Honeycombing
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Usual Interstitial Pneumonia (UIP)
Nonspecific Interstitial Pneumonia (NSIP)
Chronic Hypersensitivity Pneumonitis
Less Common
Sarcoidosis
Asbestosis
Rare but Important
Acute Interstitial Pneumonia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Honeycombing represents end-stage lung fibrosis
As final common pathway, can be difficult to distinguish inciting cause
Honeycombing seen on CT (macroscopic) does not always correlate with microscopic honeycombing seen on histology
Poor prognostic indicator
Characterized on imaging by
Clustered cysts with well-defined walls
3-10 mm in diameter (up to 2.5 cm), similar size
Frequently form stacked rows in peripheral lung
Cystic spaces on occasion can become large
Honeycombing always associated with other findings of lung fibrosis
Helpful Clues for Common Diagnoses
Usual Interstitial Pneumonia (UIP)
Histologic pattern of interstitial fibrosis characterized by
Temporal and spatial heterogeneity
Patchy distribution
Subpleural and basal predominance
Fibroblastic foci
Most patients with histologic and CT pattern of UIP have idiopathic pulmonary fibrosis (IPF)
Other causes of UIP pattern
Collagen-vascular disease, especially rheumatoid arthritis
Drug toxicity
Asbestosis
Hypersensitivity pneumonitis
Familial fibrosis
Inflammatory bowel disease (rare)
Most common cause of honeycombing
Early honeycombing forms in subpleural lung
Basal predominance
Clusters and rows of honeycomb cysts
Other associated features of lung fibrosis
Reticulation
Traction bronchiectasis and bronchiolectasis
Architectural distortion
Ground-glass opacity less than extent of reticular abnormality
Nonspecific Interstitial Pneumonia (NSIP)
Histological pattern of interstitial fibrosis characterized by
Spatial and temporal homogeneity
Basal predominant
Cellular, mixed, and fibrotic forms
Most patients have collagen vascular disease (especially scleroderma, mixed connective tissue disease, and polymyositis) or hypersensitivity pneumonitis
Other causes of NSIP pattern
Idiopathic (young women of east Asian ethnicity)
Drug toxicity
Familial fibrosis
Cigarette smoking (rare cause)
Honeycombing on CT is a late finding; less common with NSIP than UIP
Associated features
Basal predominant ground-glass opacity (most common)
Superimposed reticulation
Traction bronchiectasis and bronchiolectasis
Subpleural sparing (suggestive of diagnosis)
Peripheral and peribronchovascular distribution
Esophageal dilation (scleroderma and mixed connective tissue disease)
Chronic Hypersensitivity Pneumonitis
Lung fibrosis resulting from chronic hypersensitivity reaction to organic antigen or low-molecular-weight inorganic compounds
Mold and avian antigens most common causes
Inorganic compounds include isocyanates (industrial paints)
Honeycombing infrequent
Associated features
Peripheral and peribronchial reticulation
Traction bronchiectasis and bronchiolectasis
Architectural distortion
Patchy ground-glass opacity
Lobular foci of air-trapping (very suggestive of diagnosis)
Poorly defined centrilobular nodules (very suggestive of diagnosis)
Extreme lung bases typically spared in contrast to idiopathic pulmonary fibrosis
Helpful Clues for Less Common Diagnoses
Sarcoidosis
Honeycombing less common in sarcoidosis than with other end-stage lung diseases
Honeycomb cysts typically larger than those occurring with usual interstitial pneumonia
Subpleural and MID and UPPER lung zone distribution with basal sparing
Lymphadenopathy uncommon with end-stage sarcoidosis
Asbestosis
Interstitial fibrosis from asbestos exposure
Histologically similar to UIP
Subpleural branching opacities (fibrosis centered on respiratory bronchioles where asbestos fibers deposited) earliest finding on CT
Honeycombing less common unless disease severe
Associated features
Parenchymal bands and subpleural curvilinear opacities
Calcified or noncalcified pleural plaques
Subpleural reticulation
Traction bronchiectasis and bronchiolectasis
Architectural distortion
Helpful Clues for Rare Diagnoses
Acute Interstitial Pneumonia
Acute, rapidly evolving illness with respiratory failure requiring ventilatory support
50% mortality rate
Idiopathic acute respiratory distress syndrome (ARDS)
Characterized histologically by diffuse alveolar damage
Predominant radiographic features
Consolidation (basal and posterior lungs)
Ground-glass opacity (superior and anterior lungs)
Honeycombing late finding in survivors
More common in anterior lung due to barotrauma (overinflating nondependent alveoli)
Image Gallery
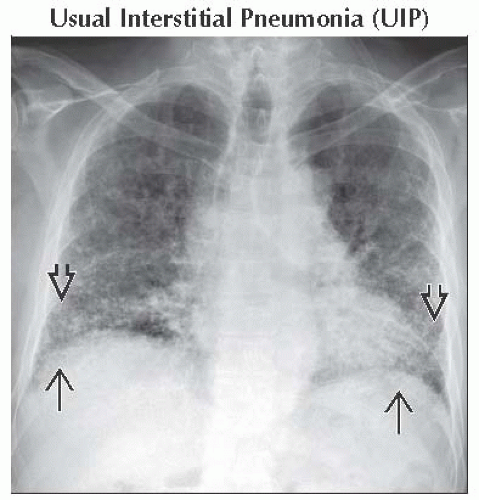 Frontal radiograph shows thin-walled honeycomb cysts in the lung bases
 with subpleural reticulation with subpleural reticulation  . Honeycombing is only apparent on chest radiographs when it is advanced. . Honeycombing is only apparent on chest radiographs when it is advanced.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|