Hospital-Acquired Pneumonia
GENERAL PRINCIPLES
Definition
• Hospital-acquired pneumonia (HAP) is pneumonia occurring >48 hours after admission to the hospital.1
• Ventilator-acquired pneumonia (VAP) is pneumonia occurring >48 hours after intubation of the trachea and initiation of mechanical ventilation.1
• Health care–associated pneumonia (HCAP) is pneumonia in patients presenting from the community with the following risk factors:
 Risk factors originally derived from risk factors for health care–associated bacteremia with a resistant pathogen1–3:
Risk factors originally derived from risk factors for health care–associated bacteremia with a resistant pathogen1–3:
 Hospitalization for ≥2 days in an acute care facility within 90 days of infection
Hospitalization for ≥2 days in an acute care facility within 90 days of infection
 Presentation from a nursing home or long-term care facility
Presentation from a nursing home or long-term care facility
 Attending a hospital or hemodialysis clinic
Attending a hospital or hemodialysis clinic
 Receiving IV antibiotic therapy, chemotherapy, or wound care within 30 days of infection
Receiving IV antibiotic therapy, chemotherapy, or wound care within 30 days of infection
 Family member with multidrug-resistant pathogen
Family member with multidrug-resistant pathogen
 Pneumonia-specific risk factors associated with drug-resistant pathogens4:
Pneumonia-specific risk factors associated with drug-resistant pathogens4:
 Recent hospitalization (within 90 days) for ≥2 days or recent antibiotic use
Recent hospitalization (within 90 days) for ≥2 days or recent antibiotic use
 Immunosuppression
Immunosuppression
 Nonambulatory status
Nonambulatory status
 Tube feeding
Tube feeding
 Use of gastric acid suppressive agents
Use of gastric acid suppressive agents
Epidemiology
• HAP/VAP is the most clinically significant hospital-acquired infection and the leading cause of death from all nosocomial infections. The incidence of HAP is estimated to be between 5 and 10 cases per 1000 admissions and is substantially higher in mechanically ventilated patients, ∼10–20% of patient mechanically ventilated for >48 hours.1,5
• The rise in hospital-associated infections due to antibiotic-resistant bacteria has resulted from the increasingly recognized administration of inadequate antimicrobial regimens.
• Inadequate initial antibiotic treatment of HCAP/HAP/VAP increases the risk of hospital mortality and may also predispose to the emergence of antibiotic-resistant bacteria.6
• Patients with HAP and HCAP have mortality rates of 15–20%, which is significantly worse than patients with community-acquired pneumonia (CAP).7
• VAP appears to be an independent determinant of mortality in critically ill patients requiring mechanical ventilation, and mortality rates range from 25–50% in different series.8 However, patients who develop VAP have a higher severity of illness and have longer ICU and hospital stays. In an analysis of 4479 patients from a multicenter database, using a model taking into account severity of illness and other confounding factors, the 30-day attributable mortality for VAP was 4.4%.9 A meta-analysis found the overall attributable mortality of VAP to be 13%.10
• More importantly, emerging clinical data suggest that the application of new management strategies for the prevention and treatment of VAP could result in improved patient outcomes.
Etiology
• Infectious organisms that commonly result in HCAP/HAP/VAP are generally different from those that are most commonly associated with CAP.
• HAP can be divided into early- or late-onset infections and more or less likely to be associated with drug-resistant organisms.
• Early-onset HAP occurs between days 2 and 4 of hospitalization.
 These infections are usually due to common community-acquired pathogens such as Streptococcus pneumoniae, methicillin-sensitive Staphylococcus aureus, and Haemophilus influenzae.
These infections are usually due to common community-acquired pathogens such as Streptococcus pneumoniae, methicillin-sensitive Staphylococcus aureus, and Haemophilus influenzae.
 Specific risk factors have been associated with certain pathogens. Aspiration has been associated with mouth anaerobes, gram-negative enteric bacilli, and S. aureus.
Specific risk factors have been associated with certain pathogens. Aspiration has been associated with mouth anaerobes, gram-negative enteric bacilli, and S. aureus.
• Late-onset HAP occurs after 4 days of hospitalization. It is associated with more virulent organisms such as methicillin-resistant S. aureus, Pseudomonas aeruginosa, and Acinetobacter species.
