Coronary chronic total occlusions (CTOs) have been associated with higher mortality in patients with ischemic cardiomyopathy and implantable cardioverter defibrillators (ICDs); yet the impact of CTO revascularization on subsequent clinical outcomes has not been studied. We evaluated the clinical characteristics and outcomes of patients with ischemic cardiomyopathy who also received an ICD for primary prevention of sudden death at the Dallas VA Medical Center from January 2002 to December 2013. On the basis of coronary angiography performed before device implantation, patients were divided into 3 groups: no CTOs, revascularized CTOs (with percutaneous coronary intervention or surgery), and unrevascularized CTOs. Primary and secondary outcomes were all-cause mortality and appropriate ICD therapy for sustained ventricular arrhythmias. A total of 307 patients (mean age 64.3 ± 8.1 years, 100% men) were included in the study. At least 1 CTO was present in 213 patients (69%) and was revascularized in 99 patients (32%). During a median follow-up of 4.1 years, 51 patients (17%) died and 98 (32%) had at least 1 episode of sustained ventricular arrhythmia. Mortality and incidence of ventricular arrhythmias were similar in the 3 study groups in both univariate and multivariate analyses. In conclusion, CTOs are commonly found in patients with ischemic cardiomyopathy. In contrast to previous studies, the presence of a CTO was not associated with higher mortality or incidence of ventricular arrhythmias. In addition, revascularization of CTOs was not associated with improved outcomes in this high-risk cohort.
Coronary revascularization of chronically ischemic, yet viable myocardium, has the potential to increase regional and global function and decrease ventricular tachyarrhythmias. We hypothesized that in patients with ischemic cardiomyopathy who had received an implantable cardioverter defibrillator (ICD), unrevascularized chronic total occlusions (CTOs) would be associated with increased risk of death or ventricular arrhythmias as compared with patients with revascularized CTOs or no CTOs.
Methods
We retrospectively reviewed the medical records of 1,201 patients who received an ICD at our institution from 2002 to 2013. Patient baseline demographics and clinical characteristics were collected. Echocardiographic data including left ventricular ejection fraction (LVEF), left atrial size, and presence and degree of mitral regurgitation and the electrocardiogram before ICD implantation were also reviewed. Only patients who had undergone coronary angiography before ICD implantation were included in the present study.
CTOs were defined as 100% occlusions of a major epicardial artery (left anterior descending, circumflex, and right coronary artery) with Thrombolysis in Myocardial Infarction flow grade 0 and estimated duration of at least 3 months. Renal dysfunction was defined as estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m 2 , as calculated using the Modification of Diet in Renal Disease formula. Medication intake at the time of events (arrhythmias or death) was collected, including use and type of β blockers, angiotensin-converting enzyme inhibitors, aldosterone antagonist inhibitors, and antiarrhythmic agents.
The type of ICD implanted, such as single-chamber, dual-chamber, or cardiac resynchronization devices, was collected. All devices were implanted transvenously without any epicardial leads being placed. We collected all postplacement ICD testing results, including lead sensing and pacing and defibrillation thresholds.
The records of all ICD follow-up visits were reviewed, and information was collected on New York Heart Association (NYHA) class, sensing and pacing thresholds, incidence of nonsustained ventricular arrhythmias, and appropriate and inappropriate ICD therapies (including antitachycardia pacing [ATP] and cardioversions). The ICD interrogation was reviewed by an electrophysiologist to determine whether each event was appropriate or inappropriate. Inappropriate therapy was defined as either ATP or defibrillation for events not associated with ventricular tachycardia or fibrillation, such as atrial tachyarrhythmias or T-wave oversensing. Only appropriate ICD therapies were included in the follow-up event analysis.
The primary end point of the study was the incidence of all-cause death from the time of ICD implantation. The secondary end point was the incidence of sustained ventricular arrhythmias and appropriate ICD therapies (either ATP or shock).
Continuous parameters were presented as mean ± standard deviation or median (interquartile range) and compared using the unpaired Student t test or the Wilcoxon rank-sum test. Nominal variables were listed as percentages and compared using the chi-square test or Fisher’s exact test, as appropriate. The incidence of death, ventricular arrhythmias, and appropriate ICD therapies was calculated using the Kaplan–Meier method and compared using the log-rank test. Cox proportional hazards models were used to determine the risk of events during follow-up after adjusting for various clinical parameters. All statistical analyses were performed using SAS software, version 9.2 (SAS Institute Inc., Cary, North Carolina). A 2-sided p value of <0.05 was considered statistically significant.
Results
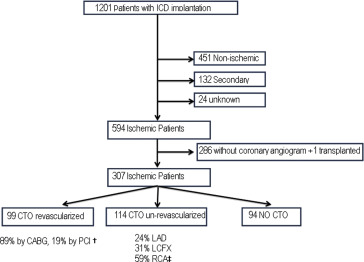
Of 1,201 patients who received an ICD at our institution during the study period, we excluded 451 patients with nonischemic cardiomyopathy, 132 patients with secondary prevention indications (i.e., history of ventricular arrhythmias or resuscitated sudden cardiac death), 24 patients with uncertain cause of cardiomyopathy, and 1 patient who underwent cardiac transplantation ( Figure 1 ). Of the remaining 593 patients, we excluded 286 patients, who did not have assessment of coronary anatomy before ICD implantation. The 307 patients that were included in the study were further classified on the basis of their coronary anatomy into those with no CTOs, those with revascularized CTOs (either with percutaneous coronary intervention [PCI] or with coronary artery bypass graft surgery [CABG]), and those with unrevascularized CTOs ( Figure 1 ).
The baseline clinical, device, and echocardiographic characteristics of the 307 study patients are presented in Table 1 . Median age for all groups was 63 (interquartile range 59 to 69) years, and all patients were men. Mean LVEF was 29.3 ± 6.6%, 170 patients (55%) had diabetes, 243 patients (79%) had previous myocardial infarction, and 109 patients (36%) had renal dysfunction. Most patients received a single- (51.4%) or dual-chamber (20.2%) ICD, and the remaining 28.4% received a cardiac resynchronization therapy ICD. Of 213 patients with CTOs 114 (54%) were not revascularized.
| Variable | Chronic Total Occlusions | p | ||
|---|---|---|---|---|
| Revascularized (n=99) | Un-revascularized (n=114) | Absent (n=94) | ||
| Age (years) | 64 [60, 69] | 64 [58, 72] | 63 [57,67] | 0.077 |
| Men | 99 (100%) | 114 (100%) | 94 (100%) | n/a |
| BMI (kg/m 2 ) | 29.7 [26.1, 35.3] | 28.9 [25.4, 33.1] | 28.5 [25.1, 33.5] | 0.226 |
| Diabetes mellitus | 55 (56%) | 67 (59%) | 49 (52%) | 0.532 |
| Hypertension | 98 (100%) | 114 (100%) | 94 (100%) | n/a |
| Smoker | 0.285 | |||
| Current | 7 (7%) | 8 (7%) | 13 (14%) | |
| Prior | 85 (87%) | 102 (90%) | 74 (80%) | |
| Renal dysfunction | 40 (40%) | 36 (32%) | 32 (34%) | 0.457 |
| eGFR (mL/min/1.73m 2 ) | 66.6 [53.7, 80.2] | 69.8 [57.0, 81.9] | 68.7 [56.8, 82.2] | 0.489 |
| Number of narrowed coronary arteries | ||||
| 1 | 5 (5%) | 10 (9%) | 28 (30%) | <0.0001 |
| 2 | 16 (16%) | 28 (24%) | 32 (34%) | 0.023 |
| 3 | 78 (79%) | 76 (67%) | 34 (36%) | <0.0001 |
| Left anterior descending artery chronic total occlusion | 22 (40%) | 28 (25%) | ||
| Prior myocardial infarction | 82 (82%) | 97 (85%) | 65 (69%) | 0.012 |
| Prior percutaneous coronary intervention | 43 (43%) | 47 (41%) | 58 (62%) | 0.006 |
| Prior coronary bypass | 85 (86%) | 60 (53%) | 30 (32%) | <0.0001 |
| New York Heart Association | ||||
| Class I | 2 (2%) | 0 (0%) | 0 (0%) | 0.213 |
| Class II | 24 (24%) | 47 (41%) | 39 (41%) | 0.014 |
| Class ≥ III | 73 (74%) | 67 (59%) | 55 (59%) | 0.035 |
| Left ventricle ejection fraction | 30 [25, 33] | 30 [27, 32] | 30 [25, 34] | 0.920 |
| QRS (ms) | 112 [100, 131] | 110 [100, 138] | 106 [92, 122] | 0.038 |
| Device type | ||||
| Single | 47 (47%) | 55 (48%) | 56 (60%) | 0.156 |
| Dual | 22 (22%) | 25 (22%) | 15 (16%) | 0.482 |
| Cardiac resynchronization therapy (CRT) | 30 (30%) | 34 (30%) | 23 (24%) | 0.575 |
| History of non-sustained ventricular tachycardia | 23 (23%) | 41 (36%) | 24 (25%) | 0.089 |
| Forced expiratory volume at one sec /Forced vital capacity | 67% | 68% | 71% | 0.410 |
| Forced expiratory volume at one sec | 72% | 73% | 68% | 0.541 |
| Medications | ||||
| Statin | 92 (93%) | 104 (91%) | 86 (91%) | 0.789 |
| β-blocker | 90 (91%) | 97 (85%) | 86 (91%) | 0.312 |
| ACEI/ARB | 82 (82%) | 95 (83%) | 80 (85%) | 0.908 |
| Aldosterone Inhibitor | 17 (17%) | 15 (13%) | 16 (17%) | 0.668 |
| Anti-arrhythmics | 16 (16%) | 21 (18%) | 12 (13%) | 0.655 |
There were no significant differences in most baseline characteristics between the 3 groups ( Table 1 ). However, patients with CTOs were more likely to have 3-vessel coronary artery disease, previous CABG, and higher NYHA class.
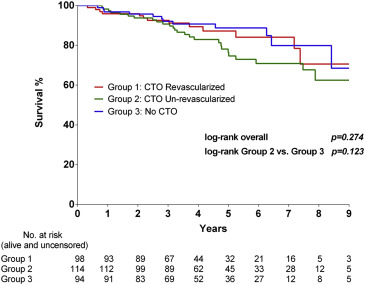
During a median follow-up of 4.1 (interquartile range 3.0 to 6.2) years, 51 of 307 patients (16.6%) died. Mortality rate at 1, 2, and 3 years was 3%, 8%, and 17%, respectively. There was no significant difference in mortality rate between patients with and without CTOs ( Figure 2 ). On univariate analyses, increasing age (p <0.0001), lower eGFR (p=<0.0001), and higher NYHA class (p = 0.0001) were associated with higher mortality ( Table 2 ). However, the presence of a CTO (irrespective of revascularization) was not associated with mortality.