Chapter 62
Iliocaval Obstruction
Endovascular Treatment
Peter Neglén, Seshadri Raju
Percutaneous endovenous stenting has emerged during the last decade as the “method of choice” for the treatment of chronic obstruction of the femoroiliocaval venous outflow. The procedure can be performed with low morbidity, no mortality, long-term high patency rate, and low rate of in-stent restenosis. It has replaced bypass surgery as the primary treatment. Open venous reconstruction for chronic femoroiliocaval obstruction should be considered only in cases of unsuccessful or failed endovenous treatment in surgically fit patients with severe symptoms.1 Stenting of the venous outflow tract specifically alleviates pain and swelling and promotes sustained ulcer healing. Most important, the quality of life of the patients is substantially improved. Availability of a relatively simple and effective endovenous treatment has also led to a reappraisal of the role of venous outflow obstruction in the pathophysiologic process of chronic venous disease. The awareness of the possible presence of iliofemoral obstruction is increasing, and consequently the venous outflow is now evaluated more carefully and stenting more frequently considered. Stenting results in marked clinical improvement whether or not an adjunct procedure to control reflux is performed.2,3 In the presence of combined iliac vein obstruction and superficial or deep reflux, therefore, the emerging course of treatment is primary correction of the obstructive component. When significant great saphenous vein reflux is present, the great saphenous vein has increasingly been obliterated by percutaneous technique at the time of the stenting.4
Clinical Findings
Symptoms of obstruction may be any of those associated with chronic venous disease, ranging from moderate swelling and pain to discoloration and stasis ulcer. Venous outflow obstruction plays an important role in the clinical expression of chronic venous disease, especially of pain.5 Remaining obstruction is the principal cause of symptoms in approximately one third of postthrombotic limbs.6,7 The iliac vein is the common outflow tract of the lower extremity, and chronic obstruction of this segment appears to result in more severe symptoms than does lower segmental blockage. The clinical expression is also influenced by any concomitant deep or superficial reflux. It is well recognized that the combination of reflux and obstruction results in the highest levels of venous hypertension and the most severe symptoms compared with either alone.8,9 Negus and colleagues suggested that limb swelling and pain are related to the obstructive component, whereas limb ulceration results from valve reflux.10 It has been shown that ulcers occur only rarely in the presence of isolated iliofemoral obstruction (4%) but more often when obstruction is associated with reflux (30%).5 A substantial number of patients with chronic venous disease complain of disabling pain and swelling of the lower limbs without skin changes. It is possible that these symptoms are mainly attributable to obstruction rather than to reflux. Five years after iliofemoral deep venous thrombosis (DVT) treated conservatively with anticoagulation, 90% of patients suffer symptoms of chronic venous disease. Debilitating “venous claudication” is found in 15% to 44% of patients, and venous ulcer has developed in 15% of limbs.11,12 Venous claudication is a dramatic condition described as an exercise-induced “bursting” pain, which requires several minutes of rest and sometimes leg elevation for relief to be achieved. Certainly patients with significant outflow obstruction may also have less distinct lower extremity pain and discomfort with decreased quality of life and moderate disability.
Patient Selection
Lack of Reliable Tests
Specific symptoms may suggest outflow obstruction, but the varying symptoms in patients with chronic venous disease and the complex underlying pathophysiologic process necessitate further investigations. The major obstacle to appropriate selection of patients for venous outflow stenting is the lack of a reliable test to measure a hemodynamically significant stenosis. Diagnosis of significant outflow obstruction, especially when it involves the common femoral vein to the inferior vena cava (IVC), will therefore be based on morphologic investigations. Physician awareness of the importance of iliofemoral venous obstruction in treating patients with chronic venous disease is essential. Although poor recanalization after acute DVT is presently thought to be the most common cause of chronic venous blockage, the existence of iliac vein compressions without thrombosis is more pathogenic than was previously thought.2,6 Thus, significant iliac venous outflow obstruction may be present without history or morphologic findings suggestive of previous DVT. In our experience in the treatment of iliofemoral obstruction in 938 limbs in 879 patients, 53% of limbs had nonthrombotic compression lesions (defined as absent history of DVT, no venographic or ultrasound findings indicating previous DVT), 40% had postthrombotic obstruction, and 7% had a combined etiology.2
After Deep Venous Thrombosis
Most symptomatic outflow obstruction occurs after DVT involving the iliac segment. It may be limited to the iliofemoral segment or contiguous from the calf to the iliac veins. Only approximately 20% of these iliac veins will completely recanalize with anticoagulation treatment; the remaining veins recanalize only partially and develop varying degrees of obstruction and collateral formation.11,13 The typical postthrombotic iliofemoral lesion often involves both common and external iliac veins with irregular stenosis or occlusions, and axial, transpelvic, and ascending lumbar collaterals are present. Infrequently, a diffusely narrowed long segment of the iliac vein with no collateral formation is found (Fig. 62-1). We have designated this entity a Rokitansky stenosis, from the 19th century pathologist who described the phenomenon.14 As the severe inflammation of the wall (phlebitis) subsides, a fibrotic cylinder is formed, which impedes any collateral development and expansion of the vein. Thus, significant outflow obstruction cannot be excluded because of lack of collaterals.
Awareness of Iliac Vein Compression
External compression of the iliac veins has been considered a common finding of little clinical importance (Fig. 62-2A and B). Previous studies have established the frequent findings of intraluminal web or band formation and varying degrees of external compression of the iliac vein in the general population (22%-33%15–17 and 66%-88%,18–20 respectively). Symptomatic nonthrombotic iliac vein obstructive lesions have previously been described as May-Thurner syndrome15 or Cockett’s or iliac vein compression syndrome.20 The prevailing concept is that iliac vein compression syndrome typically involves the left proximal common iliac vein and is clinically expressed only in the left lower extremity of predominantly young women of childbearing age. These limitations are not true because compression lesions are not uncommon in men and in elderly patients and may involve the right limb.2,10 Compression of the common iliac vein was seen in 36%, of the external iliac vein in 18%, and of both sites in 46% of limbs in symptomatic patients. The ages of the patients with nonthrombotic blockage ranged from 18 to 90 years (median, 54 years); 20% of patients were men, and 25% of the symptomatic lower limbs were on the right side.
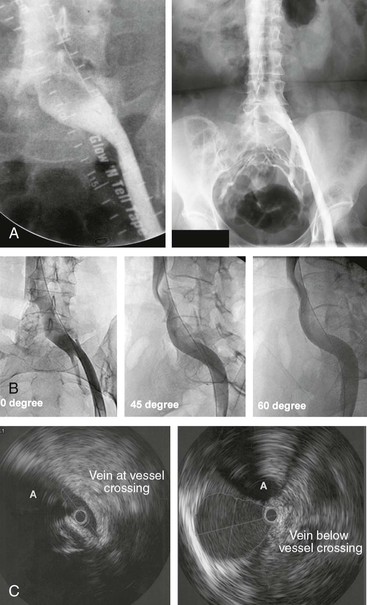
Figure 62-2 A, Single-plane transfemoral venogram showing typical findings suggestive of a left common iliac vein compression: “pancaking” and translucency of vein (left) and widening of the vein and presence of collaterals (right). B, Left transfemoral venogram with multiple projections. The oblique views (45- and 60-degree rotation) reveal stenoses, which are not visualized on the anteroposterior projection (0 degrees). C, Intravascular ultrasound (IVUS) images corresponding to the transfemoral venogram in B. The compression of the left common iliac vein is clearly shown as it is crossed by the right common iliac artery (A) (left) compared with the normal vein below the venous stenosis (right). The black circle inside the vein represents the inserted IVUS catheter.
Why a silent lesion should suddenly become significant in the pathophysiologic process is not fully understood. It has been suggested that the nonthrombotic iliac vein obstructive lesion is a so-called permissive lesion that does not become clinically significant until other components of the venous circulation of the lower limb fail. Correction of a permissive lesion alone often results in cure, which may explain the surprisingly good results of venous stenting in chronic venous disease even in the presence of untreated reflux.2
Evaluation of Venous Hemodynamics
Critical Venous Stenosis
The degree of hemodynamic venous obstruction depends on multiple factors: the number, location, degree of narrowing, and length of the lesions; the development of collaterals; and the volume flow varying at rest and during exercise. The venous circulation is a low-pressure, low-velocity, large-volume, and low-resistance converging vascular system (“sewage draining system”) compared with the high-pressure, high-velocity, small-volume, and high-resistance diverging arterial system (“water supply system”).21 The major obstacle in diagnosis of venous obstruction is that it is presently not known at what degree a venous stenosis is hemodynamically significant. Consequently, there is no accurate hemodynamic test (“gold standard”) available to properly assess venous outflow obstruction and its improvement after stenting in individual limbs.
