, Randall M. Zusman2 and Randall M. Zusman3
(1)
Harvard Medical School Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2)
Harvard Medical School, Boston, USA
(3)
Hypertension, Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
Abstract
Hypertension is one of the most common pathologic entities in the world and is associated with the development and exacerbation of a variety of cardiovascular disease, as well as morbid and mortal outcomes. In this chapter, we review the pathophysiology, diagnosis, treatment, and outcomes related to hypertension.
Abbreviations
ACEI
Angiotensin Converting Enzyme inhibitors
ARA
Aldosterone receptor antagonists
ARB
Angiotensin receptor blockers
BB
Beta blockers
BP
Blood pressure
CCB
Calcium channel blockers
CHD
Coronary heart disease
CKD
Chronic kidney disease
CV
Cardiovascular
DBP
Diastolic blood pressure
DM
Diabetes mellitus
HF
Heart failure
ISH
Isolated systolic hypertension
LVH
Left ventricular hypertrophy
LVSD
Left ventricular systolic dysfunction
MI
Myocardial infarction
PA
Primary aldosteronism
PAC
Plasma aldosterone concentration
PAD
Peripheral arterial disease
PRA
Plasma renin activity
PRC
Plasma renin concentration
RAAS
Renin angiotensin aldosterone system
SBP
Systolic blood pressure
WHO
World Health Organization
Introduction
Hypertension is one of the most common pathologic entities in the world and is associated with the development and exacerbation of a variety of cardiovascular disease, as well as morbid and mortal outcomes. In this chapter, we review the pathophysiology, diagnosis, treatment, and outcomes related to hypertension.
Pathophysiology and Epidemiology of Hypertension
Essential Hypertension
The great majority (90–95 %) of hypertension is essential hypertension (otherwise known as primary hypertension)
The pathophysiology of essential hypertension is incompletely understood, but is thought to related to one or more of the following
Changes in the sympathetic nervous system and renin angiotensin aldosterone system (RAAS)
Renal dysfunction
Genetic and environmental factors
With the decreasing price of genomic studies, the pathophysiologic mechanisms are being elucidated
Hypertension and Aging
Clinical and Epidemiological Importance
The probability of having hypertension increases with age
At age ≥ 70, approximately 70 % of men and women have hypertension, compared with less than 20 % among those aged ≤ 44 [1]
The residual lifetime risk of hypertension among persons ≥60 years who had not developed hypertension is approximately 90 % [2]
In the 2007–2008 NHANES data, only 50 % of all patients with hypertension were controlled to <140/90 mmHg
The proportion of patients with controlled hypertension was lower among those ≥60 years than in younger (<40) individuals [3]
There is a wealth of evidence that antihypertensive pharmacologic therapy decreases mortal and morbid clinical events
Even in the very old, antihypertensive therapy decreases mortality
In the HYVET clinical trial of patients with hypertension (mean age 83.6 years), indapamide/perindopril therapy resulted in decreased mortality and was well tolerated [4]
Differences in Systolic and Diastolic Blood Pressure
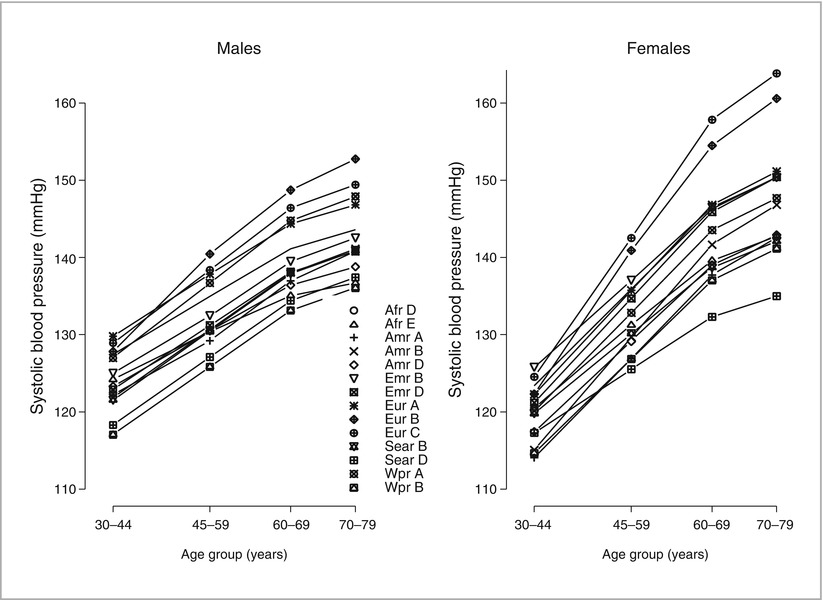
With increasing age, systolic blood pressure (SBP) increases in all populations studied
Diastolic blood pressure (DBP) increases until approximately the fifth or sixth decade and declines thereafter ([5], Fig. 5-1)
Figure 5-1
Changes in systolic and diastolic blood pressure with age (Used with permission from Burt et al. [5])
Isolated Systolic Hypertension (ISH)
The great majority of older patients with hypertension have ISH, with diastolic hypertension occurring in a minority (10 % among those aged 70)
ISH is primarily due to decreased compliance of the large arteries and increased pulse wave velocity
Age-related changes in the histology of the large vessels (especially the aorta) with a decrease in elastic fibers and replacement with collagen result in increased aortic wall stiffness and decreased compliance [5]
ISH is a result of the following phenomena ([7], Fig. 5-3):
Figure 5-3
Effect of arterial stiffening on pulse wave velocity, reflected pressure waves and central arterial pressure in younger and older persons. PWV pulse wave velocity (Modified from Asmar [7])
Increased pulse pressure (due to central arterial stiffness) for a given stroke volume, with higher SBP and lower DBP
High pulse wave velocity, which results in the reflected pulse waves arriving at the central aorta during systole rather than after the dicrotic notch (as occurs in younger individuals)
Endothelial dysfunction, which results in impaired flow-mediated arterial dilation
Additional Differences with Aging
The autonomic nervous system undergoes significant changes with aging
Downregulation and decreased responsiveness of beta-receptors and increased ambient catecholamine concentrations
The increased norepinephrine concentrations common in older individuals may be due to homeostatic mechanisms counterbalancing decreased responsiveness of the adrenergic receptors [10]
Elderly hypertensives usually have low renin, low aldosterone, salt-sensitive hypertension because of decreased natriuretic activity of the nephrosclerotic kidney and increased sodium reabsorption [11]
Renal function declines with age
Between the ages of 30 and 85, approximately one quarter of the cortex is lost due to glomerulosclerosis and interstitial fibrosis with impairment of renal hemodynamics [12]
Renal changes from nephrosclerosis and changes of the juxtaglomerular apparatus result in low renin and aldosterone levels. This may be related to expansion of total body water and suppression of renin activity [13]
The decreased renal function in hypertension may impair excretion of medications or their metabolites, especially in the elderly with polypharmacy and associated comorbidities (e.g. coronary heart disease (CHD), diabetes, dyslipidemia, and osteoarthritis)
Renal dysfunction predicts cardiovascular (CV) outcomes and mortality in older hypertensives [14]
Polypharmacy
Polypharmacy and cost result in decreased adherence to therapy
Polypharmacy in combination with decreased renal function increases the probability of drug interactions and adverse events
Non-steroidal anti-inflammatory agents (NSAIDs)
There is increased use of NSAIDs among older patients (see Drug-Induced Hypertension)
Orthostatic hypotension
Related to impaired baroreflex function (probably also related to stiffening of the carotid arteries [15]), venous insufficiency, varicosities, and diabetic neuropathy
A significant problem, especially in older hypertensives
Orthostatic hypotension is a predictor of poor outcomes in older individuals, and when compounded by changes in skeletal health and impaired equilibrium, may cause falls
Secondary Hypertension
Acute Kidney Disease
Acute glomerular disease may result in volume retention and hypertension due to increased sodium reabsorption
Acute vascular injury due to vasculitis or connective tissue disease (e.g. SLE, scleroderma) may induce hypertension by increased activation of the RAAS triggered by ischemia
Chronic Kidney Disease (CKD)
Many causes of CKD may lead to hypertension through sodium retention and volume expansion, increased activity of the RAAS due to ischemia, and enhanced sympathetic tone
Renovascular Hypertension
Most common form of secondary hypertension
Usually related to renal artery stenosis (RAS) due to atherosclerosis of the large renal arteries or their ostia
