Chapter 38
Hypercoagulable States
Howard A. Liebman, Ilene Ceil Weitz
Thromboembolism is an enormous problem across the spectrum of medicine. Approximately 10 million individuals in the United States have symptomatic peripheral artery disease, and approximately 100,000 arterial reconstructive procedures are performed annually.1 In the United States and Europe, more than 600,000 people will experience a venous thromboembolism (VTE), and nearly 20% will die as a result.2 The incidence of arterial embolism and VTE is highly age dependent, contributing significant morbidity and mortality to an aging population.3–5
More than one hundred fifty years ago, the great German pathologist, Rudolf Virchow proposed the concept known as Virchow’s triad. He observed that thrombosis occurred when the following three situations were present; vascular wall (endothelial) injury, stasis of blood, and changes in the consistency of blood that enhance coagulation (hypercoagulability). An understanding of the latter, now termed the hypercoagulable state, was least apparent and could not be further characterized until there was a greater understanding of the normal mechanisms of hemostatic regulation (see Chapter 34). In the last 40 years, a number of inherited and acquired hemostatic disorders have been characterized that are associated with an increased risk of venous and/or arterial thrombosis. In most circumstances, the relationship between specific hemostatic defect and the hypercoagulable state is readily apparent by the respective role in normal hemostasis. However, the mechanism(s) by which other well-documented hypercoagulable defects, such as the antiphospholipid syndrome or elevated homocysteine, contribute to an increased risk of venous and arterial thrombosis remain poorly understood. The interactions of these hypercoagulable defects, alone or in combination, or when combined with other transient factors, such as vascular injury from surgery or trauma, can result is a significant increased risk of thrombosis. The interaction between inherited hypercoagulable defects and acquired additional factors, such as age or acute illness, can result in what has been termed an increased “thrombosis potential,” which upon reaching a “thrombosis threshold,” can result in symptomatic thromboembolism.6
Pathophysiology
Hemostasis is a highly organized series of reactions involving platelet adhesion and activation to form the platelet plug, followed by activation of coagulation proteins in a series of controlled enzymatic reactions to generate thrombin. Thrombin potentiates platelet aggregation and activation and acts on fibrinogen to generate the insoluble fibrin clot. Under normal conditions, these reactions occur on the endothelial surface only at sites of endothelial injury. This limits the size of the clot and allows blood to remain liquid and flowing. When this balance is altered, excess thrombin is generated, and abnormal thrombosis may occur. Therefore, thrombosis can result from defects in normal hemostasis that increase either the procoagulant activity or decrease the naturally occurring anticoagulants. These hypercoagulable defects have been termed thrombophilic syndromes and have been further classified as either congenital or acquired thrombophilias.6,7
In addition, there are a group of miscellaneous disorders whose prothrombotic mechanisms are poorly understood. These include elevations of homocysteine (hyperhomocysteinemia) and lipoprotein (a) (Lp[a]). The management of patients with thrombosis with these disorders remains controversial.8–13
Arterial thrombosis, unlike VTE, is associated with conditions that primarily affect the vascular wall and endothelium. Endothelial disruption, which occurs with atherosclerosis, vasculitis (vascular inflammation), infection, trauma, or surgery, is most often associated with an arterial thrombotic event. In well-controlled population studies, the majority of congenital hypercoagulable defects associated with venous thrombosis are not associated with a statistical increased risk of arterial thromboembolism.14–17 The few congenital hypercoagulable defects that may be associated with an increased risk of both venous and arterial thrombosis, such as hyperhomocysteinemia or increased Lp(a), are also associated with an increased risk of arterial atherosclerosis.8,9,18–20 Other defects associated with an increased risk of arterial thromboembolism, such as those observed with increased levels of fibrinogen and von Willebrand factor, are known to enhance platelet function.21,22
Congenital Hypercoagulability
Although the thrombosis potential or risk of thrombosis for inherited prothrombotic defects have been well characterized in a number of prospective and retrospective population studies, it is important to understand that thrombosis is a multigenetic and multifactor disorder. The thrombosis potential for specific congenital thrombophilic abnormalities is classically defined as a relative risk of thrombosis compared with a patient population without these abnormalities.6,7,14–16 In most circumstances, patients who inherit more than one abnormality have a significantly higher risk of thrombosis potential or relative risk of thrombosis.6,7,14–16,23 However, patients may have additional risk factors, such as aging, oral contraceptives (OCs) use, hormone replacement therapy (HRT) use, pregnancy, cancer, infection, trauma, or surgery. In these circumstances, a patient’s individual risk can also be increased by a factor that is more than the sum of each individual risk factor.23
Classification
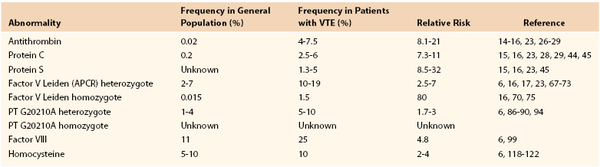
Crowther and Kelton7 proposed a simple classification system that divides the congenital hypercoagulable (thrombophilic) states associated with VTE into two broad groups (Table 38-1). The first group constitutes defects associated with the reduced levels of the natural anticoagulants, such as antithrombin, protein C, and protein S.7 The defects in this “loss of inhibition” group are much less common, but are associated with a significantly higher risk of thrombosis.7 The second group is associated with defects that result in a “gain in procoagulant function” due to increased levels or function of coagulation factors.7 These include factor V Leiden (activated protein C resistance [APCR]) and prothrombin G20210 mutations, increases in coagulation factors VIII, IX, and XI, and the dysfibrinogenemias. Although these defects have a lower thrombosis potential, they are more frequently found in the general population, and therefore, more commonly associated with clinical thrombosis. The understanding that certain defects alone or in combination can be associated with a significantly higher risk of thrombosis may be important in determining the physician’s approach to antithrombotic prophylaxis, duration of anticoagulation after venous thrombosis, and family screening for patients with these defects.
Group 1 Thrombophilia
Group 1 includes deficiencies of the naturally occurring anticoagulant factors antithrombin (AT-III), protein C, and protein S. All are rare, representing less than 1% of the population.7 However, they are highly prothrombotic, with 30% to 50% of carriers (heterozygote) having a symptomatic thrombotic event before they reach 60 years of age.7 A significant number of carriers will have had a spontaneous thromboembolic event before the age of 40 years. Frequently, there is a strong family history of venous thrombosis. Although the risk of thrombosis is high, routine prophylactic anticoagulation in ambulatory healthy individuals has not been demonstrated to be of benefit and should be reserved for high-risk situations, such as surgery, sepsis, pregnancy, and immobilization.7 Because of the high risk of recurrence, with group 1 deficiencies and patients homozygous for certain group 2 abnormalities, lifelong anticoagulation may be recommended after a spontaneous thrombotic event.7,24
Antithrombin Deficiency
Pathogenesis and Incidence.
Physiologically, AT-III is the most important inhibitor of thrombin and other activated clotting factors (e.g., factors Xa, IXa, and VIIa). AT-III physiologic activity is enhanced 1000-fold by the binding of naturally occurring or administered heparin or heparin sulfates.25 AT-III deficiency is rare, reportedly occurring in an estimated 0.02% of the general population in a study that screened samples from healthy blood donors.26,27 It has been reported in 4% to 7.5% of patients with VTE.14–16,28,29 AT-III inheritance is autosomal dominant.30 More than 250 mutations within the molecule have been described.31 Homozygosity, particularly for AT-III deficiency types I and II, is extremely rare and appears to be incompatible with life. Homozygosity for type III AT-III deficiency results in a severe thrombophilic phenotype.32
Types.
There are three general subtypes of AT-III deficiency.31 Type I is characterized by decreased AT-III functional activity and antigen. Type II defects are AT-III mutations that have reduced functional activity, but normal antigen levels resulting from a mutation in the active inhibitory site on the protein. Type III AT-III mutations are characterized by moderate decreased activity due to impaired interaction with heparin. Screening for AT-III deficiency should always be undertaken using a functional assay, because screening with an antigen assay may fail to diagnose type II and III defects. In the presence of low AT-III activity, further characterization can be made with an antigen assay.
