72.4±11.9 | 71.0±13.1 | 0.12 |
| Low-density lipoprotein cholesterol (mg/dL) | 108.5±33.8 | 118.3±34.9* | 105.2±33.4 | 115.5±37.9* | < 0.0001 |
| High-density lipoprotein cholesterol (mg/dL) | 53.1±13.3 | 51.7±11.1 | 35.5±5.2* | 34.8±5.8* | < 0.0001 |
| Triglyceride (mg/dL) | 128.9±66.3 | 131.5±78.3 | 156.9±83.6* | 148.5±80.5* | < 0.0001 |
| Fasting blood glucose (mg/dL) | 114.6±40.4 | 126.6±50.8* | 112.2±31.8 | 126.2±63.6* | < 0.0001 |
| Hemoglobin A1c (%) | 5.98±1.23 | 6.01±1.23 | 6.19±1.39 | 6.13±1.41 | 0.0404 |
| Medication | |||||
| Aspirin, | 540 (96.3%) | 369 (95.8%) | 348 (96.7%) | 347 (94.8%) | 0.60 |
| Ca-channel blockers | 224 (40.0%) | 133 (34.6%) | 142 (39.4%) | 136 (37.2%) | 0.36 |
| ACE-I/ARBs | 290 (51.7%) | 221 (57.4%) | 197 (54.7%) | 198 (54.1%) | 0.38 |
| β-Blockers | 276 (49.2%) | 190 (49.4%) | 216 (60.0%) | 191 (52.2%) | 0.0072 |
| Culprit of vessels | 0.21 | ||||
| Left main trunk or proximal of Left ascending artery | 117 (20.6%) | 96 (24.8%) | 68 (18.8%) | 76 (20.8%) | 0.22 |
| High sensitive C-reactive protein (mg/dL) | 0.07±0.05 | 1.53±3.48* | 0.08±0.05 | 1.22±2.04* | < 0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