When stenosis exceeds 70 % of the diameter (about 90 % reduction in cross-sectional area), a hemodynamically significant decrease in blood flow results in decrease of intraglomerular pressure with subsequent activation of the RAAS and increased sodium reabsorption
RAS is a manifestation of widespread atherosclerosis that may involve other arterial beds (cerebrovascular, coronary, peripheral)
Stenoses of renal arteries, detected by invasive or non-invasive diagnostic modalities are not uncommon in the elderly, but these may be incidental and non-hemodynamically-significant
In addition to controlling hypertension, revascularization of significant RAS should improve GFR or slow the decline of renal function if the stenosis is the primary cause of renal dysfunction, which is not always the case [18]
In clinical trials of patients with RAS, there has not been a marked clinical benefit from revascularization procedures
Primary Aldosteronism (PA)
Relatively common cause of resistant hypertension (hypertension despite the use of at least three antihypertensives)
Usually associated with adrenal hyperplasia (usually bilateral) or an adrenal adenoma
May also be caused by familial hyperaldosteronism, adrenal carcinoma, or ectopic aldosterone-producing tumors
Diagnostic clues include suppressed plasma renin activity, high aldosterone, and hypokalemia (may not be present) in a hypertensive patient [19]
Diagnostic approach includes measurement of
Plasma renin activity (PRA), plasma renin concentration (PRC), and plasma aldosterone concentration (PAC), as well as random plasma aldosterone concentration-to-plasma renin activity (PAC/PRA) ratio
PAC/PRA ratio > 25 suggests PA, while normal and hypertensives without PA have ratios < 10
If PAC/PRA ratio suggests PA, one or more confirmatory tests should be performed, including [20]
Measurement of urinary aldosterone excretion after oral sodium chloride loading (>12 μg/24 h after 200 mmol/day (∼6 g/day) sodium intake suggests PA)
Measurement of PAC after IV sodium chloride loading (PAC > 10 ng/dL) after infusion of 2 L normal saline over 4 h suggests PA
Fludrocortisone suppression test (upright PAC > 6 ng/dL after 4 days suggests PA)
Captopril challenge (PAC, normally suppressed by 25–50 mg of captopril, remains elevated in PA, while PRA remains low)
Certain medications (e.g. aldosterone receptor antagonists (ARA)) must be held during testing
If confirmatory tests are positive, patients should undergo adrenal CT
Selective adrenal vein sampling may be used to distinguish unilateral from bilateral adrenal involvement in cases where surgery (unilateral adrenalectomy) is an option
For unilateral adrenal involvement or for extra-adrenal lesions, surgical resection is often primary therapy
Medical treatment (e.g. for bilateral adrenal hyperplasia) is based on the use of ARAs
Thyroid Disease
Both hyperthyroidism and hypothyroidism may be associated with hypertension.
Cushing’s Syndrome
Increased ACTH levels, whether iatrogenic, from adrenal tumors, or from other paraneoplastic activity, can lead to hypertension, which may be severe
Pheochromocytomas
Rare catecholamine-producing tumors that can cause paroxysmal hypertension
Aortic Coarctation
Relatively common congenital abnormality that leads to predominately upper-extremity hypertension secondary to mechanical obstruction (typically distal to the brachiocephalic circulation)
Obstructive sleep apnea (OSA)
Associated with an increased incidence of hypertension
OSA should be treated due to a variety of sequelae, including fatigue, systemic and pulmonary hypertension, and all-cause and CAD-related mortality
May be related to other conditions (e.g. obesity and dyslipidemia) and to morbid events (e.g. HF and stroke) [21]
Drug-Induced Hypertension
Medication use is an important cause of secondary hypertension
Causes include NSAIDs, stimulants, and sympathomimetic decongestant agents and oral contraceptive pills.