Patients with AT-III deficiencies are at a significantly higher risk of thrombosis than patients with other congenital deficiencies. Approximately 60% of carriers of type I and II deficiencies will have a thrombotic event by the age of 60 years. The risk for type III deficiency may be lower.33,34 A strong family history of thrombosis is usually present. A Spanish Multi-Center study reported the relative risk of thrombosis in these thrombophilic families as 21-fold.29 A multicenter, multinational European Prospective Cohort on Thrombophilia (EPCOT) study reported an adjusted relative thrombotic risk of 17.5 (95% confidence interval [CI], 9.1-33.8).23 After the diagnosis of AT-III deficiency is made in an individual with thrombosis, screening of family members is recommended.
Clinical Presentation and Management.
The clinical presentation of AT-III deficiency is predominantly lower extremity thrombosis with or without pulmonary embolism.30,33,35 Recurrent events are common, and atypical thrombotic events involving the portal, mesenteric, and hepatic venous system, or cerebral veins have been reported.29,40,41 Arterial events are rare, and patients are not at increased risk more than the unaffected adult population.14–16,23 Pregnancy is a particularly high-risk situation, and prophylaxis with heparin is indicated throughout pregnancy and in the immediate postpartum period.35,36 Patients with breakthrough events can receive AT-III concentrates.37 An acquired form of AT-III deficiency has been reported in pregnant women with the fatty liver syndrome with disseminated intravascular coagulation.38 Treatment with plasma or AT-III concentrates rapidly reverses the coagulopathy.38
Protein C Deficiency
Pathogenesis and Incidence.
Protein C is a vitamin K-dependent anticoagulation protein that is activated by thrombin to activated protein C (APC).42 When thrombin levels are high, thrombin binds to the endothelial protein receptor, thrombomodulin (TM), which changes the specificity of thrombin from cleaving fibrinogen or activating platelets to activating protein C. Protein C binds to its specific endothelial receptor, termed the endothelial protein C receptor, which enhances its activation. APC is a potent serine protease anticoagulant that cleaves the coagulant cofactors VIIIa and Va, thus modulating thrombin generation and subsequent clot formation.42,43 Deficiency of protein C is found in 0.2% of the general population, and in 2.5% to 6% of patients with VTE.28,29,44,45
Types.
Similar to AT-III deficiency, multiple mutations resulting in protein C deficiency have been reported. These mutations have been classified into two general subtypes: type I mutations have reduced functional and antigenic protein levels; and type II mutations have reduced functional levels but preserved antigen levels of the protein.46 Adult heterozygous patients with protein C deficiency usually have activity levels of less than 60%.
Clinical Presentation and Management.
Patients who have VTE usually present in the lower extremities. Unusual sites of thrombosis have been reported and are similar to those seen with AT-III deficiency.42,43,45,46 Although rare arterial events have been reported, large cohort studies do not support an increased risk of arterial events.47 In protein C deficient patients from thrombophilic families who present with an unprovoked (idiopathic) thrombosis, recurrent thrombotic events are frequent. Life-long anticoagulation should be considered in these patients, particularly those who present before the age of 40 years.
Homozygosity for protein C deficiency, with absent protein C activity, may present at birth as a neonatal disorder termed purpura fulminans.48 This disorder is characterized by diffuse microvascular thrombosis of the skin and systemic organs. Immediate treatment with heparin, plasma, or protein C concentrates can be life saving.48 The majority of homozygous neonates with protein C deficiency will have functional levels less than 20% of normal.48
A similar severe disseminated thrombotic disorder, characterized by skin necrosis, can occur in heterozygous patients with protein C deficiency treated with higher doses of warfarin, usually without concomitant anticoagulation with heparin.49,50 The syndrome, termed warfarin necrosis, results from the disproportional decrease in protein C in comparison to other procoagulant vitamin K-dependent coagulation factors. Patients presenting with this disorder should be treated with fresh frozen plasma, vitamin K, and heparin.49,50 The syndrome can be prevented by initiating oral anticoagulation with lower doses of warfarin and concomitant use of heparin.
