Hemodialysis Access Catheters
Eric K. Peden
The National Kidney Foundation Dialysis Outcomes Quality Initiative Clinical Practice Guidelines for Vascular Access (DOQI) have defined the standard of care and have emphasized the importance of autogenous access. The DOQI state that <10% of all patients should be dialyzed using chronic catheters and define chronic as >3 months in the absence of an autogenous access that is maturing. Despite these recommendations, the prevalence of dialysis catheters across the United States is approximately 17% as defined by the Dialysis Outcome and Practice Patterns Study (DOPPS). The explanation for their widespread use is likely multifactorial, but foremost among these is inadequate pre-end stage renal disease care and delayed referral to a surgeon for permanent access. Indeed, the DOPPS reported that 60% of the patients in the United States started dialysis using a catheter and only approximately 50% had previously undergone placement of a permanent access. Although all dialysis catheters should be considered a temporary modality given DOQI, it is important for access surgeons to be familiar with their proper placement and care, given the limitations of pre-end stage renal disease care and their role as a “bridge” to allow autogenous accesses to mature. Indeed, patients may require the use of catheters for several months before an effective permanent access can be established.
Indications and Contraindications
The hemodialysis catheters can be broken down into two main categories: tunneled and nontunneled. The tunneled catheters have a fabric cuff that is positioned between the venous cannulation site and the catheter exit site on the skin that serves to incite tissue ingrowth. The cuff and the tunnel serve to create a barrier against infection and allow the catheters to be used for a prolonged period of time, ranging from several weeks to several months. In contrast, the nontunneled catheters are more prone to infection and are generally useable for only a couple of weeks. There are a variety of different manufacturers and available devices, although the generic design is similar. The catheter is comprised of two separate lumens with the corresponding ports separated by a few centimeters to prevent recirculation. Blood is withdrawn through the aspiration or “arterial” port and returned through the infusion or “venous” port, which is typically at the distal tip of the catheter. Notably, separate venous and arterial catheters can be used, but the underlying principle is the same.
The dialysis catheters afford many advantages. They are relatively easy to place, can be inserted in multiple different veins, and can be used immediately for dialysis. A recent survey reported that patients actually prefer catheters to prosthetic and autogenous arteriovenous accesses because they don’t need to be stuck with the large cannulation needles to be attached to the dialysis machine. The flow rates through the catheters during dialysis are fairly low and, thus, not associated with significant hemodynamic instability, although these low flow rates can translate into ineffective dialysis. The primary disadvantages of the catheters relate to their associated morbidity from thrombosis and infection. Indeed, the life expectancy is the shortest for patients that dialyze using catheters. Similar to all central vein catheters, they can lead to the development of stenoses and/or occlusions that limit future access options. Furthermore, they can be lifestylelimiting for active individuals (e.g., no swimming) and unacceptable to some patients from a cosmetic standpoint.
The DOQI recommend nontunneled catheters when it is anticipated that hemodialysis will be required for <3 weeks. Additionally, these catheters should be considered when it is not possible or not desirable to place a tunneled catheter. This commonly occurs in emergency situations when it is not safe to transport a patient to the operating room/angiography suite or when a patient is actively infected and, therefore, it is not safe to place a more permanent tunneled catheter. Given their relatively short lifespan, they should not be inserted any sooner than necessary for dialysis.
Tunneled catheters are indicated for longer-term use and can occasionally serve as the sole method of access. DOQI recommend that these catheters be placed in patients requiring hemodialysis >3 weeks, those awaiting maturation of their autogenous access, and in the subset of patients who have exhausted all other permanent access options (usually as a result of inadequate arterial inflow and/or venous outflow). Indeed, dialysis catheters provide an essential bridge to allow the autogenous accesses to mature and have facilitated meeting the DOQI autogenous targets (i.e., 50% incidence, 40% prevalence). Catheters also appear to be justified in patients with limited life expectancy and those with prohibitive comorbidities that preclude permanent access. The latter includes patients with severe congestive heart failure who cannot tolerate the increased cardiac output associated with the permanent access and those with dementia who cannot tolerate repeated needle cannulations.
Anatomic Considerations
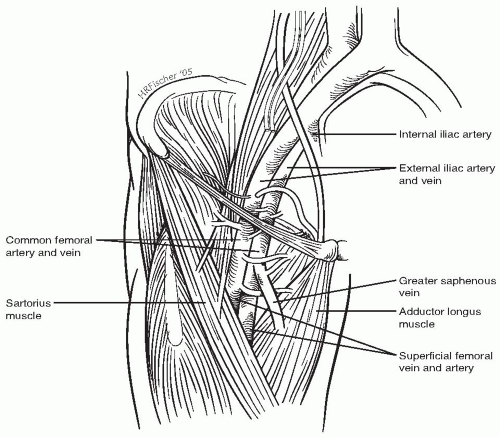
Although essentially any central vein can be used, the common femoral and the right internal jugular veins are generally preferred for the nontunneled and tunneled dialysis catheters, respectively. The superficial femoral vein courses posterolateral to its corresponding artery in the thigh, while the common femoral vein lies medial to the artery in the groin (Fig. 87-1). The common femoral vein is ideally suited for the nontunneled catheters because it courses fairly superficial and is relatively easy to cannulate. Unfortunately, common femoral vein catheters are prone to infection and developing deep venous thromboses (DVTs). The nontunneled common femoral vein catheters should not be left in place much longer than 5 days, and patients should be kept at bedrest. These nontunneled catheters should be switched to another form of access (i.e., tunneled catheter, prosthetic/autogenous arteriovenous fistula) as soon as possible.
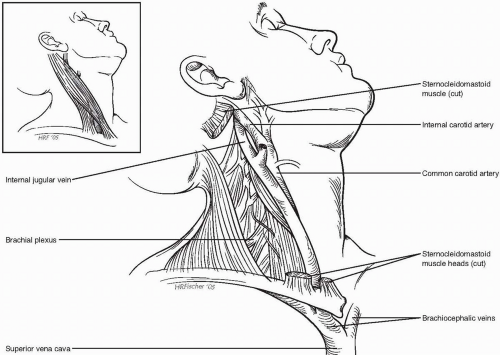
The right internal jugular vein exits the skull base at the jugular foramen, then courses inferior along the carotid and vagus nerve (Fig. 87-2). It begins posterior to the carotid at the base of the skull then spirals around anterior. At the bases of the neck, it courses between the two heads of the sternocleidomastoid muscle. It is large, fairly superficial, and follows a direct course to the superior vena cava. Because of its anatomic distance from the pleura of the lung, the incidence of causing a pneumothorax at the time of internal jugular vein cannulation is less than associated with subclavian vein cannulation. Furthermore, inadvertent puncture of the adjacent carotid artery can be treated with direct pressure, unlike the scenario for the subclavian vein/artery cannulation.
The hierarchy of central vein sites for the tunneled dialysis catheters is shown in Table 87-1. Despite the advantages of the right internal jugular highlighted above, the left internal jugular vein should be used with caution; the tortuous course from the cannulation site to the superior vena cava increases the risk of catheter malposition, injury to the central veins, and central vein stenosis/thrombosis. Although somewhat paradoxical, it is often feasible to place a dialysis catheter through an occluded or thrombosed jugular vein. If it is possible to pass a wire, the tract through the thrombosed vein can usually be dilated sufficiently to facilitate passing the catheter. Furthermore, this approach is associated with a fairly low complication rate given the fact that the vessel is already occluded. A variety of alternative sites are listed in the table. Notably, they are not listed in a specific order, but, rather, should be considered potential options to be explored in the challenging patient who has exhausted the more traditional options. A detailed description of the techniques for placing catheters in these alternative sites is beyond the scope of this chapter, but several can be found among the Suggested Readings at the end of this chapter. The subclavian vein should not be used as a site for tunneled or nontunneled dialysis catheters except in fairly extreme situations. Dialysis catheters placed in the subclavian vein result in a significant (>30%) incidence of stenosis and/or occlusion that precludes a permanent access in the ipsilateral extremity. Although well appreciated by nephrologists and access surgeons, it is important to educate our medical and critical care colleagues about this adverse sequela.
Pre-operative Assessment
The pre-operative preparation prior to the placement of a nontunneled catheter is fairly minimal, because it is a relatively straightforward bedside procedure. Indeed, most of the patients are already hospitalized and are frequently in the intensive care unit. Perhaps the most important issue is to determine whether a nontunneled catheter is the best access option. It is important to inquire during the history about any previous access procedures, central vein cannulations, or problems with central vein cannulations. Because the catheters are placed percutaneously directly into the vein, anticoagulation is not generally considered a contraindication. Ultrasound guidance can be used to potentially reduce the incidence of bleeding complications if the patients are coagulopathic or having a bleeding disorder. Furthermore, ultrasound can be used to confirm the size/ patency of the vein and its relationship to the adjacent artery. The incidence of bleeding complications can be further reduced by using a micropuncture needle (i.e., 21 gauge).
The pre-operative preparation before the placement of tunneled dialysis catheters is a little more involved and similar to most surgical procedures. The catheters are usually inserted in the operating room or fluoroscopy suite using conscious sedation and local anesthesia. In most institutions, this requires specific training in conscious sedation and/or the presence of an anesthesiologist/nurse anesthetist. Uncooperative
patients may require general anesthesia. All anticoagulation should be stopped and any underlying coagulopathy or bleeding disorder corrected. Bleeding within the subcutaneous tunnel can be quite troublesome and increases the risk of infectious complications. Occasionally, it is not possible to reverse all anticoagulation or bleeding diatheses. The absolute requirements for tunneled catheter placement in our practice include an international ratio (INR) ≤1.8, a platelet count >50,000 thousand/mm3, and an activated clotting time (ACT) <200 seconds. Additionally, any contrast allergy should be identified and pretreated, because it is occasionally necessary to administer a small volume of contrast to outline the central venous anatomy and confirm the location of the catheter. Standard sterile technique is used and prophylactic antibiotics are routinely administered pre-operatively, although their benefit in this setting remains unclear.
patients may require general anesthesia. All anticoagulation should be stopped and any underlying coagulopathy or bleeding disorder corrected. Bleeding within the subcutaneous tunnel can be quite troublesome and increases the risk of infectious complications. Occasionally, it is not possible to reverse all anticoagulation or bleeding diatheses. The absolute requirements for tunneled catheter placement in our practice include an international ratio (INR) ≤1.8, a platelet count >50,000 thousand/mm3, and an activated clotting time (ACT) <200 seconds. Additionally, any contrast allergy should be identified and pretreated, because it is occasionally necessary to administer a small volume of contrast to outline the central venous anatomy and confirm the location of the catheter. Standard sterile technique is used and prophylactic antibiotics are routinely administered pre-operatively, although their benefit in this setting remains unclear.
 Get Clinical Tree app for offline access 
|