Hemoptysis
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Bronchogenic Carcinoma
Metastases
Infection
Tuberculosis
Aspergilloma
Lung Abscess
Bronchiectasis
Bronchitis
Pulmonary Emboli
Less Common
Diffuse Alveolar Hemorrhage
Cardiac Causes
Congestive Heart Failure
Mitral Stenosis
Rare but Important
Pulmonary Artery Aneurysm
Arteriovenous Malformation (AVM)
Broncholithiasis
Pseudosequestration
Kaposi Sarcoma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Hemoptysis definition
Expectoration of blood that originates from airways or lung
Massive hemoptysis: > 300 mL in 24 hours
Majority have identifiable etiology
Cryptogenic hemoptysis 3-15%
Bronchial arteries most common source of bleeding
Bronchial artery anatomy
Orthotopic origin: Arises from descending aorta at level of 5th or 6th thoracic vertebra
CT location
Right bronchial artery at level of carina
Left bronchial artery(s) at level of proximal left main bronchus
Classic branching pattern
Type 1: 1 right intercostobronchial trunk and 2 left bronchial arteries (40%)
Type 2: 1 right intercostobronchial trunk and 1 left bronchial artery (20%)
Type 3: 1 intercostobronchial trunk, right bronchial artery, 2 left bronchial arteries (20%)
Type 4: 1 intercostobronchial trunk, right bronchial artery, 1 left bronchial artery (10%)
Ectopic origin: Bronchial arteries arise from other than expected site
Bronchial artery diameter > 2 mm abnormal
Helpful Clues for Common Diagnoses
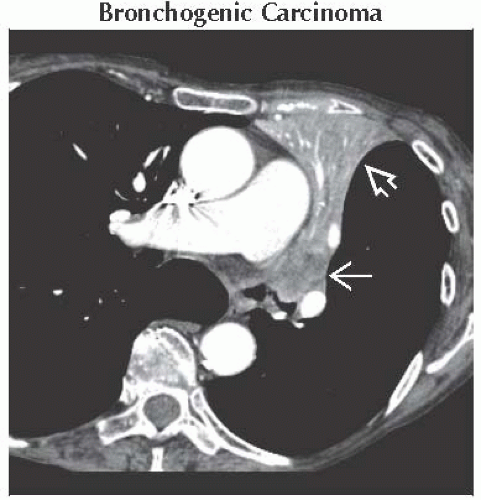
Bronchogenic Carcinoma
Hemoptysis usually seen in advanced cancers, accounts for up to 20% of cases of hemoptysis
Smokers > 40 years old with cryptogenic hemoptysis: 5% will develop lung cancer within 3 years
Carcinoid tumors
Often highly vascular, may enhance with intravenous contrast
Metastases
Hemorrhagic metastases: Commonly from choriocarcinoma, renal cell carcinoma, melanoma, thyroid
CT: Multiple variable-sized nodules surrounded by ground-glass opacities
Tuberculosis
Common cause of hemoptysis, generally seen in those with active cavitary disease
Rasmussen aneurysm: Pulmonary artery aneurysm arising adjacent to cavitary wall, hemoptysis may be massive
Aspergilloma
Saprophytic mycelia growth in preexisting cavity
Hemoptysis may be massive
Lung Abscess
Hemoptysis may be massive; foul-smelling sputum typical
Bronchiectasis
Accounts for up to 25% of hemoptysis, may be massive
Distribution clue to etiology
Central bronchiectasis: Allergic bronchopulmonary aspergillosis, tracheobronchomegaly, Williams-Campbell syndrome
Upper lobe bronchiectasis: Cystic fibrosis, tuberculosis, allergic bronchopulmonary aspergillosis
Ventral bronchiectasis: Mycobacterium avium complex
Lower lobe: Postinfectious, aspiration
Bronchitis
Accounts for 20% of cases of hemoptysis
Dieulafoy disease: Abnormal dilated submucosal vessels from chronic inflammation
CT usually normal; may have bronchial wall thickening; focal ground-glass opacities and consolidation suggest active hemorrhage
Pulmonary Emboli
Hemoptysis from pulmonary infarcts
Infarcts in < 10% of embolic episodes
Infarcts are pleural-based, wedge-shaped, with no contrast enhancement
Helpful Clues for Less Common Diagnoses
Diffuse Alveolar Hemorrhage
Inflammatory process involving blood vessels (large, medium, or small)
Spectrum includes Wegener granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome
CT: Nonspecific lobular ground-glass opacities admixed with consolidation; crazy-paving pattern more common as hemorrhage resolves
Hemoptysis in 66%
Cardiac Causes
Frothy blood sputum in congestive heart failure (accounts for 5% of cases of hemoptysis)
Patients with mitral stenosis may have repeated bouts of hemorrhage leading to hemosiderosis
Helpful Clues for Rare Diagnoses
Pulmonary Artery Aneurysm
Causes: Swan-Ganz-induced pseudoaneurysm, Behçet syndrome
Swan-Ganz pseudoaneurysm: Mortality 45-65%
Usually lower lobe segmental artery in perihilar location
Arteriovenous Malformation (AVM)
Epistaxis presenting features in hereditary hemorrhagic telangiectasis (HHT)
AVM vessels have thin walls, at risk for rupture
Rupture more common in pregnancy
Broncholithiasis
Hemoptysis in 50%
Peribronchial calcified lymph node that distorts or narrows adjacent airway
Pseudosequestration
Pure vascular pulmonary sequestration; lung and bronchi normal
Also refers to transpleural systemic-pulmonary artery anastomoses (most commonly seen with pulmonary artery stenosis)
Kaposi Sarcoma
AIDS-related multicentric neoplasm involving skin, lymph nodes, GI tract, and lungs
Diffuse peribronchial nodules emanating from hilum
Image Gallery
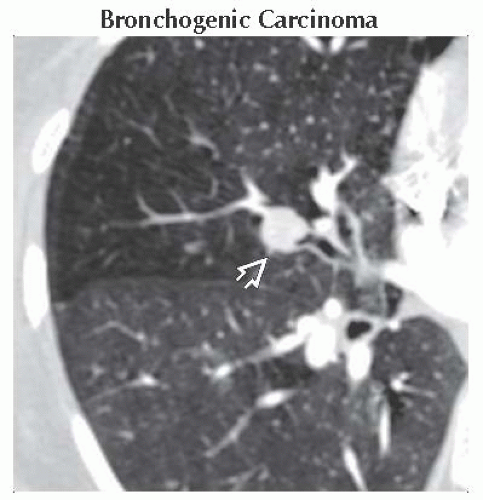 Axial CECT shows a small endobronchial carcinoid tumor
 . The tumor enhanced with contrast on mediastinal windows (not shown). . The tumor enhanced with contrast on mediastinal windows (not shown).Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|