, Douglas E. Drachman2, Douglas E. Drachman3 and Douglas E. Drachman4
(1)
Harvard Medical School Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2)
Harvard Medical School, Boston, USA
(3)
Interventional Cardiology, Boston, USA
(4)
Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
Abstract
With technological advances in laboratory testing, imaging studies, and invasive procedures in cardiology, it is easy to discount the relevance of the history and physical examination. It is precisely the astute performance of the focused history and physical examination, however, that informs appropriate and efficient diagnostic testing. In the current climate emphasizing cost-effective practice, the strategic and parsimonious use of diagnostic testing is of paramount importance. Moreover, the determination of pretest probability—based on history and physical examination findings—may enhance the accuracy and clinical interpretation of subsequent diagnostic findings. In this manner, the classic teachings of the history and physical examination, coupled with the advanced capabilities of contemporary diagnostic technology, may provide optimal insight into the care of the patient.
Abbreviations
ABI
Ankle/brachial index
ACS
Acute coronary syndrome
AR
Aortic regurgitation
AS
Aortic stenosis
ASD
Atrial septal defect
AV
Aortic valve
BB
Beta blocker
BNP
B-type natriuretic peptide
BP
Blood pressure
CAD
Coronary artery disease
CI
Confidence interval
CMP
Cardiomyopathy
CP
Chest pain
CXR
Chest x-ray
DCM
Dilated cardiomyopathy
DM
Diabetes mellitus
ECG
Electrocardiogram
EP
Electrophysiology
HCM
Hypertrophic cardiomyopathy
HF
Heart failure
HR
Heart rate
HTN
Hypertension
JVD
Jugular venous distension
JVP
Jugular venous pressure
LA
Left atrium
LBBB
Left bundle branch block
LLSB
Left lower sternal border
LR
Likelihood ratio
LV
Left ventricle
LVEDP
Left ventricular end diastolic pressure
LVEF
Left ventricular ejection fraction
LVH
Left ventricular hypertrophy
MI
Myocardial infarction
MR
Mitral regurgitation
MS
Mitral stenosis
MV
Mitral valve
MVP
Mitral valve prolapse
OS
Opening snap
PCWP
Pulmonary capillary wedge pressure
PDA
Patent ductus arteriosus
PH
Pulmonary hypertension
PMI
Point of maximal impulse
PND
Paroxysmal nocturnal dyspnea
PR
Pulmonic regurgitation
PS
Pulmonic stenosis
PV
Pulmonic valve
PVD
Peripheral vascular disease
RA
Right atrium
RBBB
Right bundle branch block
RV
Right ventricle
RVH
Right ventricular hypertrophy
SOB
Shortness of breath
TR
Tricuspid regurgitation
TS
Tricuspid stenosis
TV
Tricuspid valve
VSD
Ventricular septal defect
Introduction
With technological advances in laboratory testing, imaging studies, and invasive procedures in cardiology, it is easy to discount the relevance of the history and physical examination. It is precisely the astute performance of the focused history and physical examination, however, that informs appropriate and efficient diagnostic testing. In the current climate emphasizing cost-effective practice, the strategic and parsimonious use of diagnostic testing is of paramount importance. Moreover, the determination of pretest probability—based on history and physical examination findings—may enhance the accuracy and clinical interpretation of subsequent diagnostic findings. In this manner, the classic teachings of the history and physical examination, coupled with the advanced capabilities of contemporary diagnostic technology, may provide optimal insight into the care of the patient.
History
General History
General history is comprised of the following (from the patient or the family).
Chief complaint
Common presenting symptoms for patients with suspected or known cardiovascular disease: chest pain (CP) or discomfort, shortness of breath (SOB) or dyspnea, edema, palpitations, dizziness, syncope, and fatigue or weakness.
Asymptomatic patients with incidental findings on physical examination, electrocardiogram (ECG), chest x-ray (CXR) or other imaging modalities
Asymptomatic patients who require pre-operative evaluation.