NSAIDs exert anti-inflammatory activity by inhibiting the production of prostaglandins that mediate inflammation. This inhibition, however, may result in decreased renal function, sodium and water retention, BP elevation, and HF
Diagnosis of Hypertension
Techniques
Blood pressure, especially SBP in elderly individuals, exhibits variability with successive BP measurements and environmental changes such as temperature and emotional state
It is important to measure the pressure several times in a comfortable position after sitting for 5 min
Orthostatic changes should be ascertained by measuring the pressure after standing for 1–3 min
Pseudohypertension, a measurement of a high BP value in the presence of normal intraluminal BP because of noncompressible arteries
May occur in older individuals, but is uncommon
The Osler maneuver (palpable radial or brachial artery when the cuff is inflated above SBP), may be used, although sensitivity and specificity are not very high
Definitive diagnosis requires intraarterial measurement
Home BP monitoring
Should be performed using a reliable automated device
Measurements made three times in the morning and three times in the evening for seven consecutive days
An inexpensive and reliable method of monitoring antihypertensive therapy
Ambulatory BP is a predictor of target organ damage as well as outcomes that surpasses office BP [24]
Ambulatory BP measurement is now recommended in the National Institute for Health and Clinical Excellence (UK) guidelines to confirm the diagnosis following an initial elevated BP measurement in the clinic [25]
Association with Risk
Data from the Framingham Study have shown that in younger ages, DBP is more important in determining risk of CHD while in older individuals, the risk primarily is determined by SBP ([26], Fig. 5-4)
Figure 5-4
Relative importance of DBP and SBP as predictors of CHD as a function of age. CHD coronary heart disease (Used with permission from Franklin et al. [26])
In older patients, lower DBP is associated with higher risk
Studying persons aged 50–79 years without clinical evidence of CHD, the investigators reported that CHD risk increased with lower DBP for a given SBP, suggesting that higher pulse pressure determines the risk in older individuals ([27], Fig. 5-5)

Figure 5-5
Joint influences of SBP and pulse pressure on CHD risk (Used with permission from Franklin et al. [27])
This relationship could be explained by
Decreased coronary flow
A stiffer aortic reservoir related to older age
Comorbidities (e.g. diabetes)
Lifestyle factors (e.g. smoking)
Sequelae of Hypertension
Target Organ Damage
Hypertension results in damage to the arterial system, brain, heart, eyes, and kidneys.
Peripheral arterial disease (PAD) is frequently associated with hypertension
PAD is likely to occur in the same patients who have cerebrovascular disease and CHD and is associated with a marked increase in the occurrence of acute myocardial infarction (MI) and stroke
Hypertension is an important risk factor for the development of abdominal and thoracic aortic aneurysm and aortic dissection
The probability is increased among smokers and those with connective tissue disorders
BP control is very important and surgery is necessary when the aneurysms reach specific dimensions since mortality following rupture is extremely high
Hypertensive retinopathy with arteriovenous nicking, arteriolar narrowing, and in some cases hemorrhages, exudates, and papilledema increases in frequency with age and SBP [28]
Diabetes mellitus (DM), a current worldwide epidemic, increases the risk in hypertensive patients and interacts with hypertension in causing CV events, CKD, and HF [29, 30]
Obesity, another public health issue, is related to and may be causative of diabetes, with the majority of the population being either obese (BMI >30) or overweight (BMI > 25) [31]
Morbid and Mortal Events
Hypertension accounts for more attributable deaths worldwide than any other risk factor, whereas smoking and high cholesterol are second and third, respectively [32]
The causes of death related to hypertension are CHD, stroke, HF, and CKD, especially when hypertension coexists with diabetes ([33], Fig. 5-6)
Figure 5-6
Elevated SBP is a strong risk factor for cardiovascular mortality (Used with permission from Flack et al. [33])
Age is a major determinant of risk for both stroke and CHD events
BP tends to increase with age and the relative risk imposed by a given BP level decreases with age< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree