One of the most commonly used conduits in the setting of endovascular aortic repair is the surgically created conduit approached through a retroperitoneal exposure to the common iliac artery or distal aorta. Preoperative imaging helps to determine which side is chosen, taking into account the vessel’s size and calcification. A standard incision is made in an oblique, slightly curvilinear fashion two fingerbreadths from the anterior superior iliac spine, starting at or slightly above the level of the umbilicus. The external oblique, internal oblique, and transversalis muscles are divided with electrocautery, exposing the peritoneum. The retroperitoneal space is exposed by gently mobilizing the peritoneum with a sponge stick. The ureter is identified, and if the left side is chosen, care is taken to avoid manipulating the nerve plexus draped over the common iliac artery. A self-retaining retractor is useful to maintain exposure while the conduit is created.
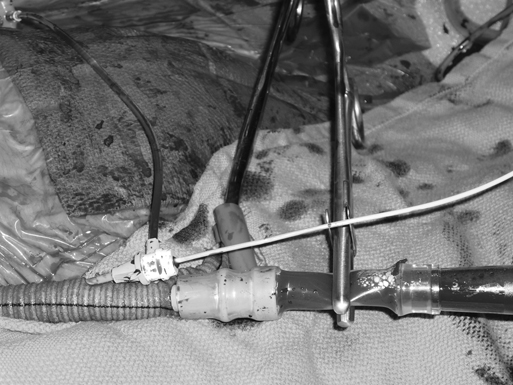
After systemic anticoagulation, depending on the patient’s anatomy, two vascular clamps or a side-biting clamp is placed on the iliac artery, and a 10-mm polyester graft is sewn in an end-to-side fashion to the vessel using a running monofilament suture (Figure 1). A graft of this size will accommodate both the delivery sheath and a 5-Fr sheath used for passage of a diagnostic angiogram catheter (Figure 2). This allows single-sided access in the setting of TEVAR. The anastomosis can be reinforced with a felt cuff in patients with friable vessels, and it can be marked with a radiopaque clip so that the level of the anastomosis can be visualized fluoroscopically during later sheath passage. In obese patients or in deep wounds, the graft is often tunneled out the abdominal wall through a separate stab incision in the skin to keep the sheath from entering into the native vessel at a steep angle.
The open end of the graft is clamped, the side of the conduit is punctured with an entry needle, and the sheaths are inserted through the side of the graft to avoid unnecessary blood loss if sheath exchanges are required. The tip of the delivery sheath should be advanced through the anastomosis so that the anastomosis is not disrupted with multiple device exchanges. Manual stabilization of the anastomosis as the delivery sheath passes through the anastomosis can also aid in preventing disruption.
After the endovascular portion of the procedure is completed, the sheaths are removed from the conduit, the graft is transected, and the remaining small cuff is oversewn or transected and closed with a vascular stapler. Presence of this cuff should be noted because it can lead to some confusion on postoperative imaging. Alternatively, in the setting of symptomatic iliac occlusive disease, the graft can be tunneled under the inguinal ligament and can be used as an iliofemoral bypass. In either case, the patient has a prosthetic graft that is susceptible to infection.
Another option for endovascular access is direct aortic or iliac access. This can be performed through the retroperitoneal approach described earlier or through a transperitoneal approach if the patient is undergoing simultaneous exploratory laparotomy (e.g., trauma patients). This option avoids leaving behind prosthetic material prone to infection, or if too large a cuff is left behind, it may be a source of distal embolization. Some describe puncturing the artery in the middle of a purse-string suture placed in the common iliac artery or distal aorta and cinching down the adventitial suture after removing the sheath. Although this technique and the standard iliac conduit technique overcome iliac artery limitations, both require retroperitoneal dissection, which can add to the morbidity of endovascular aortic procedures.
The retroperitoneal approach, in comparison to the femoral approach used during endovascular aortic procedures, has been shown to lead to a 2.6-fold greater blood loss, 1.5-day longer hospital stay, 82% longer procedure time, and a 21% incidence of retroperitoneal hematoma. Nevertheless, surgical conduits or direct arterial access through a retroperitoneal exposure are excellent options for overcoming iliac artery size and tortuosity limitations. These options require involvement of physicians with surgical expertise and stringent adherence to sterile techniques as can be found in the operation room setting.