High-Attenuation Mass, Mediastinum or Hilum
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Calcified Lymphadenopathy
Histoplasmosis
Tuberculosis
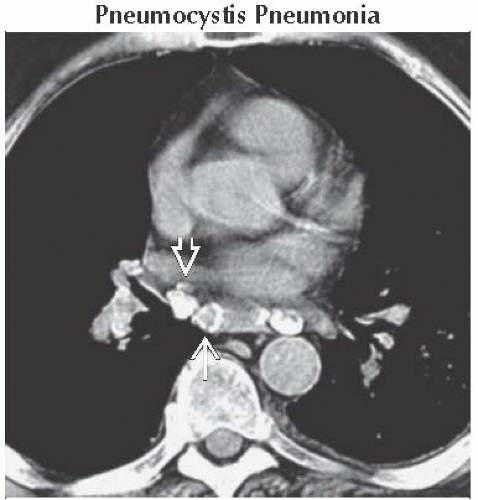
Pneumocystis Pneumonia
Mediastinal Fibrosis
Goiter
Aneurysm
Hematoma
Less Common
Silicosis/Coal Worker’s Pneumoconiosis
Neoplastic
Treated Hodgkin Lymphoma
Thymoma
Teratoma
Neuroblastoma
Castleman Disease
Metastases
Sarcoidosis
Rare but Important
Amyloidosis
Foregut Cyst
Hemangiomas
Gossypiboma
Aluminum Pneumoconiosis
Perflubron Ventilation
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Mnemonic: EGGSHELL CA+
Environmental dusts (silica, coal, aluminum)
Goiter
Gossypiboma
Sarcoidosis
Hemangioma
Ecchymosis (hematoma)
Lymphoma (treated Hodgkin)
Lymph nodes (histoplasmosis, tuberculosis, PCP)
Cancer (thymoma, teratoma, neuroblastoma, metastases, or Castleman)
Aneurysm
Helpful Clues for Common Diagnoses
Calcified Lymphadenopathy
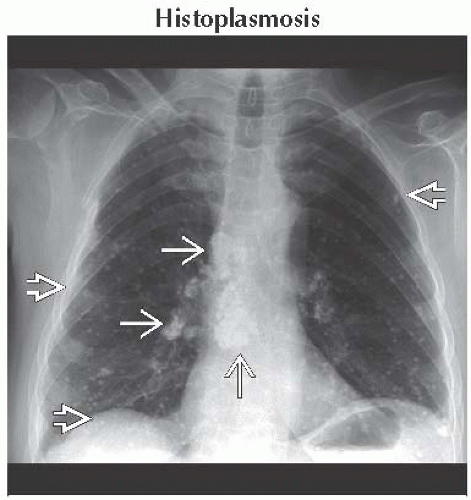
Histoplasmosis
Calcification of granuloma and nodes age and time dependent
Calcification within months in children, years in adults
Either central nidus or diffuse calcification pattern
Nodes follow drainage pattern of lung granuloma
Splenic calcification common
Multiple small pulmonary calcifications in histoplasmosis; fewer, larger pulmonary calcifications in tuberculosis
Tuberculosis
Nodal calcification often diffuse
Seen in 50%
Mediastinal Fibrosis
Focal mediastinal mass > 5 cm diameter, most common paratracheal
Central calcification in mass (90%), also seen in peripheral granuloma
Eventually obstructs superior vena cava, airways, & pulmonary veins, in that order
Goiter
Calcification: Coarse, punctate, or rings
Aneurysm
Curvilinear calcification
Due to atherosclerosis, trauma, fungal infection, cystic medial necrosis, vasculitis
Hematoma
Acute hematoma due to trauma, catheter insertion, surgery, clotting disorder, aneurysms, tumor
Consider ectopic parathyroid adenoma, which may spontaneously hemorrhage
90% of clots have ↑ attenuation over 1st 72 hours
Helpful Clues for Less Common Diagnoses
Silicosis/Coal Worker’s Pneumoconiosis
Eggshell calcification in 3-6%
Associated with interstitial lung disease
Neoplastic
Treated Hodgkin Lymphoma
Following radiation therapy, ˜ 20% of nodal masses will calcify
2 types: Eggshell or multiple discrete deposits (mulberry type)
Extremely rare (case reports) of calcification prior to treatment
Thymoma
1/3 have calcification: Thin linear in capsule, scattered punctate calcification less commonly seen
Also seen in invasive thymomas
Teratoma
a.k.a. dermoid cyst
Teratomas: 70% of germ cell tumors
Fat: 75%, fluid: 90%, calcification: 40%
Calcification may have tooth shape
Neuroblastoma
Calcification (80%): Cloud-like, stippled, ring-shaped, solid
Castleman Disease
Calcification (5-10%): Discrete, coarse, or tree-like, rarely visible on radiographs
Metastases
Usually seen in those with known disease
Osteosarcoma, mucinous colon or ovarian, papillary thyroid carcinoma most common tumors
Sarcoidosis
50% have calcification, 40% within 1 year of diagnosis
Calcification typically central: Smudgy or putty-like, may be eggshell but uncommon
Helpful Clues for Rare Diagnoses
Amyloidosis
Adenopathy, isolated or associated with interstitial lung disease (50%)
Usually multiple lymph node groups, may be massive
Calcification stippled, diffuse, or eggshell
Systemic disease common, typically Waldenström macroglobulinemia
Foregut Cyst
Bronchogenic cysts most common (50%)
Calcification either in fluid (milk of calcium: 3%), less common curvilinear in wall
Hemangiomas
Phleboliths: 10-40% (fat 40%)
Central area of decreased attenuation pathognomonic for phlebolith (in 7%)
More common: Multiple punctate round calcifications (30%)
Gossypiboma
Retained surgical sponge or swab
Spongiform low-density mass with gas bubbles
Sponges in USA contain radiopaque markers, often 1 or 2 linear wires
Calcification also deposited along network architecture of surgical sponge (“calcified reticulate rind”)
Aluminum Pneumoconiosis
Nodes with diffuse homogeneous increased attenuation (from aluminum)
Perflubron Ventilation
Used in severe respiratory failure
Contains bromine atoms, which makes agent radiopaque
May accumulate and remain long term in lymph nodes and efface mediastinal fat
Image Gallery
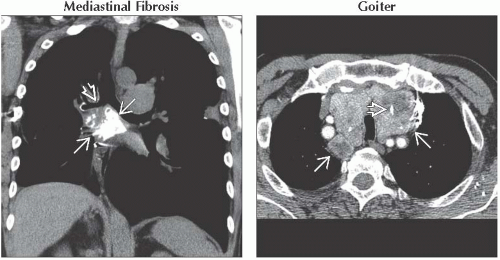 (Left) Coronal NECT reconstruction shows a large subcarinal calcified mediastinal mass
 narrowing the right main bronchus narrowing the right main bronchus  . Subcarinal location is the 2nd most common location. Typically fibrosis in this area obstructs airways or pulmonary veins. (Right) Axial CECT shows a large superior mediastinal mass . Subcarinal location is the 2nd most common location. Typically fibrosis in this area obstructs airways or pulmonary veins. (Right) Axial CECT shows a large superior mediastinal mass  compressing the trachea. Goiter is high density from iodine and foci of calcification compressing the trachea. Goiter is high density from iodine and foci of calcification  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|