Chapter 20 Hemoptysis
Differential Diagnosis
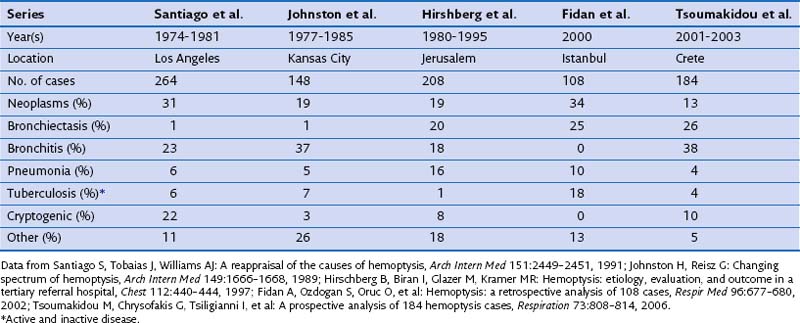
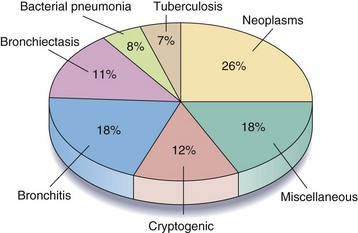
A large number of disorders have been reported to cause hemoptysis, and the most important are listed in Box 20-1. Of these, bronchogenic carcinoma, bronchiectasis, bronchitis, and bacterial pneumonia are responsible for most cases. Table 20-1 shows the relative frequency of disorders causing hemoptysis in major series published since 1980. The significant variability, especially in the frequency of bronchiectasis, bronchitis, and tuberculosis, probably reflects differences in the time of publication, the patient population studied, and the diagnostic tests and criteria used. Figure 20-1 illustrates the percentage of patients with each diagnosis on the basis of pooled data from these studies.
Box 20-1
Causes of Hemoptysis
Cryptogenic Hemoptysis
In almost all reported series, the cause of hemoptysis remains unknown in a significant percentage of patients. As shown in Table 20-1, the frequency of cryptogenic hemoptysis has varied widely, and this variability presumably is due to differences in diagnostic criteria and the extent of evaluation.
Patient Evaluation
Initial Evaluation
Important symptoms, signs, and historical details that suggest one or more disorders are listed in Table 20-2. In some patients, such as those with pulmonary embolism, left ventricular failure, mitral stenosis, and traumatic or iatrogenic lung injury, the history and physical examination may provide the most important clues to the diagnosis.
Table 20-2 Important Clinical Features in Patients with Hemoptysis
| Category |
|---|