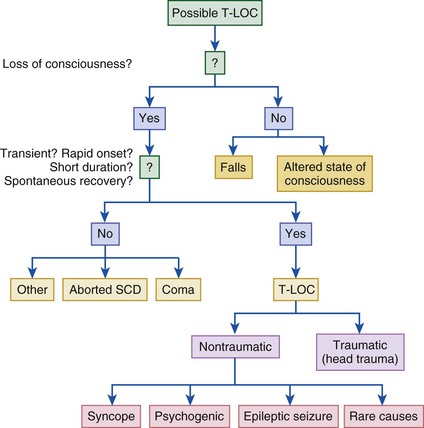
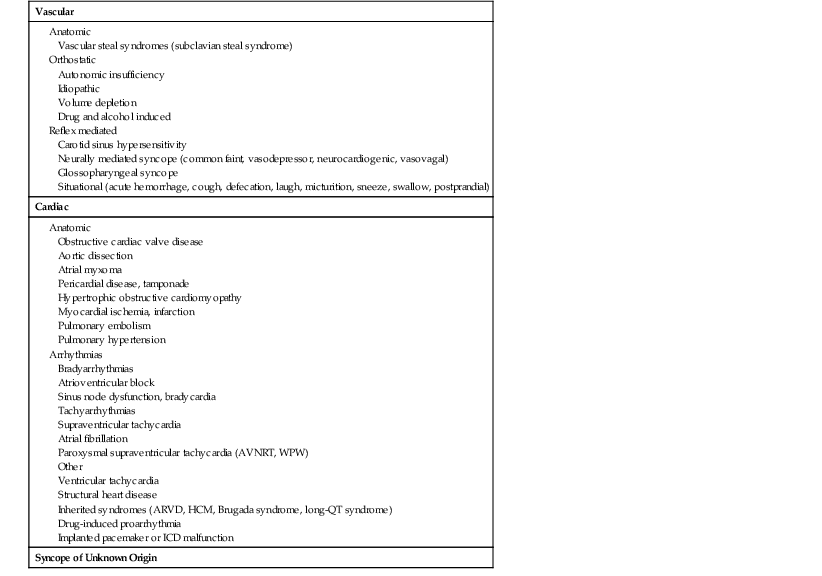
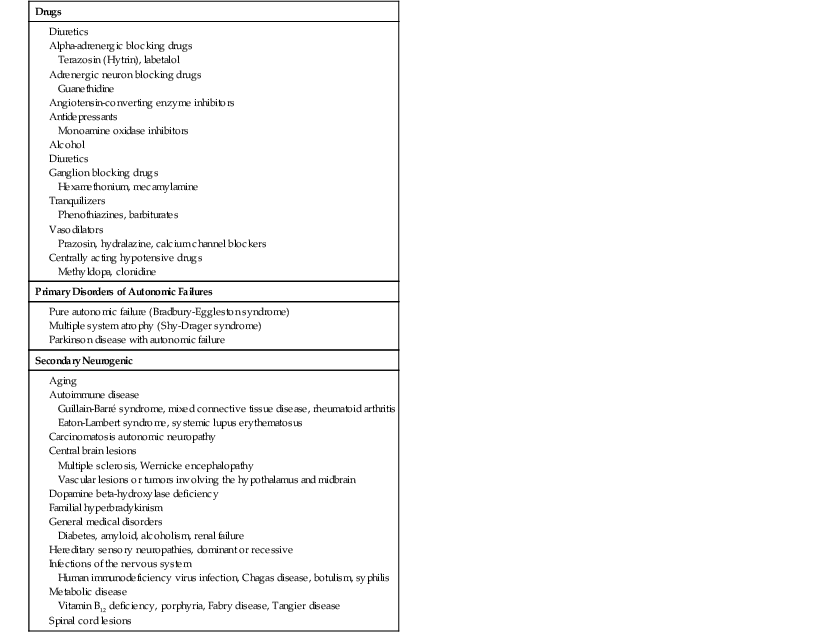
Hugh G. Calkins, Douglas P. Zipes Syncope, or transient loss of consciousness (LOC) caused by transient global cerebral hypoperfusion, is characterized by rapid onset, short duration, and spontaneous recovery.1 LOC results from a reduction in blood flow to the reticular activating system located in the brainstem and does not require electrical or chemical therapy for reversal. The metabolism of the brain, in contrast to that of many other organs, is exquisitely dependent on perfusion. Consequently, cessation of cerebral blood flow leads to LOC within approximately 10 seconds. Restoration of appropriate behavior and orientation after a syncopal episode is usually immediate. Retrograde amnesia, though uncommon, can be present in older adults. It is important to recognize that syncope, as defined above, represents a subset of a much wider spectrum of conditions that can result in transient LOC, including conditions such as stroke and epileptic seizures. Nonsyncopal causes of transient LOC differ in their mechanism and duration.1 Syncope is an important clinical problem because it is common, costly, and often disabling; can cause injury; and can be the only warning sign before sudden cardiac death1–3 (see Chapter 39). Patients with syncope account for 1% of hospital admissions and 3% of emergency department visits. Surveys of young adults have revealed that up to 50% report a previous episode of LOC. Most of these episodes are isolated events that never come to medical attention. The prevalence of a first episode of syncope is particularly high between the ages of 10 and 20 years.4 Additional peaks in the prevalence of first syncopal episodes occur at approximately 60 and 80 years of age.4 Patients who experience syncope also report markedly reduced quality of life. Furthermore, syncope can result in traumatic injury.5 The prognosis of patients with syncope varies greatly with the diagnosis. Patients with syncope in the setting of structural heart disease or primary electrical disease have an increased incidence of sudden death and overall mortality. Syncope caused by orthostatic hypotension is associated with a twofold increase in mortality, which reflects the presence of multiple comorbid conditions in this patient group. In contrast, young patients with neurally mediated syncope have an excellent prognosis. Shown in Tables 40-1 and 40-2 are the diagnostic considerations in patients with real or apparent transient LOC (Table 40-1) and also in those with syncope (Table 40-2). An approach to the differential diagnosis of transient LOC is outlined in Figure 40-1.1 Syncope can be distinguished from most other causes of transient LOC by asking whether the LOC was transient, of rapid onset, of short duration, and followed by spontaneous recovery. If the answer to each of these questions is yes and the transient LOC did not result from head trauma, the diagnostic considerations include true syncope in which the mechanism of transient LOC is global cerebral hypoperfusion, epileptic seizures, psychogenic syncope, and other rare causes. It is important to consider nonsyncopal conditions when evaluating a patient with transient LOC, such as metabolic disorders, epilepsy, or alcohol, as well as conditions in which consciousness is only apparently lost (i.e., conversion reaction). These psychogenic causes of syncope, being recognized with increased frequency, are typically diagnosed in patients 40 years or younger and especially in those with a history of psychiatric disease. TABLE 40-1 Causes of Real or Apparent Transient Loss of Consciousness TABLE 40-2 Causes of Syncope AVNRT = AV nodal reentrant tachycardia; ARVD = arrhythmogenic right ventricular dysplasia; HCM = hypertrophic cardiomyopathy; WPW = Wolff-Parkinson-White syndrome. The differential diagnosis of syncope (see Table 40-2) includes vascular causes as most common, followed by cardiac causes, with arrhythmias being most frequent (see Chapter 37). Although knowledge of the common conditions that can cause syncope is essential and allows the clinician to arrive at a probable cause of the syncope in most patients, it is equally important to be aware of several less common but potentially lethal causes of syncope, such as long-QT syndrome, arrhythmogenic right ventricular dysplasia, Brugada syndrome, hypertrophic cardiomyopathy, idiopathic ventricular fibrillation (VF), catecholaminergic polymorphic ventricular tachycardia, short-QT syndrome, and pulmonary emboli6–11 (see Chapter 32). It is important to recognize that the distribution of causes of syncope varies both with patient age and with the clinical setting in which the patient is evaluated. Neurally mediated syncope and other causes of reflex-mediated syncope are the most frequent causes of syncope at any age and in any setting. Cardiac causes of syncope, especially cardiac tachyarrhythmias and bradyarrhythmias, are the second most common causes of syncope. The incidence of cardiac causes of syncope is higher in older adults and in patients evaluated in emergency departments. Orthostatic hypotension is extremely uncommon in patients younger than 40 years but is common in very elderly adults (see Chapter 76). Vascular causes of syncope, particularly reflex-mediated syncope and orthostatic hypotension, are by far the most common causes and account for at least a third of all syncopal episodes.1,2,12–21 In contrast, vascular steal syndromes are exceedingly uncommon causes of syncope. Standing displaces 500 to 800 mL of blood to the abdomen and lower extremities, thereby resulting in an abrupt drop in venous return to the heart. This drop leads to a decrease in cardiac output and stimulation of aortic, carotid, and cardiopulmonary baroreceptors, which triggers a reflex increase in sympathetic outflow. As a result, heart rate, cardiac contractility, and vascular resistance increase to maintain stable systemic blood pressure (BP) on standing. Orthostatic intolerance is a term used to refer to the signs and symptoms of an abnormality in any portion of this BP control system. Symptoms of orthostatic intolerance include syncope, lightheadedness/presyncope, tremulousness, weakness, fatigue, palpitations, diaphoresis, and blurred or tunnel vision. Orthostatic hypotension is defined as a 20–mm Hg drop in systolic BP or a 10–mm Hg drop in diastolic BP within 3 minutes of standing. Orthostatic hypotension can be asymptomatic or associated with the symptoms of orthostatic intolerance just listed. These symptoms are often worse immediately on arising in the morning or after meals or exercise. Initial orthostatic hypotension is defined as less than a 40–mm Hg decrease in BP immediately on standing with rapid return to normal (<30 seconds).17 In contrast, delayed progressive orthostatic hypotension is characterized by a slow progressive decrease in systolic BP on standing.18 Syncope that occurs after meals, particularly in elderly people, can result from a redistribution of blood to the gut. A decline in systolic BP of approximately 20 mm Hg approximately 1 hour after eating has been reported in up to a third of elderly nursing home residents. Though usually asymptomatic, it can result in lightheadedness or syncope. Drugs that either cause volume depletion or result in vasodilation are the most common causes of orthostatic hypotension (Table 40-3). Elderly patients are particularly susceptible to the hypotensive effects of drugs because of reduced baroreceptor sensitivity, decreased cerebral blood flow, renal sodium wasting, and an impaired thirst mechanism that develops with aging. Orthostatic hypotension can also result from neurogenic causes, which can be subclassified into primary and secondary autonomic failure (see Chapter 89). Primary causes are generally idiopathic, whereas secondary causes are associated with a known biochemical or structural anomaly or are seen as part of a particular disease or syndrome. TABLE 40-3 Causes of Orthostatic Hypotension Modified from Bannister SR (ed): Autonomic Failure. 2nd ed. Oxford, Oxford University Press, 1988, p 8. Postural orthostatic tachycardia syndrome (POTS) is a milder form of chronic autonomic failure and orthostatic intolerance characterized by the presence of symptoms of orthostatic intolerance, an increase of 28 beats/min or more in heart rate, and absence of a significant change in BP within 5 minutes of standing or upright tilt.1,2,14 The precise pathophysiologic basis for POTS has not been well defined. Some patients have both POTS and neurally mediated syncope.15 Reflex-mediated causes of syncope are listed in Table 40-2. In this group of conditions the cardiovascular reflexes that control the circulation become inappropriate in response to a trigger, which results in vasodilation with or without bradycardia and a drop in BP and global cerebral hypoperfusion. In each case the reflex is composed of a trigger (the afferent limb) and a response (the efferent limb). This group of reflex-mediated syncopal syndromes has in common the response limb of the reflex, which consists of increased vagal tone and withdrawal of peripheral sympathetic tone and leads to bradycardia, vasodilation, and ultimately, hypotension, presyncope, or syncope. If hypotension secondary to peripheral vasodilation predominates, it is classified as a vasodepressor-type reflex response; if bradycardia and/or asystole predominates, it is classified as a cardioinhibitory response; and when both vasodilation and bradycardia play a role, it is classified as a mixed response. What distinguish these causes of syncope are the specific triggers. For example, micturition-induced syncope results from activation of mechanoreceptors in the bladder, defecation-induced syncope results from neural input from gut wall tension receptors, and swallowing-induced syncope results from afferent neural impulses arising from the upper gastrointestinal tract. The two most common types of reflex-mediated syncope, carotid sinus hypersensitivity and neurally mediated hypotension, are discussed later. Identification of the trigger is of importance because of its therapeutic implications, with avoidance of the trigger possibly preventing further syncopal episodes. The term neurally mediated hypotension or syncope (also known as neurocardiogenic, vasodepressor, and vasovagal syncope and “fainting”) has been used to describe a common abnormality in regulation of BP characterized by an abrupt onset of hypotension with or without bradycardia. Triggers associated with the development of neurally mediated syncope include orthostatic stress, such as can occur with prolonged standing or a hot shower, and emotional stress, such as can result from the sight of blood.1,2,13,16 A large proportion of patients with neurally mediated syncope may have minor psychiatric disorders.19 It has been proposed that neurally mediated syncope results from a paradoxical reflex that is initiated when ventricular preload is reduced by venous pooling. This reduction leads to a decrease in cardiac output and BP, which is sensed by arterial baroreceptors. The resultant increased catecholamine levels, combined with reduced venous filling, leads to a vigorously contracting, volume-depleted ventricle. The heart itself is involved in this reflex by virtue of the presence of mechanoreceptors, or C fibers, consisting of nonmyelinated fibers found in the atria, ventricles, and pulmonary artery. It has been proposed that vigorous contraction of a volume-depleted ventricle leads to activation of these receptors in susceptible individuals. These afferent C fibers project centrally to the dorsal vagal nucleus of the medulla and can result in “paradoxical” withdrawal of peripheral sympathetic tone and an increase in vagal tone, which in turn causes vasodilation and bradycardia. The ultimate clinical consequence is syncope or presyncope. Not all neurally mediated syncope results from activation of mechanoreceptors, however. In humans, the sight of blood or extreme emotion can trigger syncope, thus suggesting that higher neural centers can also participate in the pathophysiology of vasovagal syncope. In addition, central mechanisms can contribute to the production of neurally mediated syncope. Syncope caused by carotid sinus hypersensitivity results from stimulation of carotid sinus baroreceptors located in the internal carotid artery above the bifurcation of the common carotid artery. Carotid sinus hypersensitivity is detected in approximately a third of elderly patients evaluated for syncope or falls.1,2,20 It is important, however, to recognize that carotid sinus hypersensitivity is also commonly observed in asymptomatic elderly patients. Thus, the diagnosis of carotid sinus hypersensitivity should be approached cautiously after excluding alternative causes of the syncope. Once diagnosed, dual-chamber pacemaker implantation is recommended for patients with recurrent syncope or falls resulting from carotid sinus hypersensitivity.22 The American Heart Association/American College of Cardiology/Heart Rhythm Society guidelines for device implantation have given this a class I indication for pacemaker implantation.22 If the diagnosis of carotid sinus hypersensitivity is based on longer than a 3-second pause with carotid sinus massage without clear, provocative events, pacemaker implantation is less strongly recommended (class IIA). Cardiac causes of syncope, particularly tachyarrhythmias and bradyarrhythmias, are the second most common cause of syncope and account for 10% to 20% of syncopal episodes (see Table 40-2 and Chapter 39). Ventricular tachycardia (VT) is the most common tachyarrhythmia that can cause syncope. Supraventricular tachycardia (SVT) can also cause syncope, although the great majority of patients with supraventricular arrhythmias have less severe symptoms such as palpitations, dyspnea, and lightheadedness. Bradyarrhythmias that can result in syncope include sick sinus syndrome and atrioventricular (AV) block. Anatomic causes of syncope include obstruction to blood flow, such as massive pulmonary embolism (see Chapter 73), atrial myxoma (see Chapter 69), or aortic stenosis (see Chapter 63). Neurologic causes of transient LOC, including migraines, seizures, Arnold-Chiari malformations, and transient ischemic attacks, are surprisingly uncommon and account for less than 10% of all cases of syncope (see Chapters 59 and 87). Most patients in whom a “neurologic” cause of transient LOC is established are in fact found to have had a seizure rather than true syncope. Identification of the precise cause of the syncope is often challenging. Because syncope usually occurs sporadically and infrequently, it is extremely difficult to either examine a patient or obtain an electrocardiogram (ECG) during an episode of syncope. For this reason, the primary goal in the evaluation of a patient with syncope is to arrive at a presumptive determination of the cause of the syncope. The history and physical examination are by far the most important components of the evaluation of a patient with transient LOC and syncope and can be used to identify the cause in more than 25% of patients.1,2,12,23 Maximal information can be obtained from the clinical history when it is approached in a systematic and detailed fashion. Initial evaluation should begin by determining whether the patient did in fact experience a syncopal episode by asking the following: (1) Did the patient experience complete LOC? (2) Was the LOC transient with a rapid onset and short duration? (3) Did the patient recover spontaneously, completely, and without sequelae? and (4) Did the patient lose postural tone? If the answer to one or more of these questions is negative, other nonsyncopal causes of transient LOC should be suspected. Although falls can be differentiated from syncope by the absence of LOC, an overlap between symptoms of falls and syncope has been reported1,2
Hypotension and Syncope
Definition
Classification

Vascular
Cardiac
Syncope of Unknown Origin
Vascular Causes of Syncope
Orthostatic Hypotension
Reflex-Mediated Syncope
Neurally Mediated Hypotension or Syncope (Vasovagal Syncope)
Carotid Sinus Hypersensitivity
Cardiac Causes of Syncope
Neurologic Causes of Transient Loss of Consciousness
Diagnostic Tests
History, Physical Examination, and Carotid Sinus Massage
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hypotension and Syncope
40