Plethysmography
Plethysmographic outflow fraction determination and pressure tests (hand-foot pressure differential, hyperemia-induced dorsal foot venous pressure increase) are global hemodynamic tests and may suggest obstruction to the venous outflow at any anatomic site and level, but significant blockage may exist in the presence of a normal result.22–24 Positive test results may support further investigation and intervention, but a negative test result does not exclude clinically significant venous outflow obstruction.
Femoral Venous Pressure
Femoral venous pressure is a test for focal outflow obstruction. A pull-through pressure differential over a lesion or a pressure increase peripheral to the lesion with augmentation of venous inflow may be indicative of a significant stenosis.25–27 The venous pressure not only is a function of resistance to the flow but also depends to a high degree on the flow velocity and magnitude of volume flow. It is not known to what degree the resting venous flow must be increased to detect a functionally significant stenosis, nor is a method available to reproduce this flow rate consistently. Pressure gradients recorded in the venous system are much lower than in the arterial system, and only small pressure differentials may indicate significant obstruction. Studies suggest that a prestenotic pressure rise in the supine position greater than 2 to 4 mm Hg on provocation, a slow return to base level (>30s), or a gradient compared with the contralateral femoral pressure exceeding 2 to 5 mm Hg indicates a hemodynamically significant obstruction.25–27 It has been suggested that a pressure differential on exercise should be at least 5 mm Hg to warrant intervention, but none of these pressure limitations has been validated. Good clinical results have been obtained in the treatment of morphologic obstruction with normal pressure findings.28
The accuracy of these hemodynamic tests is insufficient to detect borderline obstructions. Thus, they play only a limited role in the management of obstructive disease. A positive hemodynamic test result may indicate hemodynamic significance, but a normal finding does not necessarily exclude it.
Investigations of the Venous Morphology
Venography
In lieu of an adequate hemodynamic test, morphologic tests must be used. Ascending venography after injection of contrast dye in a foot vein or antegrade transfemoral venography reveals the distribution and nature of the morphologic changes, including occlusion, stenosis, and the presence of collateral circulation, but is unable to indicate any hemodynamic impact of visualized lesions. Ascending venography usually insufficiently visualizes the iliac vein to permit assessment of any obstruction of that segment. It is mainly used today as a preoperative mapping tool to delineate the inflow to a postthrombotic iliac vein segment considered for stenting. To increase accuracy, all antegrade transfemoral venography should be performed by arterial angiographic techniques with subtraction imaging, multiple oblique projections, and pressure injectors (see Fig. 62-2B). With this technique, the quality of the images will improve and the contrast medium load will be minimal. A single-plane venogram was actually considered “normal” in at least one fourth of limbs despite the fact that intravascular ultrasound (IVUS) showed more than 50% obstruction.29 Interestingly, Cockett and colleagues made similar observations.10,19,20 Venography was diagnostic in only 65% of obstructed limbs in their experience, and collaterals were visualized in only 63%. It was noted that in 54% of symptomatic patients, findings on transfemoral venography appeared “normal” with smooth contours of contrast material in the iliac vein and without collaterals. The authors noted that absence of collateral formation should not negate consideration of the disease.10,20
Although the formation of collaterals is classically regarded as a compensatory mechanism to bypass and thus alleviate an obstruction, the precise mechanism and inducement of collateral formation are unknown. Collateral circulation shown before stenting is often not visualized after stenting of a venous stenosis (Fig. 62-3). The flow through the stent is obviously favored. Limbs with collateral formation have been shown to have a significantly tighter stenosis than limbs with no collaterals, as measured by IVUS.30 The rate of limbs with femoral pressure increase on intra-arterial injection of papaverine was three times greater in patients with collaterals. These observations support the concept of pelvic collateralization as an indicator of obstruction and that collaterals poorly compensate for the blockage in symptomatic patients.
