Hybrid Revascularization
Soroosh Kiani
Molly Szerlip
Robert Poston
Introduction
The standard approach to coronary artery bypass grafting (CABG) involves a full sternotomy with bypass grafts placed to all appropriate coronary targets. There are 200,000 cases/year in the United States that use this approach, making it one of the most thoroughly investigated, improved, optimized, and streamlined surgical procedures in all of medical history. The results of a given program can be risk stratified, compared to national norms using well-defined benchmarks established by the Society of Thoracic Surgeons (STS) National Database, which drives continuous improvement. These efforts have turned CABG into a fungible commodity that is reproducible in a cost-effective manner by most cardiothoracic surgeons. This cost efficiency has major implications for our healthcare system because the annual expenditures for CABG exceed $10 billion.
The technique for a CABG done today remains fundamentally unchanged since it was first developed decades ago via a full median sternotomy, with complete cardiopulmonary bypass (CPB) and an arrested heart, using saphenous vein conduits to create most of the bypass grafts. Less invasive approaches that avoid the sternotomy (e.g., MIDCAB) were developed in the 1990s but are currently limited to less than 0.5% of all CABG cases in the United States. Even more modest improvements aimed at avoiding the side effects of CPB such as off-pump CABG through a full sternotomy (OPCAB) machine (CPB) have failed to achieve widespread adoption.
Robotic-assisted CABG (rCABG) is a less invasive approach to CABG that avoids a median sternotomy. Single-center studies demonstrate that rCABG attenuates the bleeding and infection risk associated with large incisions, reduces postoperative recovery times and convalescence, and shortens the duration of time for pain to resolve. After multiple clinical trials, sternotomy OPCAB has shown no advantage for these endpoints compared to on-pump CABG. This suggests that the sternotomy is an important and underappreciated driver of morbidity and recovery time while the adverse effects of CPB may have been overestimated.
Performed only at selected centers, rCABG has none of the benchmarks, standards, or “best practice” recommendations available for traditional CABG. There is no clear consensus on the best approach to performing the distal anastomoses, either hand-sewn via a left-sided minithoracotomy or created totally endoscopically using the robotic instruments (i.e., TECAB). In addition, most centers only apply rCABG for grafting the left internal mammary artery (LIMA) to the left anterior descending (LAD) coronary
artery. Those patients that require multiple bypass grafts for a complete revascularization are rarely grafted with bilateral IMA (BIMA) conduits during rCABG. However, there is a greater consensus among rCABG surgeons about the utility of staged combination of both percutaneous coronary intervention (PCI) and less invasive LIMA to LAD grafting, known as the “hybrid approach.” Hybrid coronary artery revascularization is tailored in a patient-specific manner so that stenting is used to treat amenable non-LAD lesions while the gold standard IMA graft is used to revascularize the critical LAD. This approach necessitates real time collaboration of a multidisciplinary team, or the “heart-team” approach. The most recent ACC/AHA guidelines have recognized hybrid procedures are a reasonable and viable approach to achieve revascularization in appropriate patients.
artery. Those patients that require multiple bypass grafts for a complete revascularization are rarely grafted with bilateral IMA (BIMA) conduits during rCABG. However, there is a greater consensus among rCABG surgeons about the utility of staged combination of both percutaneous coronary intervention (PCI) and less invasive LIMA to LAD grafting, known as the “hybrid approach.” Hybrid coronary artery revascularization is tailored in a patient-specific manner so that stenting is used to treat amenable non-LAD lesions while the gold standard IMA graft is used to revascularize the critical LAD. This approach necessitates real time collaboration of a multidisciplinary team, or the “heart-team” approach. The most recent ACC/AHA guidelines have recognized hybrid procedures are a reasonable and viable approach to achieve revascularization in appropriate patients.
Standard Candidate
The standard of care for treating multivessel coronary artery disease is conventional CABG or PCI. The hybrid approach is often considered in patients with factors that would limit the success of these gold standards such as a heavily calcified aorta, lack of suitable conduits for grafting, or extensive CAD not amenable to stenting. In addition, some patients are more suitable for a less invasive approach, either due to personal preference or poor surgical candidacy. For patients with stable angina due to multivessel CAD, the target with the highest-grade lesion is addressed as “step one,” of a staged hybrid approach and the remaining target(s) addressed afterward.
Acute Coronary Syndromes
Usually after gaining experience, use of a hybrid procedure can be safely extended to selected cases with acute coronary syndromes. This requires an understanding of the “culprit lesion,” or the vessel causing the acute coronary ischemia. Most typically, the culprit is revascularized first and nonculprit lesions are addressed in a staged fashion afterward. If the culprit lesion is to be addressed by PCI, then the PCI is performed first followed by rCABG in a separate setting during active clopidogrel administration and the staging is reversed if the culprit is best addressed by LIMA grafting. In the case of acute, transmural myocardial infarction, the culprit lesion is usually clearly identifiable while with NSTEMI and unstable angina, the ability to identify the exact lesion is less precise. If the culprit lesion for an acute coronary syndrome is misidentified, the patient is placed at increased risk for myocardial ischemia by the culprit lesion remaining untreated during either surgery or PCI. The risks of CABG in the setting of acute myocardial infarction are known to be increased; whether rCABG reduces this risk remains to be clarified.
Patients at Risk for Bleeding
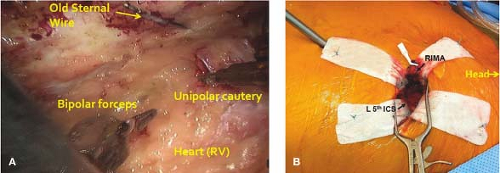
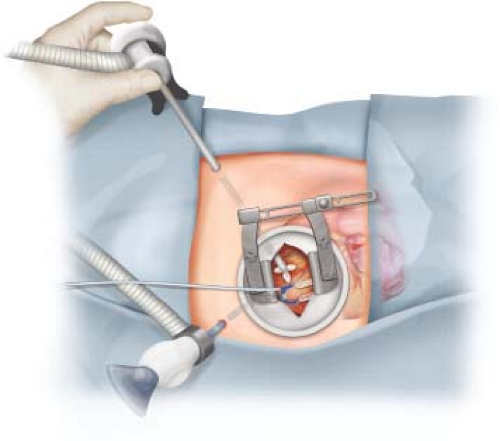
Evidence suggests that hybrid revascularization can be safely applied to patients that are actively treated with potent antiplatelet agents such as clopidogrel up to the day of surgery. Active clopidogrel use increases the risk of bleeding and transfusions after rCABG but the magnitude of risk is far less than is seen after conventional CABG. A unique aspect of the rCABG procedure is that it requires the placement of ports bluntly through the chest wall (Fig. 28.1). When removed, these ports create bleeding sites that can be difficult to detect and treat. We have demonstrated that routine use of a topical hemostatic agent placed locally within these port sites helps to reduce postoperative bleeding and blood product requirements. These findings suggest that undetected bleeding from chest wall sites used for port access has likely been an underappreciated source of morbidity after rCABG.
Redo Surgery
As centers gain experience, candidacy for robotics can be broadened to include those that require reoperative cardiac surgery. Redo cardiac surgery via a repeat sternotomy poses unique risks that have been difficult to avoid, even at experienced centers. Sternal adhesions render the heart prone to injury during sternal reopening and when injury occurs it is associated with a remarkably high mortality rate. Cardiac manipulation to dissect these adhesions can trigger hemodynamic instability, result in prolonged CPB times, excessive bleeding, transfusions, and postoperative cardiac dysfunction. We have found that less invasive surgery helps circumvent many of these complications associated with reoperative sternotomy. Reoperation via a robotic approach improves access to the retrosternal space for precise dissection of adhesions (Fig. 28.2A) and is associated with improved safety of harvesting and grafting the right internal mammary artery (RIMA) (Fig. 28.2B). Reoperative CABG is frequently indicated in patients that have previously undergone harvest of the LIMA while the RIMA is often intact and available for harvest. Harvest of the only remaining IMA at the time of repeat sternotomy may present a risk factor for poor sternal healing and mediastinitis. However, using robotics to circumvent the sternotomy obviates any concerns for healing difficulties or mediastinitis that might otherwise follow procurement of both IMA.
Although the hybrid approach is appropriate for a broad population of patients, careful patient selection is paramount. Patients with unstable hemodynamics or active coronary ischemia (e.g., ST elevations on arrival to the OR) benefit from the full cardiac exposure and access provided by a sternotomy, making them poor candidates for the limited exposure of rCABG. Patients with pulmonary hypertension or significant lung disease are not likely to tolerate the period of single-lung ventilation required during rCABG and are contraindicated for this approach. Relative contraindications include those with unfavorable anatomy or lesions not amenable to complete revascularization through a less invasive approach. Given the impact that the specialized team has on the success of this procedure, rCABG is often not used in patients that present for urgent revascularization “off hours” when the robotic team is not available. Multiple grafts done using the rCABG technique are challenging in those with low left ventricular ejection fractions because surgical access to posterior or lateral wall targets is difficult, even while the heart is decompressed on peripheral CPB support. During the informed consent process, the surgeon should try to determine if the patient might prefer a more stereotyped procedure with a longer “track record” than rCABG. A patient who seems reluctant to accept the often unforeseen risks of innovation or has unrealistic expectations are at increased risk of postoperative decisional regret after rCABG and should be steered toward a traditional approach.
Surgical Strategy for Single versus Multiarterial Grafting for Hybrid Cases
Multivessel CABG via a sternotomy can be performed off-pump as long as the hemodynamics tolerate the cardiac subluxation required to expose coronary targets that are not on the anterior surface. When cardiac manipulation compromises hemodynamics, it can lead to complications related to poor tissue perfusion. The inconsistent ability to manage hemodynamics has been an important reason for the lack of widespread adoption of sternotomy OPCAB. In contrast, the heart maintains normal positioning during the typical hybrid treatment of multivessel CAD because LIMA to LAD grafting during rCABG and PCI require minimal cardiac manipulation (Fig. 28.3). As a result, hemodynamics
remain more stable than either on- or off-pump CABG, thereby making hybrid cases a more reliable way to avoid intraoperative hypotension and reap the advantages of off-pump CABG.
remain more stable than either on- or off-pump CABG, thereby making hybrid cases a more reliable way to avoid intraoperative hypotension and reap the advantages of off-pump CABG.
Several centers have established the feasibility of multivessel CABG to targets other than the LAD. In contrast to isolated LIMA to LAD grafting, maintaining hemodynamics during less invasive multiarterial grafting has proven challenging, particularly when posterolateral coronary targets are planned for grafting. The technical complexity leads to prolonged operative times, and therefore long periods in which single-lung ventilation and CO2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree