15 History of Coronary Balloon Angioplasty and Current Indications
 Historical Overview of Cardiac Catheterization
Historical Overview of Cardiac Catheterization
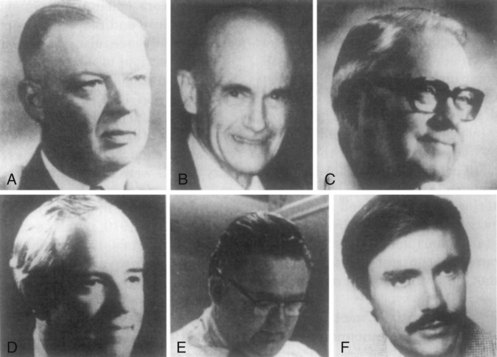
Human beings have been affected by the stenosis of luminal conduits across the body throughout history; its treatment has been influenced by the technologies available at specific historical periods (Table 15-1). Interventions that were performed to improve urinary flow by dilating the urethra were recorded by the Egyptians 3000 B.C., using bronze, gold, and silver pipes. Much later, the vascular system was instrumented in cadavers. Around 400 B.C., air and water were pushed through hollow reeds or brass pipes into cadaver aortas to clarify the function of the cardiac valves. In 1651, Harvey catheterized the inferior vena cava in a cadaver, proving that venous blood flows from the periphery to the lungs.2 In 1844, Claude Bernard, a French physiologist, inserted a mercury thermometer into the carotid artery of a horse and advanced it through the aortic valve into the left ventricle in order to measure blood temperature. Bernard called the procedure cardiac catheterization and continued to perform and improve it over the next four decades, measuring intracardiac pressures in a variety of animals and gaining essential insight on the hemodynamics of the cardiovascular system. Another milestone was passed by Adolph Fick, a German physiologist, in 1870, who estimated cardiac output through oximetric measurements and developed the appropriate calculations. In 1895, Wilhelm Conrad Roentgen discovered x-rays, allowing for the subsequent deeper visualization of the body and blood vessels. Later, in 1901, Roentgen was awarded the first Nobel Prize in physics. In 1929, Werner Forssmann was seeking a “safer approach for intracardiac drug injection”; he inserted a catheter into his left basilic vein and advanced it to the right atrium, the first documented catheter placement inside the heart of a living human being. Subsequently, in 1941, Cournand and Richards used the cardiac catheter already described initially by Forssmann and the three of them shared the 1956 Nobel Prize in medicine for development of cardiac catheterization.3 In the 1950s and ‘60s, Sones, Ricketts, Abrams, and Judkins developed coronary arteriography, allowing further understanding of the anatomy, physiology, and clinical implications of coronary artery disease.4 That paved the way for the development of coronary artery bypass grafting in the late 1960s by Kolessov, Green, and Favaloro. It is important to remember that coronary angiography also helped to correlate the clinical symptoms of angina with different degrees of luminal stenosis. In the early 1960s, Charles Dotter and Melvin Judkins, in Portland, Oregon, developed transluminal coronary angioplasty using a wire and coaxial Teflon catheters to “unclog arteries, improving symptoms and peripheral blood flow.”5 Unfortunately Dotter failed to receive support in the United States and was not able to develop the technique further. In the meantime, several investigators and researchers in Europe, especially Zeitler, gained experience in the Dotter technique. In 1974, Andreas Grüntzig, a young German physician, who had trained with Eberhardt Zeitler, modified Dotter’s catheter system (Fig. 15-1). Grüntzig developed a double-lumen catheter at the distal end of which was a distensible balloon made of polyvinylchloride (PVC). When inflated, the balloon exerted circumferential pressure on the plaque. Grüntzig achieved 86% patency in the iliac and femoropopliteal arteries and a 3-year patency rate of 73%.6
Table 15-1 Historical Evolution of Catheterization and Interventions
 Mechanisms
Mechanisms
The basic principles of percutaneous transluminal coronary angioplasty (PTCA) are extensions of Laplace’s law. The inflation of the balloon creates a “dilating force” that is a consequence of the diameter and length of the balloon; the resulting pressure and dilating force influence the “hoop stress” (Figure 15-2). When properly inflated, the balloon creates contained barotrauma that produces intimal damage, with fissuring or disruption of the plaque, usually more marked at the plaque shoulder; partial dehiscence of the intimal plaque from its underlying media; occasional intramedial dissection; stretching of the media and adventitia; and aneurismal dilatation of the vessel (Table 15-2).7,8 However, PTCA can induce acute coronary occlusion due to dissection (Fig. 15-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree