Although Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score based on angiographic scoring system was developed in patients with previous coronary artery bypass grafting (CABG), few data exist regarding its prognostic utility in patients undergoing percutaneous coronary intervention (PCI). We examined 272 patients with previous CABG (217 men; mean age, 70.4 ± 9.7 years) undergoing PCI. Severity of the coronary anatomy was evaluated using CABG-SYNTAX score. The primary end point of this study was cardiovascular death. The baseline CABG-SYNTAX score ranged from 2 to 53.5, with an average of 26.0 ± 10.2. In the index procedures, PCI for the native coronary accounted for nearly all patients (88%). During follow-up (median 4.1 years), 40 cardiovascular deaths had occurred. In multivariate analysis, age >75 years (hazard ratio [HR] 2.82, 95% CI 1.45 to 5.52), left ventricular ejection fraction <40% (HR 2.99, 95% CI 1.39 to 6.07), end-stage renal disease (HR 2.90, 95% CI 1.15 to 6.75), peripheral artery disease (HR 2.20, 95% CI 1.10 to 4.64), and CABG-SYNTAX score >25 (HR 2.37, 95% CI 1.19 to 5.05) were independent predictors of cardiovascular death. After creating a composite risk score in consideration of identified predictors, the freedom from cardiovascular death at 5 years was 98%, 86%, and 58% in the low (0 to 1), medium (2), and high (3 to 5) scores, respectively (p <0.001). The area under the receiver-operating characteristic curve for cardiovascular death for the CABG-SYNTAX and composite risk scores were 0.66 and 0.77, respectively (p <0.05). In conclusion, the combination of angiographic and clinical characteristics is useful for risk stratification in patients with previous CABG undergoing PCI.
Although percutaneous coronary intervention (PCI) for native coronary in patients with previous coronary artery bypass grafting (CABG) is necessary as an advanced technique to treat complex lesions, such as bifurcation, calcification, and total occlusion, recent studies have shown that PCI is feasible for the native coronary artery in patients with previous CABG, compared with PCI for bypass graft. Under these conditions, the angiographic risk score for the coronary artery has been developed for the evaluation of anatomical complexities in patients with previous CABG (CABG-Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery [SYNTAX] score). Moreover, previous studies of the SYNTAX score have demonstrated the importance of combining the anatomical and clinical factors for risk stratification in patients undergoing coronary revascularization. Thus, we hypothesized that the prediction of outcome in these patients would be refined by combining the angiographic and clinical factors. However, few data exist regarding its predictive ability in patients with previous CABG undergoing PCI. Therefore, the purpose of our study was to investigate the predictive ability of the CABG-SYNTAX score on clinical outcome in patients with previous CABG undergoing PCI.
Methods
We reviewed the records of patients with previous CABG who underwent PCI at 2 institutions from November 2006 to October 2014. The local Ethics Committee approved the use of the clinical data for this investigation. The indications for PCI were symptomatic myocardial ischemia or evidence of a positive stress test with either electrocardiogram or nuclear imaging. PCI strategies were determined by the operator for each case. Postprocedural administration of antiplatelet therapy has been described elsewhere. All patients were informed about the risks of the procedure and each patient provided written informed consent.
Left ventricular ejection fraction (EF) was obtained from transthoracic echocardiography or diagnostic left ventriculography. Renal function was expressed as the estimated glomerular filtration rate, calculated using the Modification of Diet in Renal Disease formula, as modified for Japanese patients. Peripheral arterial disease was defined as the presence of lower extremity peripheral artery disease, carotid artery stenosis, or abdominal aortic aneurysm. Lower extremity peripheral artery disease was defined as an ankle-brachial index <0.9 or a history of endovascular or surgical revascularization. The presence of ≥50% carotid stenosis recorded by ultrasonography or a history of endovascular or surgical revascularization was defined as carotid artery stenosis. Abdominal aortic aneurysm was defined as aortic diameter >30 mm or a history of endovascular or surgical repair. The CABG-SYNTAX score was calculated by determining the SYNTAX score of the native coronary and deducting points based on the importance of the diseased coronary segment with a functioning bypass graft anastomosed distally, as proposed previously.
The primary end point of this study was cardiovascular mortality. Clinical information was obtained from a review of the hospital record or by telephone. Death was regarded as being of cardiac origin, unless obvious noncardiac causes could be identified. Myocardial infarction was defined as an increase in serum creatine kinase level to more than twice the upper limit of normal value with an elevated creatine kinase-MB level. Target lesion revascularization (TLR) was defined as either PCI or CABG for restenosis of the target lesions that included the proximal and distal edge segments, as well as the ostium of the side branches associated with symptoms or objective signs of ischemia. Stroke was defined as ischemic or hemorrhagic stroke requiring hospitalization with symptoms lasting >24 hours. Stent thrombosis was assessed according to the Academic Research Consortium definition.
Continuous variables were expressed as the mean ± SD, and categorical variables as counts and/or percentage. Categorical variables were compared using the chi-square test. Multivariate analyses of independent predictors of cardiovascular mortality and TLR were performed using the Cox-proportional hazard regression model. Variables with p <0.05 on univariate analysis were selected for the multivariate analysis in consideration of potential confounding variables. Receiver-operating characteristic analysis was used to estimate the predictive performance of each score. The area under the receiver-operating characteristic curves was compared according to the method of DeLong et al. Time-to-event variables are presented as Kaplan–Meier estimates and compared using the log-rank test. A probability of p <0.05 was considered statistically significant. All statistical analyses were performed using JMP Pro, Version 12 (SAS Institute, Cary, North Carolina) and R statistical software.
Results
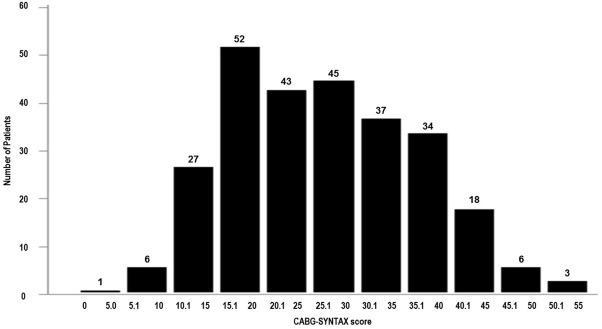
During the study period, 279 consecutive patients with previous CABG underwent PCI. Among these, 7 patients without diagnostic angiogram available or with poor imaging quality were excluded. Thus, 272 patients (217 men, mean age: 70.4 ± 9.7 years) were included for further analysis. The baseline characteristics of the study population are presented in Table 1 . The overall baseline distribution of the CABG-SYNTAX score is presented in Figure 1 . In the index procedures, PCI for the native coronary accounted for nearly all patients (88%; Table 2 ).
| Variable | All (n = 272) |
|---|---|
| Age (years) | 70.4 ± 9.7 |
| Men | 217 (80%) |
| Body mass index (kg/m 2 ) | 23.9 ± 3.3 |
| Time from CABG to percutaneous coronary intervention (years) | 7.4 ± 6.2 |
| Hypertension | 197 (72%) |
| Diabetes mellitus | 150 (55%) |
| Total cholesterol (mg/dL) | 165 ± 34 |
| Triglyceride (mg/dL) | 122 ± 65 |
| High density lipoprotein cholesterol (mg/dL) | 44 ± 13 |
| Ever smoke | 164 (60%) |
| Acute myocardial infarction | 20 (7%) |
| Previous myocardial infarction | 132 (49%) |
| Previous percutaneous coronary intervention | 132 (49%) |
| Previous stroke | 34 (13%) |
| Left ventricular ejection fraction (%) | 55 ± 15 |
| Estimated glomerular filtration rate (mL/min/1.73m 2 ) | 56 ± 25 |
| End-stage renal disease on hemodialysis | 28 (10%) |
| Peripheral artery disease | 129 (47%) |
| Previous implantable cardioverter-defibrillator | 8 (3%) |
| Medication at discharge | |
| Statins | 195 (72%) |
| Beta blockers | 108 (40%) |
| Angiotensin converting enzyme inhibitor/angiotensin receptor blocker | 164 (60%) |
| Amiodarone | 11 (4%) |
| Warfarin | 108 (40%) |
| H 2 blockers or proton pump inhibitors | 218 (80%) |
| Variable | All (n = 272) |
|---|---|
| CABG-SYNTAX score | 26.0 ± 10.2 |
| Patent internal mammary artery to the left anterior descending | 182 (67%) |
| Number of patent grafts | 1.5 ± 0.8 |
| Target coronary narrowing | |
| Left main | 83 (31%) |
| Left anterior descending | 60 (22%) |
| Left circumflex | 69 (25%) |
| Right | 101 (37%) |
| At least one graft vessel | 33 (12%) |
| Number of vessels treated per patient | 1.3 ± 0.6 |
| Target of chronic total occlusion (native coronary) | 35 (13%) |
| Rotational atherectomy | 24 (9%) |
| B2/C (American College of Cardiology/American Heart Association lesion classification) | 166 (61%) |
| Total numbers of stents per patient | 1.8 ± 1.2 |
| Mean stent diameter per patient (mm) | 3.0 ± 0.4 |
| Total stent length per patient (mm) | 36 ± 26 |
| Drug eluting stent implantation | 193 (71%) |
| Femoral approach | 146 (54%) |
| Total contrast media (mL) | 179 ± 71 |
| Angiographic success | 259 (95%) |
| Intravascular ultrasonography use | 235 (86%) |
The median duration of follow-up for the survivors was 4.1 years (interquartile range: 1.6 to 6.4 years). Complete 1-, 2-, and 4-year follow-up information was obtained for 86%, 76%, and 60% of all patients, respectively. Cardiovascular deaths occurred in 40 patients, including 15 with congestive heart failure, 13 with sudden death, one with cerebrovascular disease, one with ruptured aortic aneurysm, and 10 that were unknown. When the patients were divided into 2 groups according to the median of CABG-SYNTAX score, the frequency of all-cause death, cardiovascular death, and myocardial infarction was significantly greater in the higher CABG-SYNTAX score group than in the lower CABG-SYNTAX score group ( Table 3 ). In the multivariate analysis, age >75 years, left ventricular EF <40%, end-stage renal disease on hemodialysis, peripheral artery disease, and CABG-SYNTAX score >25 were independent predictors of cardiovascular mortality ( Table 4 ). Baseline CABG-SYNTAX score was one of the significant factors for TLR in univariate analysis.
| All Patients (n = 272) | Higher CABG-SYNTAX Score (CABG-SYNTAX score >25) (n = 134) | Lower CABG-SYNTAX Score (CABG-SYNTAX score ≤25) (n = 138) | P Value | |
|---|---|---|---|---|
| All-cause death | 51 (19%) | 32 (24%) | 19 (14%) | 0.03 |
| Cardiovascular death | 40 (15%) | 29 (22%) | 11 (8%) | 0.001 |
| Non-cardiovascular death | 11 (4%) | 3 (2%) | 8 (6%) | 0.14 |
| Myocardial infarction | 9 (3%) | 8 (6%) | 1 (1%) | 0.02 |
| Definite stent thrombosis | 2 (1%) | 1 (1%) | 1 (1%) | 0.98 |
| Stroke | 20 (7%) | 12 (9%) | 8 (6%) | 0.32 |
| Target lesion revascularization | 52 (19%) | 31 (23%) | 21 (15%) | 0.1 |
| Redo CABG | 6 (2%) | 4 (3%) | 2 (2%) | 0.38 |
| Cardiovascular Mortality | Target Lesion Revascularization | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | |||||
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age (>75 years) | 2.87 (1.53–5.46) | 0.001 | 2.82 (1.45–5.52) | 0.002 | 1.21 (0.67–2.12) | 0.52 | ||
| Men | 1.99 (0.79–6.66) | 0.19 | 0.61 (0.34–1.16) | 0.13 | ||||
| Diabetes mellitus | 1.03 (0.55–1.96) | 0.93 | 1.14 (0.66–2.01) | 0.65 | ||||
| Acute myocardial infarction | 2.55 (0.87–5.97) | 0.08 | 0.32 (0.02–1.46) | 0.17 | ||||
| Left ventricular ejection fraction <40% | 3.45 (1.68–6.67) | 0.001 | 2.99 (1.39–6.07) | 0.006 | 0.99 (0.38–2.14) | 0.98 | ||
| End-stage renal disease on hemodialysis | 4.43 (1.96–9.09) | <0.001 | 2.90 (1.15–6.75) | 0.02 | 3.70 (1.67–7.35) | 0.002 | 2.93 (1.27–6.00) | 0.01 |
| Peripheral artery disease | 2.99 (1.55–6.13) | <0.001 | 2.20 (1.10–4.64) | 0.03 | 1.75 (1.01–3.05) | 0.046 | 1.32 (0.73–2.39) | 0.36 |
| Absence of statin therapy | 2.72 (1.45–5.13) | 0.002 | 1.76 (0.88–3.48) | 0.11 | 1.65 (0.93–2.86) | 0.09 | ||
| Absence of beta blockers | 0.88 (0.47–1.73) | 0.71 | 0.83 (0.48–1.45) | 0.50 | ||||
| Absence of angiotensin converting enzyme inhibitor/angiotensin receptor blocker | 1.60 (0.86–3.00) | 0.14 | 1.03 (0.58–1.78) | 0.93 | ||||
| CABG-SNYTAX score >25 | 3.02 (1.55–6.33) | <0.001 | 2.37 (1.19–5.05) | 0.01 | 1.74 (1.01–3.07) | 0.047 | 1.20 (0.65–2.24) | 0.56 |
| PCI for left main | 1.35 (0.68–2.55) | 0.38 | 2.11 (1.20–3.64) | 0.01 | 1.81 (0.99–3.28) | 0.05 | ||
| PCI for graft vessel | 1.15 (0.39–2.69) | 0.78 | 0.99 (0.38–2.14) | 0.98 | ||||
| Rotational atherectomy | 1.14 (0.33–2.95) | 0.80 | 3.61 (1.76–6.79) | 0.001 | 2.63 (1.23–5.24) | 0.01 | ||
| Angiographic success | 0.38 (0.15–1.26) | 0.10 | 0.69 (0.25–2.84) | 0.56 | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