Sudden cardiac death.
Similar symptoms may stem from different underlying cardiovascular disorders and paying attention to history and examination findings will reveal clues to diagnosis.
History of the presenting illness
Description, location, onset, radiation, precipitating factors, associated symptoms, duration, alleviating factors.
Semi-quantitative assessment of symptom severity may enable serial evaluations for a change in clinical status.
Recent health status, events.
Past medical history
Known cardiac disorders
Known vascular disorders such as peripheral vascular disease (PVD) or stroke
Relevant risk factors for cardiovascular disease such as hypertension (HTN), hypercholesterolemia, metabolic syndrome, diabetes mellitus (DM), smoking status, obesity, exercise
Others: sleep apnea, chest surgery or radiation, mental stress.
Baseline functional capacity assessment is very important; a sedentary patient may never experience exertion-associated symptoms. Exercise capacity also has important prognostic implications [1]. Despite limitations, frequently used classification systems include the New York Heart Association classification, Canadian Cardiovascular Society classification and Specific Activity Scale [2].
Previous cardiovascular test results
ECG, echocardiogram, CXR, noninvasive imaging, stress test, catheterization, electrophysiologic (EP) evaluation.
Medications
Cardiac medications and compliance
Relevant non-cardiac medications with implications for diagnosis and management of the cardiovascular disease, such as: phosphodiesterase inhibitors taken for erectile dysfunction; anticoagulation for venous thromboembolism; metformin in patients exposed to iodinated contrast from cardiac catheterization
Allergies
Drug and contrast allergies and reaction should be documented.
Family history
Premature coronary artery disease (CAD), history of hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM) or sudden cardiac death.
Social history
Cocaine and alcohol intake, smoking status, job, family or home situation.
Review of systems
Neurologic, pulmonary, gastrointestinal, urinary, infectious, hematologic, immunologic, musculoskeletal, endocrine and psychiatric systems should be reviewed (Table 1-1).
Common Chief Complaints
Chest discomfort or pain (Table 1-2)
Classic angina [3]: exertional or stress-related, substernal discomfort, resolves with rest or nitroglycerin; response to nitroglycerin in the emergency department is not predictive of cardiac etiology [4] (Table 1-3).
CP equivalents: Presenting symptoms in a retrospective study of 721 patients with acute myocardial infarction presenting to the emergency department [5]
Chest, left arm, jaw, or neck complaint (53 %), SOB (17 %), cardiac arrest (7 %), dizziness/weakness/syncope (4 %), abdominal complaints (2 %), miscellaneous (trauma, gastrointestinal bleeding, altered mental status, nausea/vomiting, palpitations, and other) (17 %)
Pericarditis: abrupt onset, sharp, pleuritic and positional (better with sitting forward and worse with lying down), radiating to the back, recent fever or viral illness
Look for evidence of associated pericardial effusion (muffled or distant heart sounds) and tamponade (distant heart sounds, hypotension, jugular venous distension (JVD), dyspnea, tachycardia, pulsus paradoxus) [8]
Think constrictive pericarditis if a history of chest radiation, cardiac or mediastinal surgery, chronic tuberculosis or malignancy and right-sided heart failure (HF) symptoms/signs.
