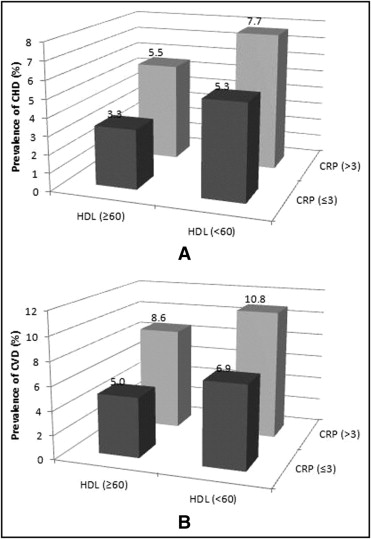
High-density lipoprotein (HDL) cholesterol is inversely associated with the risk of cardiovascular disease (CVD). However, whether the protective effect of HDL becomes impaired by elevated high-sensitivity C-reactive protein (hs-CRP) is not well-established. We evaluated 13,572 United States adults aged ≥18 years who participated in the cross-sectional National Health and Nutrition Examination Survey 1999–2008. The subjects were classified according to the recognized cutpoints of HDL cholesterol elevations of ≥60 mg/dl, hs-CRP of >3 mg/L, and by a history of self-reported coronary heart disease (CHD) or CVD. Multivariate logistic regression analysis was used to assess the odds of prevalent CHD and CVD according to HDL cholesterol/hs-CRP group, after adjusting for known risk factors. Those with HDL cholesterol of ≥60 mg/dl and CRP >3 mg/L versus HDL cholesterol <60 mg/dl and CRP ≤3 mg/L had as high or a greater prevalence of CHD (5.5% and 5.3%, respectively) and CVD (8.6% and 6.9%, respectively). Compared to those with HDL cholesterol of ≥60 mg/dl and CRP ≤3 mg/L, those with HDL cholesterol ≥60 mg/dl and hs-CRP >3 mg/L had a 1.38 (95% confidence interval 0.94 to 2.02) adjusted odds of CHD and 1.38 (95% confidence interval 1.00 to 1.90) adjusted odds of CVD. Those with an HDL cholesterol <60 mg/dl and CRP >3 mg/L had the greatest adjusted odds of both CHD (1.75, 95% confidence interval 1.28 to 2.38) and CVD (1.74, 95% confidence interval 1.33 to 2.28). In conclusion, an hs-CRP >3 mg/L in the presence of HDL cholesterol of ≥60 mg/dl is associated with an attenuation in the protective association of HDL cholesterol ≥60 mg/dl and CRP of ≤3 mg/L with CHD and CVD.
It is well documented that high-density lipoprotein (HDL) cholesterol is inversely related to coronary heart disease (CHD). HDL promotes reverse cholesterol transport and protects low-density lipoprotein from oxidative stress. C-reactive protein (CRP), a marker of systemic inflammation, is associated with increased CHD risk and has been shown to add to the risk conferred by low-density lipoprotein (LDL) cholesterol. The epidemiologic relation of the levels of CRP with HDL cholesterol to CHD has not been described. If an interaction exists between CRP and HDL, such that the former renders the latter dysfunctional, the protective effect of HDL on CHD risk in the presence of high CRP could be inhibited. Not established is whether elevated CRP levels might attenuate the protective relations of HDL cholesterol with CHD. We examined in a large sample of subjects representative of United Stages adults whether the relations of HDL cholesterol with CHD and cardiovascular disease (CVD) are modified by the CRP levels.
Methods
We identified 28,852 men and women aged ≥18 years (weighted to 213.2 million), who participated in the National Health and Nutrition Examination Survey 1999–2008, a complex multistage sample design of the civilian, noninstitutionalized United States population conducted by the National Center for Health Statistics. Of these, 13,572 subjects (weighted to 106.4 million) had complete medical history and risk factor information, including measurements of lipids and high-sensitivity CRP (hs-CRP) levels available for analysis.
Blood samples were collected from the mobile screening vans and processed according to standard procedures. HDL cholesterol was measured directly in serum using heparin manganese precipitation (1999–2002) and immunoassay (2003 onward). A correction formula was applied to account for the differences in these 2 methods. hs-CRP was measured quantitatively using latex-enhanced nephelometry with a Behring Nephelometer. The concentrations were calculated using a calibration curve. LDL cholesterol was calculated from the fasting measures of total cholesterol, triglycerides, and HDL cholesterol using the Friedewald formula. Diabetes mellitus was defined by a fasting glucose level of ≥6.99 mmol/L (126 mg/dl), a nonfasting glucose level of ≥11.1 mmol/L (200 mg/dl), oral hypoglycemic medication or insulin, or self-reported. The plasma glucose concentration was measured using an enzymatic reaction (Cobas Mira Chemistry System; Roche Diagnostic Systems, Montclair, New Jersey). Fasting serum triglycerides were hydrolyzed to produce glycerol and measured enzymatically on a Hitachi 704 analyzer (Boehringer Mannheim Diagnostics, Indianapolis, Indiana). The details of specimen collection and storage have been previously published.
CHD (including myocardial infarction or angina pectoris), heart failure, and stroke were identified by the participant by self-report of being told by a physician they had 1 of these conditions. CVD was defined as reporting yes to ≥1 of these CHD conditions or being told by a physician of having stroke or heart failure.