• In certain areas of the world, antimicrobial resistance is common and increasing. In one large, international study of HAP and VAP, multidrug resistance rates for Acinetobacter species and P. aeruginosa were 82.0% and 42.8%, respectively. Extensively drug-resistance rates were 51.1% and 4.9%.11
• Patients with HCAP may be at risk for infection with the same organisms that are responsible for late-onset HAP.
Pathophysiology
• The pathogenesis of HAP and VAP is linked to two separate but related processes:
 Colonization of the aerodigestive tract with pathogenic organisms
Colonization of the aerodigestive tract with pathogenic organisms
 Aspiration of contaminated secretions
Aspiration of contaminated secretions
• The most common sources of pathogens are1
 Microaspiration of oropharyngeal secretions
Microaspiration of oropharyngeal secretions
 Aspiration of esophageal/gastric contents
Aspiration of esophageal/gastric contents
 Inhalation of infected aerosols
Inhalation of infected aerosols
 Hematogenous spread from distant infection
Hematogenous spread from distant infection
 Exogenous penetration from the pleural space
Exogenous penetration from the pleural space
 Direct inoculation (e.g., resulting from intubation)
Direct inoculation (e.g., resulting from intubation)
• Bacterial colonization of the oropharynx is universal and S. pneumoniae, various anaerobes, and, occasionally, H. influenzae are found in the oropharynx of normal subjects.
• However, colonization with gram-negative bacilli, notably virulent organisms such as P. aeruginosa and Acinetobacter species, is rare in healthy individuals.
• It is known that oropharyngeal and tracheal colonization with P. aeruginosa and enteric gram-negative bacilli increases with length of hospital stay and with severity of illness.
• Aspiration of oropharyngeal secretions is not uncommon, even in healthy individuals. In one study, ∼45% of healthy subjects were shown to aspirate during sleep.12 However, the rate of aspiration is higher in patients with impaired levels of consciousness and inability to adequately protect their airway.
• Factors promoting aspiration include
 Abnormal swallowing for any reason
Abnormal swallowing for any reason
 Reduced levels of consciousness
Reduced levels of consciousness
 Blunted gag reflex
Blunted gag reflex
 Delayed gastric emptying
Delayed gastric emptying
 Decreased gastrointestinal (GI) motility
Decreased gastrointestinal (GI) motility
 Supine position
Supine position
• Reflux and aspiration of nonsterile gastric contents (especially when antacids are used) is also a possible mechanism of pathogen entry into the lungs, although its role is generally less significant than that of oropharyngeal microbial colonization.13,14
• The stomach has been implicated, particularly in late-onset VAP, as a potential reservoir for the aspiration of contaminated secretions.15
TABLE 13-1 RISK FACTORS FOR NOSOCOMIAL PNEUMONIA
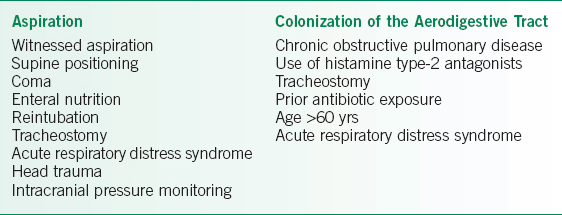
Risk Factors
• A number of risk factors for the development of HCAP/HAP/VAP have been described.
• These risk factors generally promote either aspiration or colonization of the aerodigestive tract with pathogenic bacteria (see Table 13-1).16
Prevention
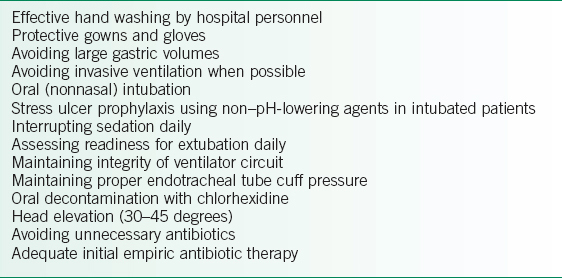
A number of pharmacologic and nonpharmacologic interventions have been studied as modalities to minimize HAP and VAP. The strategies with best clinical evidence include those in Table 13-2.1,17–21
TABLE 13-2 STRATEGIES FOR PREVENTING HOSPITAL-VENTILATOR-ASSOCIATED PNEUMONIA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