Ultrasound Scanning
Ultrasound scanning of the iliac vein is under development but still lacks sufficient accuracy to detect partial chronic obstruction. It can be used to evaluate patency of inserted stents. Computed tomographic venography and magnetic resonance venography techniques are improving and may replace transfemoral venography for screening in the future.31–35 Like ultrasound scanning, none of these tests have been validated in chronic obstructive disease.
Intravascular Ultrasound
IVUS is superior to single-plane and multiplane venography in detection of the extent and type of morphologic lesion of the vein (Fig. 62-2C).30,36–40 It is the most accurate test in this aspect and should be used to validate findings of other morphologic imaging methods. IVUS has proved superior in showing intraluminal details (e.g., trabeculations and webs) that may be hidden in the contrast medium. Venous wall thickness, in-stent layering, and movement can be adequately assessed. An external compression with the resulting deformity of the venous lumen or postthrombotic remodeling can be directly visualized (Fig. 62-4). The degree of stenosis can be precisely calculated by measurement of the cross-cut areas and diameters of the normal and compressed or diseased veins with the software built into the IVUS apparatus. In addition to being a diagnostic tool, it is also a crucial aid to guide stent insertion.
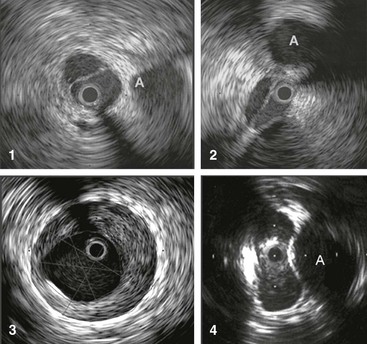
Figure 62-4 Images obtained by venous intravascular ultrasound (IVUS). 1, Intraluminal septa. 2, Trabeculation with multiple lumina. 3, In-stent restenosis precisely identifying the stent, neointimal hyperplasia, and remaining lumen. 4, Compression of the vein by the artery at the iliac vessel crossing, creating an hourglass appearance. The adjacent artery is marked with an A. The black circle inside the vein represents the inserted IVUS catheter.
Current Indications for Stenting
The major obstacle to improving the selection of patients for venous outflow stenting is the lack of a reliable test to measure a hemodynamically significant stenosis. The key for the physician is to be aware of the importance and possibility of venous blockage. Patients with previous DVT, patients with limb symptoms (especially pain out of proportion to detectable disease), patients not improving with conservative treatment, and patients with no other detectable pathologic changes to explain their symptoms are specifically targeted. More than half of patients with leg ulcers that do not improve with conservative treatment and saphenous vein ablation or phlebectomy have been found to have iliac vein outflow obstruction.41 Although a positive result of a noninvasive or invasive test may support further studies, a negative test result should not exclude it. The diagnosis and treatment must presently be based on invasive morphologic investigations of the iliac venous outflow, although hemodynamic criteria would be preferred. IVUS investigation is the ultimate test and should be generously used in symptomatic patients in whom outflow obstruction is suspected. Morphologic obstruction of more than 50% as measured by IVUS has arbitrarily been chosen for stenting.42,43 Limiting workup of patients with significant chronic venous disease to only duplex ultrasound will not suffice, especially not when it is restricted to the infrainguinal vein segments.
Technique
The technical details of percutaneous endovenous stenting of the venous outflow tract have been described in several reports.30,37,42,44 Although venous stenting may appear a simple procedure, attention to details is important to ensure an optimal outcome (Box 62-1). Venous balloon angioplasty with stenting is a different procedure from that employed in the arterial system. Experience acquired from arterial dilatation and stenting may not necessarily be extrapolated to the venous system. Balloon angioplasty alone is insufficient in the venous system. Stent insertion is mandatory. Severe recoil of the vein is observed intraoperatively in the majority of limbs, and simple balloon dilatation leads to early restenosis.45–48 The procedure may be performed under local infiltration analgesia in combination with monitored sedation or general anesthesia. Because the balloon dilatation may be painful, general anesthesia is recommended when tight stenoses or occlusions are stented. Attempts to recanalize occluded veins are also often time-consuming. The procedure should be performed in a fully equipped endovascular or angiographic suite, and availability of IVUS and external ultrasound for cannulation guidance is essential.
Access
Access to the iliac segment can be achieved retrogradely through the jugular or contralateral femoral vein, but an antegrade approach through an ultrasound-guided access distal to the obstruction in the thigh portion of the femoral vein or through the popliteal vein is preferred. Popliteal vein access is rarely used and often is not possible because of segmental occlusion of the proximal femoral vein. The midthigh access facilitates recanalization of occlusions from below, evaluation of the inflow, and precise placement of the stent in relationship to distal tributaries when necessary. Ultrasound guidance is particularly helpful in this situation to avoid inadvertent arterial puncture as the femoral vein occupies a variable posterolateral or posteromedial location in reference to the femoral artery. In contrast to arterial access at the thigh level, control of the venipuncture site by manual pressure is not a problem because of the low venous pressure. Ultrasound-assisted guidance of the cannulation is a necessity and has largely eliminated access complications.
Traversing the Lesion
Nonocclusive Obstruction
A hydrophilic guide wire (0.035 inch) is inserted and the cannula replaced by a 9F to 11F sheath, which will accommodate the appropriate balloon and stent sizes. A stiff guide wire and predilatation with serial dilators may be necessary to facilitate sheath placement in case of perivenous fibrosis of the postthrombotic femoral vein. Except in the event of occlusions, the guide wire can usually be passed through the stenosis and into the IVC with ease. An initial contrast venogram is then obtained. Multiplane venograms (anteroposterior, 45- and 60-degree oblique projections) are necessary to delineate a stenosis, which may not be revealed in the anteroposterior projection, especially if IVUS is not available (Fig. 62-5). IVUS is superior to venography in delineating any obstructive lesion and is recommended for diagnosis of the extent and degree of obstruction.
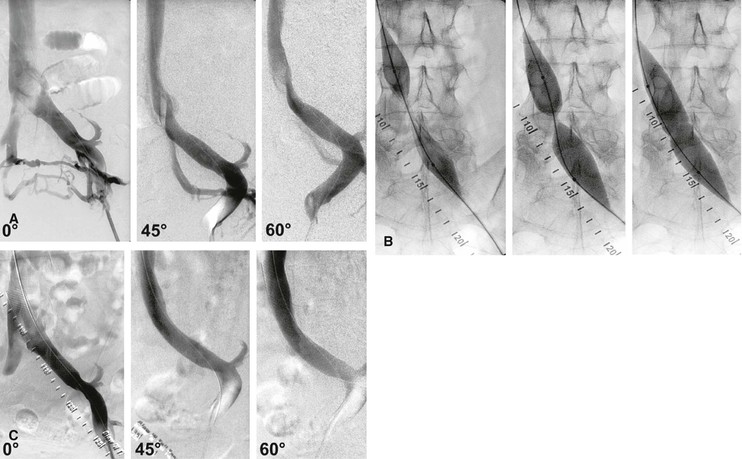
Figure 62-5 Balloon dilatation and stenting of a left common iliac vein compression (May-Thurner syndrome). A, Multiplane projections show the absence of obvious stenosis, a translucent area of the common iliac vein, and the presence of collaterals in the anteroposterior view before venous stenting. The stenosis is detected by rotation. B, Waisting of balloon during inflation by the stenosis. C, Post-stent venogram revealing no stenosis.
Occlusion
When an occlusion is present, the initial venogram may suggest the direction of manipulation of the guide wire beyond the point of occlusion. Recanalization is a challenging procedure and can be time-consuming (Fig. 62-6A to F). Success or failure in recanalization of occlusions cannot be predicted by the duration or extent of the lesion or its venographic appearance. The initial venogram may appear discouraging, but more often than not, a guide wire can be passed through the complete occlusion by sight and feel (see Fig. 62-6A). Patience is the key. In the event of initial failure, one or more additional attempts at reopening of the occlusion are warranted in all cases. Surprisingly, the guide wire tracks in the occluded lumen of the vein, which can be verified with IVUS after predilatation (see Fig. 62-6D). Multiple small-volume injections of contrast material and multiple oblique projections are performed to ensure that the guide wire stays in the vessel and progresses in the correct direction in the pelvis. Limited extravasations of contrast material can be safely ignored and the procedure continued. Larger dye extravasation calls for cessation of the procedure, which can be reattempted a few weeks later. A combination of soft and stiff guide wires with straight, angled, and J tips of different sizes (0.018 to 0.035 inch) and with supporting catheters (straight or angled) is required. Once the correct plane has been entered, rapid progress can usually be achieved without perforation by developing a loop or extended J at the end of a semistiff guide wire or catheter-supported soft wire during manipulation. Once the guide wire has traversed the occluded common iliac vein, passage through the iliocaval junction usually meets with additional resistance, again requiring extended manipulation in the area with coaxial catheter support. Specialized techniques, such as those described to cross the occluded aortoiliac junction, are usually not used.49 Successful vena cava entry is indicated by further easy passage of the guide wire into the right atrium and is confirmed by injection of contrast material through a general purpose catheter (5F) exchanged for the guide wire (see Fig. 62-6B).
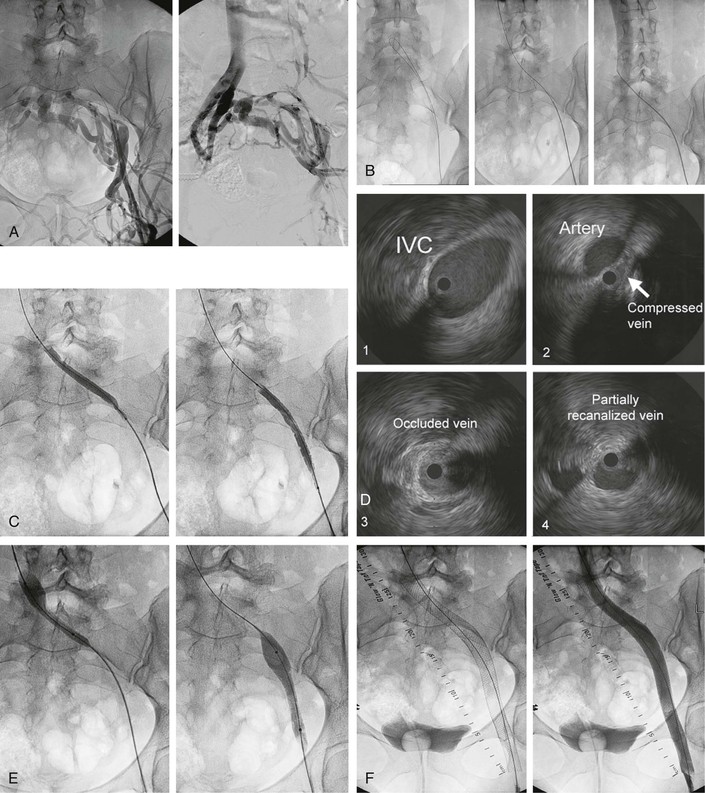
Figure 62-6 A, Transfemoral venogram performed through a sheath inserted after ultrasound-guided cannulation of the left femoral vein. A complete postthrombotic chronic occlusion of the left common iliac vein and severe stenosis of the external and common femoral veins are shown. Huge transpelvic collaterals fill a normal right iliocaval venous system. B, The obstruction has been traversed by manipulation with soft and stiff guide wires supported by guiding catheters (left). A cavogram obtained by contrast dye injection through an inserted general purpose catheter ensures that the inferior vena cava (IVC) has been penetrated. C, The occluded vessel is recanalized by a smaller balloon to allow passage of the intravascular ultrasound (IVUS) catheter for assessment of extent of lesion and subsequent insertion of larger balloons and stents. D, Images obtained by venous IVUS. 1, Normal IVC proximal to stenosis. 2, The common iliac vein severely compressed by the crossing iliac artery. 3, The completely occluded common iliac vein. Despite the chronic nature of the occlusion, the recanalizing guide wire has followed the course of the original vein and is clearly intraluminal on this image. 4, The partially recanalized external iliac vein. The black circle inside the vein represents the inserted IVUS catheter. E, Sequential ballooning of the entire iliofemoral venous segment to final diameter size (in this case, 14-mm width). F, Left, Image showing the entire stent system comprising three stents, proximally placed well into the IVC and then telescoped over each other to cover the entire iliofemoral vein, with the distal end placed at the inflow of the profunda vein. Right, Final transfemoral venogram, which shows uninterrupted venous outflow and no visualization of any collaterals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