Protein S Deficiency
Pathogenesis and Incidence.
Protein S is the vitamin K-dependent cofactor necessary for the inactivation of factors Va and VIIIa by APC. A deficiency in protein S is phenotypically similar to protein C deficiency. Protein S exists in two forms: the functionally active free form that usually constitutes 20% to 40% of the total protein, and the remaining 60% to 80% that is active and bound to complement binding protein C4b.51,52 Most patients with protein S deficiency will have activity levels between 50% and 75% of normal.51–53
Types.
Similar to the other natural anticoagulant proteins, protein S deficiency can be classified into 3 subtypes: type I is characterized by reduced functional and antigen protein levels; type II has reduced functional activity, but normal antigen levels; and type III has normal antigen levels, but reduced free active protein S due to enhanced C4b binding.54 Type I and type III protein S deficiencies are the most common forms of the deficiency encountered and do not appear to differ in their risk of venous thrombosis.55
The measurement of protein S activity and antigen can be confounded by a number of physiologic and clinical conditions. In pregnancy, protein S levels fall in the second and third trimester.56,57 Reduced protein S levels have also been reported in patients with active cancer, lupus erythematosus, antiphospholipid antibody syndrome, sepsis, chronic inflammatory disorders (e.g., inflammatory bowel disease) and in advanced HIV disease.58–60
Clinical Presentation and Management.
Protein S deficiency is clinically characterized by venous thrombosis and has been frequently reported in association with venous thrombosis in atypical sites.51–53,61,62 These reports may be confounded by other comorbidities in these patients that can be associated with acquired protein S deficiency. In addition, several reports have suggested a relationship between low protein S levels and arterial thrombosis, including a reported association between low free protein S and cardiolipin antibodies in stroke patients.63
Like protein C deficiency, homozygous deficiency can be associated with neonatal purpura fulminans. Approach to management is similar to that of homozygous protein C deficiency.64 Warfarin necrosis can also develop in heterozygote protein S patients.64
Group 2 Thrombophilia
Although associated with a lower thrombosis potential than Group 1 thrombophilia, Group 2 hypercoagulable disorders are more frequently found in the general population and are found in a greater proportion of patients with VTE. They represent gain of function mutations resulting in increased thrombin generation. They are typified by either increased synthesis of specific coagulation factors or as observed with factor V Leiden, resistance to the inactivation of this cofactor by APC.
Factor V Leiden (Activated Protein C Resistance)
Pathogenesis and Incidence.
Factor V is a cofactor that accelerates the conversion of factor II (prothrombin) to thrombin by factor Xa. Under normal circumstances, factor V is degraded by the serine protease, APC, which cleaves the protein at two sites. Factor V Leiden has a mutation in the 506 position that results in a substitution of glycine for arginine. This renders one of the factor V cleavage sites resistant to the action of the APC, which, like all coagulation serine proteases, cleaves arginine bonds.65–67 This results in a slowing of the inactivation of the cofactor, which leads to increased thrombin generation.
Factor V Leiden is a common mutation, occurring in approximately 2% to 7% of individuals of European ancestry.67–69 It can be found in nearly 10% of people with VTE and in 30% to 50% of individuals being evaluated for thrombophilia.67–70 The mutation is very rare in native Asians and Africans.69,70 The mutation is also rare in African Americans (0.6%) and has not been reported in Native Americans.69,70 Compared with patients with group 1 thrombophilia, patients with factor V Leiden have a lower relative risk of thrombosis, estimated between 2.5- and 7-fold.16,17,23,71–74 A cross-sectional study from Italy found that only 6% of carriers of the mutation developed a thromboembolic event by the age of 65 years.75 Homozygotes are at much higher risk then heterozygotes, with an estimated relative risk of 80-fold.16,71,76 However, heterozygotes with combined defects have a significantly increased risk of VTE.16,23,75 A second, very rare, mutation of the second factor Va cleavage site (Arg306Thr) has also been reported to be associated with increased risk of thrombosis, whereas other studies have failed to find a relationship of this mutation with the development of VTE.77
Clinical Presentation and Management.
The clinical presentation of thrombosis with factor V Leiden is overwhelmingly venous. Although rare, unusual sites, such as cerebral vein and retinal vein thrombosis, have been reported.78,79 The onset of thrombosis is frequently at an older age than seen in patients with type 1 thrombophilia.17 In the Physicians Health Study, the risk of VTE in men with the factor V Leiden mutation did not become statistically significant until after the age of 50 years.17 The study also found no association with the factor V Leiden and an increased risk of stroke or myocardial infarction.17 Thrombosis is frequently triggered by transient risk factors, such as a prolonged plane flight, oral contraceptive (OC) use, or pregnancy.80–83 In women carriers of the mutation, the reported thrombosis risk associated with the use of second-generation OCs varies widely, ranging from 6- to 50-fold.80–83 The wide variation reported in the thrombotic risk of OCs may be explained, in part, by a higher risk of thrombosis in women more than 30 years old who are taking OCs and some variation in the specific OCs used in the European studies, some of which contain prothrombotic progesterone substitutes.83
There is no excess mortality in carriers of the factor V Leiden mutation. No prophylaxis is recommended for carriers except what is recommended by guidelines for surgical interventions. Antepartum prophylaxis is not recommended for women who have not had a previous thrombotic event or a history of recurrent fetal loss.84 The risk of recurrent VTE after cessation of oral anticoagulation is not greater than that observed in other patients with unprovoked VTE.85
Prothrombin Gene Mutation G20210A
Pathogenesis and Incidence.
The prothrombin G20210A mutation is an abnormality located at the untranslated 3′ end of the prothrombin gene that results in increased plasma levels of prothrombin. The mutation affects the 5′ end cleavage signal, leading to increased prothrombin mRNA stability.86 The thrombotic risk is relatively low.87–89 The gene frequency in the European population is about 1% to 4%, with the greatest frequency in southern Europe and Spain.90–91 It is present in 5% to 10% of patients with VTE, and 15% of patients with thrombophilia.87–91 Similar to factor V Leiden, the prothrombin G20210A mutation is very rare in native Asians, Africans, African Americans, and Native Americans.92 Many carriers with a history of VTE have co-inheritance of the factor V Leiden mutation.23,93 The relative risk of thrombosis is low in carriers of the prothrombin mutation, ranging from two- to threefold higher in carriers compared with noncarriers of the mutation.94,95
Clinical Presentation and Management.
The clinical presentation is predominantly venous thrombosis of the lower extremities, and unusual sites are rare.87–89,94,95 Some controversy exists as to whether the prothrombin mutation is associated with an increased risk of arterial thrombosis.95–97 In carriers of the mutation who develop thrombosis, studies to date have shown either no increase in risk or only a slight increased risk of recurrent VTE after discontinuation of anticoagulation.95,98
The risk of VTE in women on OCs has been reported to be significantly increased, similar to that reported for factor V Leiden.94 Women who are carriers of both the prothrombin G20210A mutation and the factor V Leiden mutation have a markedly high risk of VTE.94 An association between the development of cerebral venous thrombosis in women carriers of the prothrombin mutation taking OCs has been reported, in which 20% of patients carried the mutation versus only 3% of controls.99
Elevated Factors VII, XI, and IX
Pathogenesis and Incidence.
Koster et al.100 first reported an increased risk of VTE in patients with an elevated factor VIII coagulant protein of more than the 90th percentile (>150%). Factor VIII activity levels more than 150% were associated with an adjusted relative risk of 4.8% compared with factor VIII levels 100% or less.100 These elevations appear to be independent of ABO blood type and were measured in patients without evidence of inflammation confirmed by a normal erythrocyte sedimentation rate (ESR) and C-reactive protein.101,102
Subsequent studies have supported this observation and found both a family and racial clustering suggestive of an inherited propensity for increased factor VIII levels.101,103 A study of African-American women found a statistically higher level of factor VIII compared with the white and Asian population in the United States.104 Unlike female carriers of the factor V Leiden and prothrombin mutations, the use of OCs did not appear to significantly increase the risk of VTE.105 Elevations of factor VIII activity have also been associated with an increased risk of recurrent VTE.106
The measurement of factor VIII activity is confounded by the fact that factor VIII, along with its carrier protein, von Willebrand factor, is an acute phase reactant and increases with bleeding and inflammation.101,102 Therefore, measurement of factor VIII activity should be performed with a simultaneous acute phase marker, such as the ESR or C-reactive protein. The assay should also be repeated at least twice at distant time intervals.100–102 Each laboratory must define the 90th percentile range for its own population to determine the patient population at risk.
Clinical Presentation and Management.
The clinical presentation of patients with elevations in factor VIII activity is predominantly VTE of the lower extremities.100 Because factor VIII levels increase with inflammation, elevation of this coagulation protein is an important cofactor in the development of thrombosis associated with infection, inflammatory bowel disease, and cancer. There is controversy as to whether increased levels of factor VIII are associated with arterial thrombosis, because elevations in factor VIII activity are associated with increases in von Willebrand factor. Increased levels of von Willebrand factor have been shown in population-based studies to be associated with an increased risk of arterial thrombosis.107
Increased levels of factors IX and XI have been associated with a twofold increase in risk of VTE.108,109 These are relatively weak risk factors for thrombosis, but if combined with other defects, they may become significant. To date, no molecular markers have been reported to characterize these elevations in factors VIII, IX, and XI.110
Hyperhomocysteinemia
An association was made between markedly elevated levels of homocysteine and arterial vascular disease in individuals with homocysteinuria.111,112 Additional studies confirmed this association and found additional evidence that individuals with homocysteinuria also experience an increased incidence of VTE.111 Subsequent studies found an association between elevations of plasma homocysteine and an increased risk of atherosclerosis and arterial thrombosis in apparently healthy individuals.113–121 Additional studies that focused on risk factors for venous thrombosis reported a similar association.121–124
Homocysteine metabolism involves two enzymatic pathways that require essential vitamin cofactors: folate, vitamin B12, and vitamin B6 (pyridoxine).125 The vitamine B6-dependent pathway involves the enzymatic conversion of homocysteine to cystathionine by the enzyme cystathionine-β-synthase (CBS).112,125 The second pathway involves re-methylation of homocysteine back to methionine requiring folate, vitamin B12, and the two enzymes 5,10-methylenetetrahydrofolatate reductase (MTHFR) and methionine synthetase.125 The primary mutations responsible for homocysteinuria are in the CBS gene.112 However, in the general population, independent of deficiencies in the vitamin cofactors, a common mutation in the MTHFR gene at position 677 is most frequently associated with elevations in homocysteine.125 This C to T mutation results in a 50% reduction in the enzymatic activity of the gene.125 However, even in MTFR C677T homozygotes, folate supplementation or a diet intrinsically rich in folate can reduce homocysteine levels into the normal range.125,126
The reported mechanisms by which homocysteine increases the risk of both arterial and venous thrombosis include a direct toxic effect on endothelium, enhanced platelet activation, oxidation of low-density lipoprotein cholesterol, an inflammatory decrease in endothelial TM, and an increase in von Willebrand factor and factor VIII.125 However, no single reported effect of homocysteine adequately explains its prothrombotic effect in both the arterial and venous vasculature.
A number of cohort studies and some prospective studies have found a statistically significant association between elevated homocysteine and an increased risk for myocardial infarction and stroke with estimated risks of 2- to 7.8-fold for individuals in the highest quartile.113–115 However, several prospective studies have failed to confirm this association.116–118 Data from the Physicians’ Health Study,118 the Atherosclerosis Risk in Communities Study,119 and the Women’s Health Study116,117 suggest a gender-defined risk for elevated homocysteine in which the risk is most significant in women. Elevations of homocysteine have also been found in case-controlled studies to be a weak risk factor for VTE, with a relative risk of only 2 to 4.120–124 Meta-analyses further confirmed an increased risk in patients with homocysteine levels more than the 95th percentile.124
Complicating the issue of elevated homocysteine as a risk factor for both arterial and VTE disease is the lack of response, in randomized controlled trials, to lowering homocysteine in reducing the risk of recurrent arterial10–12 and VTE13 disease in patients treated with vitamin therapy.
The measurement of homocysteine in patients can be complicated by comorbid conditions, such as vitamin deficiency, renal insufficiency, and improper plasma collection and handling. Measurements are best performed using freshly collected plasma, preferentially with patients in the fasting state. It is reasonable to repeat the assay on at least two separate occasions. Studies to date do not support an advantage for determination of the MTHFR genotype over direct measurement of homocysteine.126
Lipoprotein(a)
Lp(a) is a serum lipoprotein composed of a low-density lipid particle with a disulfide link to a long polypeptide chain, apolipoprotein (a).20,127 The protein has “kringle-like” domains that compete with tissue plasminogen activator, plasminogen, and plasmin for binding to fibrin and endothelial annexin II, thereby inhibiting fibrinolysis.127,128 The plasma levels of Lp(a) vary greatly within and between different racial populations, with African Americans having higher levels.129 Also, Lp(a) may increase as an acute phase reactant130,131 and has been reported to be elevated in certain inflammatory rheumatologic disorders.132
Early retrospective studies suggested a relationship between elevated levels of Lp(a) and the risk of premature atherosclerosis and arterial thrombosis.133–135 However, prospective studies have been less supportive and at the most suggest only a small increase in risk for individuals with elevated plasma Lp(a).136–142 Additional reports have suggested a role for elevated Lp(a) as an independent risk factor for VTE,143,144 although a failure to find an association has been reported by other investigators.145
Sticky Platelet Syndrome
Sticky platelet syndrome (SPS) is an inherited, autosomal dominant disorder associated with early-onset myocardial infarction and peripheral vascular disease.146–148 Although most often associated with arterial vasculopathy, VTE has been reported.146–148 A causal relationship to early miscarriage has also been reported. Patients usually present with a history of myocardial infarction or thromboembolism as young adults. The events often are precipitated by stress.146–148 The defect appears to be common in patients with unexplained thromboembolic events. In an analysis of 200 patients and family members identified with SPS, 21% had arterial thromboembolic events and 13.2% had VTE events.147 SPS platelets demonstrate hyperreactivity to epinephrine and adenosine diphosphate (ADP) even with dilution, but have normal responses to thrombin, collagen, and arachadonic acid.146–148 Three types of platelet responses have been noted: type I is hyperreactive to both ADP and epinephrine; type II is hyperreactive to epinephrine only; and type III is hyperreactive to ADP only. Increased arterial events may be mediated through polymorphisms of glycoprotein IIIa allele PLA-A2.149 Although other investigators have reported similar hyperreactivity of platelets in patients with ischemic stroke,150 there remains controversy as to whether SPS represents a true congenital prothrombotic syndrome. In patients with documented platelet reactivity and thrombosis, low-dose acetylsalicylic acid (81 mg) appears to be effective in inhibiting platelet hyperreactivity.148
Idiopathic (Unprovoked) Venous Thrombosis
Unprovoked or idiopathic venous thrombosis is defined as the development of deep vein thrombosis and/or pulmonary embolism in the absence of known genetic prothrombotic mutations, permanent factors, or acquired risk factors. Patients who develop VTE provoked by surgery, trauma, immobilization, pregnancy, or female hormone intake are at low risk of recurrent thrombosis.151,152 Patients with unprovoked VTE have a recurrence risk of 5% to 10% per year, with nearly 50% developing a recurrent event by 10 years.151,152 A prospective study that screened 66 patients with idiopathic venous thrombosis found abnormalities in 26 (39.3%) patients when they were screened for thrombophilia (antithrombin, protein C, protein S, factor V Leiden, prothrombin G20210A, antiphospholipid antibodies).153 Therefore, 60% of patients with unprovoked VTE have no underlying known major inherited or acquired thrombophilia and still remain at high risk of recurrent VTE. It has been proposed that an underlying inflammatory state may be responsible for the increased risk of VTE in patients with unprovoked events.154,155 Laboratory assessment of patients with idiopathic VTE have demonstrated higher levels of interleukin-6 and -8 with low levels of interleukin-10 compared with age- and sex-matched controls.156 It is notable that the same inflammatory markers are linked to an increased risk of atherothrombotic disease.154–157
Acquired Hypercoagulability
An increased risk of thrombosis can be associated with a variety of acquired abnormalities. Disorders such as the antiphospholipid antibody syndrome (APLAS) and cancer are significant prothrombotic syndromes.158,159 Common clinical situations such as cancer, pregnancy, infection, and estrogen use are transient causes of hypercoagulability.160–162 Surgery is a well-documented transient cause of hypercoagulability in which the risk of thrombosis is related to a number of factors, such as the type of surgery, duration of surgery, age of the patient, and other patient comorbidities.162 A significant iatrogenic thrombotic disorder is heparin-induced thrombocytopenia (HIT), in which early diagnosis and treatment may be life-saving.163 Chronic inflammatory and autoimmune disorders, such as inflammatory bowel disease, Behcet’s syndrome, or lupus erythematosus, with and without antiphospholipid antibodies, are also associated with a significant risk of thrombosis.164–167
Acquired elevations in factor VIII levels or depressions in protein S may be an important contributing factor to a number of prothrombotic disorders, including cancer, pregnancy, infection, and chronic inflammatory disorders. In patients with cancer, the expression of tissue factor by the malignant cell further increases the thrombotic risk.168,169 Paroxysmal nocturnal hemoglobinuria, a rare hemolytic disorder in which nearly half of the patients develop symptomatic thrombosis, has been shown to be associated with both increased platelet activation and increased leukocyte tissue factor expression.170,171 Thrombosis in patients with myeloproliferative syndromes frequently involves unusual sites, such as the portal and hepatic veins, and is more often associated with syndromes associated with the Janus kinase-2 (JAK-2) mutation.172–175 The presence of JAK-2 mutation has also been shown to be associated with thrombosis in the splanchnic, portal, and hepatic veins, even in the presence of normal blood counts.175
Antiphospholipid Antibody Syndrome
The APLAS is one of the more common causes of acquired hypercoagulability.158,159 The syndrome is associated with an increased risk of both arterial and venous thrombosis.158,159 Although the APLAS can occur with systemic lupus erythematosus (SLE), 50% of the patients do not fulfill criteria for lupus or other autoimmune disorders.176 The syndrome is characterized by the presence of antibodies that inhibit in vitro coagulation reactions, the lupus anticoagulant (LA), and antibodies that bind to anticardiolipin and β2-glycoprotein.158,159 Clinical criteria include a history of either thrombosis and/or pregnancy complications with fetal loss.177
Pathogenesis and Incidence
There is strong epidemiologic evidence to support a relationship between the presence of these antiphospholipid antibodies and thrombosis.158,159,178 There appears to be a differential risk with the highest risk of thrombosis associated with the presence of an LA and high titer immunoglobulin-G (IgG) anticardiolipin antibody.158,178 The Leiden Thrombophilia Study, a large population-based, case-control study of unselected patients with a first episode of venous thrombosis, found a 3.6-fold increased risk for deep venous thrombosis for individuals positive for LA (odds ratio [OR], 3.6; 95% confidence interval [CI], 1.2-10.9).178 However, patients who were positive for both the LA and either antiprothrombin or anti-β2-glycoprotein-1 antibodies had an estimated 10-fold increased risk of VTE (OR, 10.1; 95% CI, 1.3-79.8).
The syndrome is something of a paradox in that this thrombotic disorder is characterized by antibodies that prolong in vitro coagulation tests, most commonly, the activated partial thromboplastin time (aPTT). The mechanism(s) by which these antibodies result in thrombosis remains unclear.179 Activation of monocytes, platelets, and endothelial cells by antibody/β2-glycoprotein-1 complexes has been implicated in the etiology of thrombotic events.180–183 Antibodies to annexin II on endothelial cells, tissue plasminogen activator, and plasmin have been proposed as additional antigenic targets.182 Complement (C5a) mediated inflammation has been demonstrated to be associated with increased thrombogenicity and recurrent fetal loss.179,183
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree