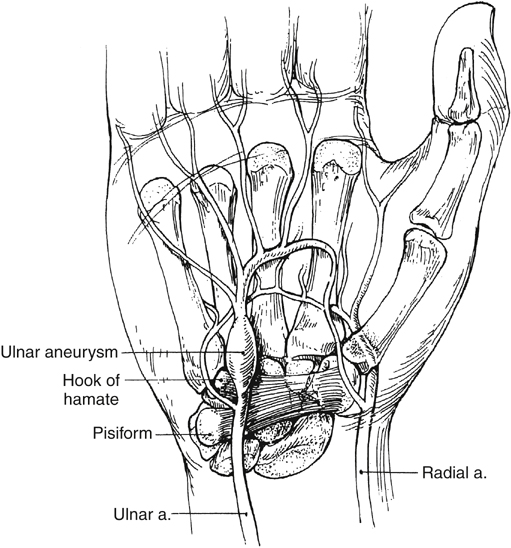
The ulnar artery is the larger medial branch of the brachial artery at the antecubital fossa, and in the majority of people it is the dominant artery that supplies the hand. At the wrist level, the ulnar artery, along with the ulnar nerve, superficializes over the flexor retinaculum before it enters the hand (Figure 1). At this juncture the ulnar artery gives rise to the deep palmar branch, which enters the hand medial to the pisiform and lateral to the hook of the hamate carpal bone. The remainder of the ulnar artery enters the hand by passing over the hamate and the hypothenar muscle, to enter through Guyon’s canal and give rise to the superficial palmar branch. This 2- to 3-cm segment of the ulnar artery is fixed, palpable, superficial, and only protected by skin, subcutaneous tissue, a portion of the palmaris brevis muscle, and the superficial palmar aponeurosis. The relative paucity of overlying tissue makes the superficial portion of the ulnar artery susceptible to blunt forces, which are accentuated by its contiguous bony process (hook of the hamate), which functions very much like an anvil (see Figure 1).
The superficial palmar arch is the dominant vascular supply of the hand, and in 37% of people it is entirely supplied by the superficial palmar branch of the ulnar artery. Extending underneath the palmar aponeurosis, the superficial palmar arch gives rise to three common palmar digital arteries that extend adjacent to the lumbrical muscles, and each divide into the proper palmar digital arteries that supply their respective digits. Notably, only 10% of people have a classic superficial palmar arch that joins the superficial palmar branch of the ulnar artery and to branches of the radial artery. Cadaveric studies demonstrate that 78% of people have a complete superficial arch that supplies all fingers including the ulnar side of the thumb. The remaining individuals with incomplete arches are found to have diverse anatomic branching patterns, and they might have a more dominant deep palmar arch. A complete deep palmar arch occurs in 76% to 96% of the population and describes an arch that migrates from the radial artery, across the metacarpals, to join the deep palmar branch of the ulnar artery.
The presence of collaterals, completeness of the palmar arches, and degree of dominance of the ulnar arterial supply can significantly influence the severity of symptoms in patients with HHS. With a classically dominant superficial palmar arch, disruption of the ulnar artery is more likely to result in more profound symptoms. However, in patients with an incomplete or nondominant superficial palmar arch, symptoms may be less severe, or they can even be masked by the presence of sufficient arterial flow by collaterals.
It is presumed that acute forceful trauma to the ulnar artery induces microtears in the intima and causes denudation of the endothelium. Ordinarily the intima recovers from such insults, but with repetitive trauma, subendothelial matrix proteins are exposed that promote the adhesion of macrophages and platelets to the site of injury. Recruited cells release inflammatory mediators that by way of paracrine mechanisms can induce hyperplasia, fibrosis, and thrombosis. Indeed, pathologic examination of resected ulnar artery segments from patients with HHS demonstrate a high incidence of intimal hyperplasia as evidence of the chronic inflammatory changes the ulnar artery endures in HHS.
Repetitive blunt trauma can also damage the arterial media and disrupt its matrix of elastin and collagen fibers. Histologic studies reveal fragmentation of the internal elastic lamina, hemorrhage into the media, and fibrosis of the vessel wall. Over time these disruptions can lead to gradual arterial wall aneurysmal dilatation, adventitial fibrosis, and periarterial sympathetic fiber disruption. As in other low-resistance vascular arterial beds, aneurysmal dilation of the distal ulnar artery can lead to thrombus accumulation and subsequent microembolization to the terminal arterioles in the digits.
In one study, histologic evaluation of arterial specimens from patients affected by HHS suggested pathologic characteristics of fibromuscular dysplasia. The authors concluded that perhaps certain persons have intrinsically abnormal arteries that predispose them to develop HHS following repetitive trauma to the ulnar artery. However, this argument did not explain why the majority of persons affected are male, whereas fibromuscular dysplasia is more commonly diagnosed in female patients. Moreover, there are no reports of HHS patients who also have evidence of disease in other arterial beds that are typically affected by fibromuscular dysplasia, such as the renal, iliac, or carotid arteries.