Aortic dissection: Having (1) sudden, severe, tearing CP (or equivalent), maximal at onset with radiation to the back, (2) Unequal arm blood pressure (BP) >20 mmHg and (3) Wide mediastinum on CXR had a positive likelihood ratio of 66.0 (CI 4.1–1062.0) [9]
Look for neurologic deficits, aortic regurgitation (AR), history of HTN, bicuspid aortic valve (AV), coarctation of the aorta, Marfan’s syndrome, Ehlers-Danlos syndrome, Turner syndrome, giant cell arteritis, third-trimester pregnancy, cocaine abuse, trauma, intra-aortic catheterization, history of cardiac surgery
Table 1-2
Life-threatening causes of chest pain
Cardiac
Non-cardiac
Acute coronary syndrome substernal, radiating to arm, dyspnea on exertion, diaphoresis, worse with exertion
Acute pulmonary embolism sudden onset, pleuritic, dyspnea, tachycardia, tachypnea, hypoxia, evidence of lower extremity deep venous thrombosis
Aortic dissection sudden onset, severe, tearing, radiating to the back (associated with neurologic deficits, AR), unequal arm BP >20 mmHg, wide mediastinum
Tension pneumothorax sudden onset, sharp, pleuritic, decreased breath sounds and chest excursion, hyperresonant percussion, hypoxia
Acute pericarditis & tamponade sudden onset, pleuritic, better with sitting forward, radiating to the back, pericardial rub, ± tamponade (distant heart sounds, hypotension, JVD)
Esophageal rupture/perforation severe, increase with swallowing, fever, abdominal pain, history of endoscopy, foreign body ingestion, trauma, vomiting
Table 1-1
Major causes of chest pain
Cardiac: ACS, aortic dissection, valvular heart disease, HF, myocarditis, pericarditis, variant angina, syndrome X, cocaine abuse, stress-induced cardiomyopathy
Pulmonary: PE, pleuritis/serositis, pneumonia, pneumothorax, reactive air way disease, PH and cor pulmonale, lung malignancy, sarcoidosis, pleural effusion
Gastrointestinal: GERD, esophageal spasm, esophageal tear or rupture, mediastinitis, esophagitis, peptic ulcer disease, cholecystitis, biliary colic, pancreatitis, kidney stones
Musculoskeletal: Costochondritis, spinal disease, fracture, muscle strain, herpes zoster
Psychogenic: anxiety, panic disorder, depression, hypochondriasis
Increase the likelihood
LR (95 % CI)
Decrease the likelihood
LR (95 % CI)
Radiates to the right arm or shoulder
4.7 (1.9–12)
Pleuritic
0.2 (0.1–0.3)
Radiates to both arms or shoulders
4.1 (2.5–6.5)
Sharp
0.3 (0.2–0.5)
Precipitated by exertion
2.4 (1.5–3.8)
Positional
0.3 (0.2–0.5)
Radiates to the left arm
2.3 (1.7–3.1)
Reproducible with palpation
0.3 (0.2–0.4)
Associated with diaphoresis
2.0 (1.9–2.2)
Palpitations [11]
Often described as flutters, heart skipping, pounding sensation
A history of cardiac disease increases the likelihood for cardiac arrhythmia (Likelihood ratio [LR] 2.0, 95 % confidence interval [CI] [1.3–3.1])
Palpitation associated with a regular, rapid-pounding sensation in the neck was strongly predictive in one study of atrioventricular nodal re-entry tachycardia with a LR of 177, 95 % CI (25–1,251)
Dyspnea
Differential diagnosis includes cardiac, pulmonary, neuromuscular, obesity, deconditioning, anemia and psychiatric.
Cardiac causes can be divided into the following
Heart failure (may be due to a variety of causes including valvular disease, arrhythmia, etc.):
Lack of adequate forward flow (fatigue, weakness, exercise intolerance)
Increased systemic venous or pulmonary pressures or congestion (dyspnea, orthopnea, paroxysmal nocturnal dyspnea [PND], abdominal discomfort from hepatic congestion or ascites, edema).
Acute HF tends to present with dyspnea while chronic HF tends to present with edema, fatigue, anorexia.
Myocardial ischemia: typically presents as dyspnea on exertion. Caused by acute coronary syndrome (ACS) or demand supply mismatch (left ventricular hypertrophy [LVH], HCM, valvular disease, bradycardia or tachycardia)
Pericardial disease: mainly due to increased pulmonary pressures
Claudication [12, 13]
Types of claudication:
Classic: exertional calf pain that resolves with 10 min of rest causes the patient to stop walking.
Atypical: non-calf pain, does not resolve with rest, does not keep the patient from walking, rest as well as exertional leg pain (concurrent DM, neuropathy, spinal stenosis)
Differential diagnosis of arm or leg pain
PVD: claudication associated with edema and skin discoloration
Other arterial disease: aneurysm, dissection, injury, trauma, radiation therapy, vasculitis, ergot use, artery entrapment/kinking (cyclists)
Deep vein thrombosis: associated with unilateral edema, pain worse with dependency
Musculoskeletal disorders: arthritis
Peripheral neuropathy: radiation of pain, sharp pain, back pain
Spinal stenosis: muscular weakness, worse after standing for a long time, back pain
In PVD, the location of the pain depends on the level of arterial narrowing (Table 1-4)
Table 1-4
Location of the arterial stenosis and the pain
Pain
Buttock or hip
Thigh
Upper 2/3 of the calf
Lower 1/3 of the calf
Foot
Location
Aortoiliac
Aortoiliac or common femoral
Superficial femoral
Popliteal
Tibial or peroneal
In new outpatients patients diagnosed with PVD 47 % did not have claudication, 47 % had atypical claudication and only 6 % had classic claudication [13].
Functional and exercise capacity determination is paramount as a patient may not have any symptoms if sedentary.
Physical Examination
General Examination
Vital signs
Any abnormality in BP, heart rate (HR), respiratory rate and oxygenation should be explored.
Blood pressure
Significant difference in pulses and BP in arms: >20 mmHg in BP is associated with aortic coarctation or dissection, subclavian artery disease, supravalvular (right > left in BP) and aortic stenosis (AS)
Significant difference in the pressure in legs compared with arms: >20 mmHg higher than arms is associated with the Hill sign in severe AR or extensive and calcified lower extremity peripheral arterial disease. A delay in pulse from radial to femoral in a patient with HTN is associated with aortic coarctation
Pulse pressure is defined as systolic pressure – diastolic pressure
Wide pulse pressure is associated with AR, older age, atherosclerosis
Narrow pulse pressure is associated with HF (a pulse pressure of <25 % of the systolic pressure is associated with a cardiac index of <2.2 L/min/m2) [14], HCM
Orthostatic blood pressures: measure BP and HR after standing for 1–3 min.
Orthostatic hypotension: a drop in systolic BP >20 mmHg, a drop in diastolic BP >10 mmHg or HR rise >10 bpm.
Valsalva response
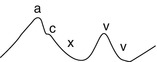
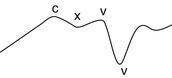
Normal Valsalva sinusoidal response (Fig. 1-1)
Figure 1-1
Normal valsalva sinusoidal response. BP blood pressure (Courtesy of Dr. Hanna Gaggin)
Abnormal response pattern (in patients not taking a beta blocker [BB])
Absent overshoot response: no Phase 4 rise in systolic BP, associated with moderately decreased left ventricular ejection fraction (LVEF)
Square wave response: presence of Korotkoff sounds during the entire straining phase and no Phase 4 rise in systolic BP, associated with severely decreased LVEF
Pulsus paradoxus
Fall in systolic BP >12 mmHg with inspiration has a sensitivity of 98 % and specificity of 83 % for the diagnosis of pericardial tamponade [8]
Can also be positive in hypovolemia, anything that results in right-sided failure (pulmonary embolism, chronic lung disease), constriction, HF
General appearance
The first assessment before any history or physical examination should be the global overview. Is the patient acutely ill? Diaphoresis, tachypnea, cyanosis, decreased mental status all signify serious conditions. The result of this assessment will determine how focused and timely the history and examination should be.
The skin
Identify evidence of poor perfusion such as cold and clammy skin (cardiogenic shock, HF or PVD), cyanosis (congenital heart disease or shunts), bronzing of the skin (iron overload or hemochromatosis), ecchymoses (antiplatelet or anticoagulation medication), xanthomas (hypercholesterolemia), lupus pernio, erythema nodosum or granuloma annulare (sarcoidosis).
Look for dialysis fistulas (end stage renal disease and in acutely ill patients, likely metabolic disarray).
Skin findings that increase the likelihood of PVD [15]
Cool to touch LR 5.9 (95 % CI 4.1–8.6)
Wounds or sores LR 5.9 (95 % CI 2.6–13.4)
Skin discolorations LR 2.8 (95 % CI 2.4–3.3)
Head and neck
Elevated jugular venous pressure (HF), high arched palate (Marfan’s), large protruding tongue (amyoloidosis), ptosis and ophthalmoplegia (muscular dystrophies), hypertelorism, low-set ears, micrognathia, webbed neck (Noonan, Turner and Down syndromes), proptosis, lid lag and stare (Grave’s hyperthyroidism).
Jugular venous pressure (Table 1-5)
Calculation of jugular venous pressure (JVP) in mmHg
1.
Determine vertical distance above the sternal angle to the top of the venous pulsation (in cm water)
3.
Divide by 1.36
Normal RA pressure is <8 mmHg
Clinical assessment of the presence of an elevated JVP (rather than exact JVP) is fairly accurate in predicting elevated right atrial (RA) pressure and the pulmonary capillary wedge pressure (PCWP)
JVP <11 cm in predicting invasively measured RA pressure <8 mmHg: negative predictive value =82 % [17]
Presence of elevated JVP at rest or hepatojugular reflux in predicting PCWP >18 mmHg: sensitivity =81 %, specificity =80 %, predictive accuracy =81 % (in the absence of cirrhosis, volume overload in renal diseases and right-sided cardiac disease) [18]
When three or more signs (JVD, S3, tachycardia, low pulse pressure, rales, abdominojugular reflux), >90 % likelihood of increased filling pressures if severe left ventricular (LV) dysfunction was not known. 1 or 0 symptoms or signs <10 % likelihood of increased filling pressures [19]. In chronic HF, rales, edema, JVD and pulmonary edema on CXR can be often absent.
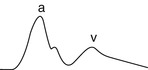
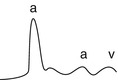
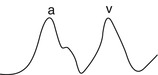
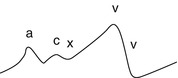
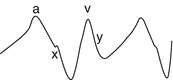
Table 1-5
Jugular venous waveforms
Finding and RA tracing
Examples
Normal
Prominent a wave
Obstruction to RA emptying
TV abnormalities: TS, RA myxoma, carcinoid heart disease, lupus endocarditis, RA thrombus, tricuspid atresia
Distal to tricuspid valve: decreased RV compliance such as in RVH, RV outflow obstruction such as in PS
PH
Uncommon in conditions with VSD or ASD
Cannon a wave
RA contraction against a closed TV
A-V dissociation
Premature atrial, junctional or ventricular beats
1st degree AVB
Flutter a wave
Atrial flutter
Absent a wave
No effective atrial contraction
Atrial fibrillation
Ebstein’s anomaly
Equal a wave and v wave
ASD
TR
Prominent v wave
ASD without PH
Prominent × descent
ASD
Early cardiac tamponade
Blunted or absent y descent

Late pericardial tamponade
TS
Severe RVH
Steep y descent

Constrictive pericarditis (classic M or W contour with prominent x and y descents)
Restrictive cardiomyopathy
Severe right side HF
TR
Chest
Look for venous collaterals (venous obstruction), pectus carinaturm or excavatum (connective tissue disorders), barrel chest (emphysema), kyphosis (ankylosing spondylitis)
Abdomen
Hepatomegaly and ascites (right-sided HF, constrictive pericarditis), enlarged abdominal aorta (the positive predictive value for abdominal aortic aneurysm is only 43 % [20])< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