The subjects were categorized into 4 distinct groups: group 1, HDL cholesterol ≥60 mg/dl and CRP ≤3 mg/L; group 2, HDL cholesterol ≥60 mg/dl and CRP >3 mg/L; group 3, HDL cholesterol <60 mg/dl and CRP ≤3 mg/L; and group 4, HDL cholesterol <60 mg/dl and CRP >3 mg/L. The chi-square test of proportions and t tests were performed to evaluate the differences in baseline characteristics between the hs-CRP and HDL cholesterol groups and by gender and presence of CHD and CVD. Logistic regression analysis, unadjusted and adjusted, for age, gender, race, smoking status, diabetes status, systolic blood pressure, LDL cholesterol, triglycerides, hours fasting, and body mass index was performed to examine the joint relation of HDL cholesterol and hs-CRP groups with the odds of CHD and CVD. Odds ratios and 95% confidence intervals of CHD and CVD were calculated, using group 1 (HDL cholesterol ≥60 mg/dl and hs-CRP ≤3 mg/L) as the referent group. The baseline characteristics were weighted to the United States population. All statistical analyses were performed using SAS, version 9.2, statistical software (SAS Institute, Cary, North Carolina) and SUDAAN, version 9.0 (Research Triangle Institute, Research Triangle Park, North Carolina).
Results
Significant differences were present in age and key risk factors between the men and women and by HDL cholesterol and hs-CRP category, and according to the presence of CHD or CVD ( Table 1 ). Those with HDL cholesterol ≥60 versus <60 mg/dl were more likely to be younger, without CHD, CVD, or diabetes, nonsmoking, with lower LDL cholesterol, body mass index, triglycerides, and hs-CRP. Those with hs-CRP >3 versus ≤3 mg/L were more likely to be older, to have CHD, CVD, diabetes, to be a smoker, and to have greater LDL cholesterol, systolic blood pressure, body mass index, triglycerides, and low HDL cholesterol. Furthermore, those with versus without CHD or CVD were more likely to be older, to have diabetes and to have a higher systolic blood pressure, body mass index, triglycerides but lower LDL cholesterol levels. In addition, the correlation of hs-CRP with HDL cholesterol was poor (−0.037) although statistically significant (p <0.001) owing to the large sample size studied.
| Gender | HDL Cholesterol (mg/dl) | hs-CRP (mg/L) | CHD | CVD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ≥60 | <60 | ≤3 | >3 | No | Yes | No | Yes | |
| Overall (n) | 6,659 | 6,913 | 4,050 | 9,522 | 8,382 | 5,190 | 12,678 | 894 | 12,307 | 1265 |
| Coronary heart disease | 6.8% | 4.3% ⁎ | 3.9% | 6.2% ⁎ | 4.7% | 7.1% ⁎ | — | — | — | — |
| Cardiovascular disease | 8.6% | 6.8% ⁎ | 6.1% | 8.4% ⁎ | 6.3% | 10.3% ⁎ | — | — | — | — |
| Smoking | 30.0% | 21.7% ⁎ | 21.5% | 27.6% ⁎ | 24.8% | 27.6% † | 25.9% | 23.9% | 25.9% | 24.6% |
| Diabetes | 7.0% | 6.8% | 4.6% | 7.8% ⁎ | 5.1% | 10.1% ⁎ | 6.0% | 22.2% ⁎ | 5.6% | 22.5% ⁎ |
| Age (years) | 44.1 | 45.7 ⁎ | 46.9 | 44.1 ⁎ | 43.5 | 47.5 ⁎ | 43.8 | 64.6 ⁎ | 43.3 | 64.0 ⁎ |
| Low-density lipoprotein cholesterol (mg/dl) | 120.5 | 118.2 ⁎ | 114.7 | 121.2 ⁎ | 117.5 | 122.7 ⁎ | 119.9 | 110.2 ⁎ | 119.8 | 113.3 ⁎ |
| Systolic blood pressure (mm Hg) | 122.9 | 120.0 † | 121.6 | 121.4 | 119.8 | 124.4 ⁎ | 120.9 | 129.8 ⁎ | 120.7 | 130.5 ⁎ |
| Body mass index (kg/m 2 ) | 28.0 | 28.2 ‡ | 25.8 | 29.0 ⁎ | 26.4 | 31.2 ⁎ | 28.0 | 29.3 ⁎ | 28.0 | 29.3 ⁎ |
| Triglycerides (mg/dl) | 127.9 | 113.8 ⁎ | 89.4 | 133.8 ⁎ | 111.7 | 137.3 ⁎ | 119.2 | 147.1 ⁎ | 118.7 | 145.2 ⁎ |
| High-sensitivity C-reactive protein (mg/L) | 3.39 | 4.95 ⁎ | 3.86 | 4.33 † | 1.19 | 9.71 ⁎ | 4.12 | 5.43 ⁎ | 4.06 | 5.70 ⁎ |
| High-density lipoprotein cholesterol (mg/dl) | 48.0 | 58.4 ⁎ | 72.6 | 45.3 ⁎ | 54.4 | 51.2 ⁎ | 53.5 | 50.0 ⁎ | 53.5 | 50.9 ⁎ |
‡ p <0.05 (compared to males, HDL ≥60 mg/dl group, hs-CRP ≤ 3 mg/L group, without CHD, and without CVD).
Figure 1 shows the unadjusted prevalence of CHD and CVD, respectively, according to HDL cholesterol and hs-CRP categories. Those with HDL cholesterol ≥60 mg/dl and hs-CRP ≤3 mg/L had the lowest prevalence of CHD (3.3%) and CVD (5.0%). Those with HDL cholesterol <60 mg/dl and hs-CRP >3 mg/L had the greatest prevalence (7.7% and 10.8%, respectively). In the presence of hs-CRP >3 mg/L, the prevalence of CHD and CVD is still increased when the HDL cholesterol was ≥60 mg/dl (5.5% and 8.6%, respectively), which for CHD was similar and for CVD was higher than that seen in those with HDL cholesterol <60 mg/dl and CRP ≤3 mg/L.