19 Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is the accepted term for a form of unexplained left ventricular (LV) hypertrophy that is attributable to mutations in genes encoding cardiac sarcomere proteins. Although the presentation of HCM within families varies in part because of the presence of known triggers such as hypertension, HCM is distinct from myocardial hypertrophy that develops solely in response to this sort of stimulus (Fig. 19-1). The cardinal histologic feature of HCM is myofibrillar disarray occupying 20% or more of at least one pathologic tissue block.
Etiology and Pathogenesis
Various terms have been used to describe the phenotype of HCM. These include hypertrophic obstructive cardiomyopathy, idiopathic hypertrophic subaortic stenosis, asymmetric septal hypertrophy, and muscular subaortic stenosis—all based on the misconception that dynamic outflow tract obstruction was the key pathologic determinant of the hypertrophy (Fig. 19-2).
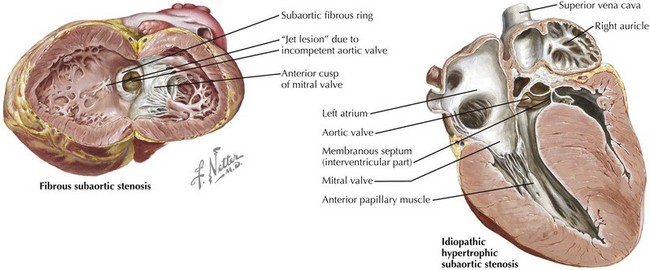
Figure 19-2 Anomalies of the left ventricular outflow tract that can mimic valvular aortic stenosis.
Epidemiology
HCM is inherited in an autosomal-dominant pattern in 50% to 75% of cases. Its prevalence is thought to be 1 per 500 in the general U.S. population and higher in African American individuals. Three age peaks of presentation have been proposed: adolescence, the early 40s, and the early 60s. The clinical presentation of HCM (syncope, sudden cardiac death, severe effort-related chest discomfort, or dyspnea) tends to be most dramatic when HCM presents in adolescence, and more dramatic when the presentation is in the 40s than in the 60s. There is a male predominance in younger patients, whereas there may be an equal or higher prevalence in females in the older population. Clinical presentation with dyspnea, atrial fibrillation, and hypertension is more common in elderly individuals. Echocardiographic differences in two series highlight ovoid LV shape in elderly persons as opposed to reversed septal curvature with a crescent-shaped cavity in persons 40 years or younger. Posterior septal movement, as opposed to systolic anterior motion of the mitral valve, may contribute to higher outflow velocities in elderly individuals. ECG findings of Q waves in the anterior and lateral leads are often seen in the younger group. The genetic basis for HCM is addressed in Chapter 72, Genetics in Cardiovascular Disease.
Differential Diagnosis
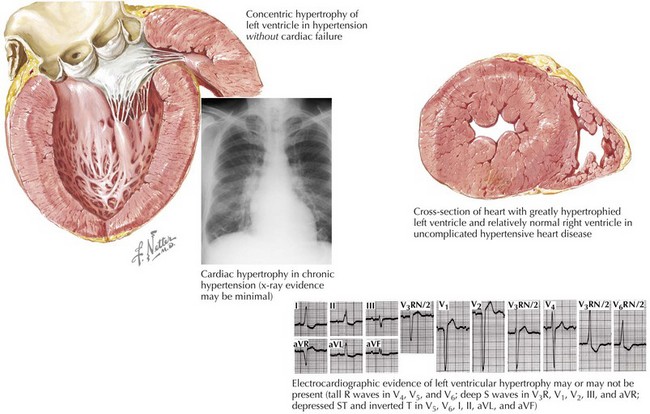
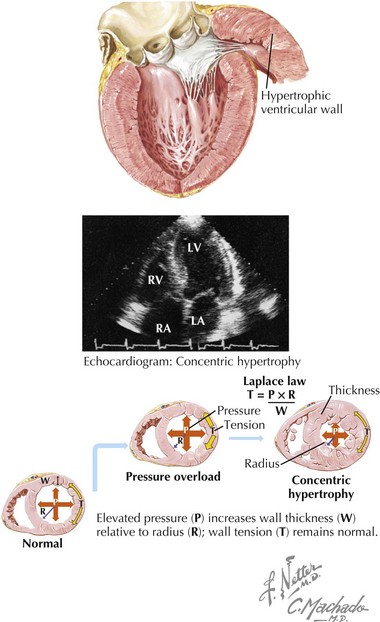
LV hypertrophy (mimicking HCM) may also be present in patients with long-standing systemic hypertension (Fig. 19-3), outflow obstruction secondary to valvular heart disease (e.g., aortic stenosis or coarctation of the aorta), and infiltrative disorders of the myocardium. At times, distinguishing these conditions from HCM clinically, or even by echocardiography, can be very difficult. Tips for making this diagnostic distinction include the following: (1) in patients with aortic stenosis the gradient is fixed, unlike in patients with HCM in whom the gradient is dynamic and may fluctuate with each heartbeat; and (2) the pattern of hypertrophy seen in patients with hypertension is concentric as opposed to the pattern seen in patients with HCM, which is often distinctive, as described later in this chapter.
Diagnostic Approach
Physical Examination
The carotid impulse of the patient with the obstructive form of HCM is rapid in upstroke, bifid, and followed by a prominent dicrotic notch. This “spike-and-dome” pulse pattern is caused by rapid ventricular emptying secondary to increased LV contractility, followed by abrupt flow reduction secondary to systolic anterior motion of the mitral valve, causing partial occlusion of the outflow tract. The jugular venous pulse in sinus rhythm is characterized by prominent a waves. The outflow murmur characteristically is systolic and heard best along the left sternal border without radiation to the carotid arteries. Because the outflow tract gradient is dynamic, the murmur can be altered by various physical and pharmacologic maneuvers (see Chapter 1). It increases with amyl nitrate, Valsalva maneuvers, and upright posture, and decreases with administration of phenylephrine, squatting, and isometric handgrip.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree