(1)
Section for Transfusion Medicine, Capital Region Blood Bank, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark
(2)
Department of Surgery, Center for Translational Injury Research, The University of Texas Health Science Center, Houston, TX, USA
(3)
Department of Cardiothoracic Surgery, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark
(4)
Trauma, Critical Care and Acute Care Surgery, Scott and White Memorial Hospital, Texas A&M University, Temple, TX, USA
12.1 Introduction
12.2.1 Anatomy
12.2.2 Physiology
12.4 Initial Management
12.5 Surgical Management
12.5.2 Specific Injuries and Repair
12.5.3 Intracardiac Injuries
12.5.6 Special Considerations
12.5.7 Equipment
12.7 Outcomes
12.8 Conclusion
Abstract
Blunt trauma to the heart and great vessels is often secondary to a high-energy impact to the thorax, leading to major injuries that can be rapidly fatal in many circumstances. Those patients who arrive to the emergency room with signs of life are candidates for an immediate thoracotomy. Patients who are stable may be candidates for diagnostic imaging, including ultrasonography, computed tomography, and invasive arteriography. The initial management of all patients should follow ATLS guidelines. Following the decision to proceed to surgery, an appropriate incision that maximizes access to key structures should be chosen. Full-thickness sutures for atrial lesions will avoid tearing of this thin tissue. Pledgeted sutures may be necessary for partial-thickness sutures in the ventricles. Injury to the great vessels requires proximal (i.e., hilar clamping) and distal control, and extracorporeal membrane oxygenation (ECMO) may be required in select patients following surgical correction of bleeding. Early involvement of cardiothoracic surgeons is often beneficial to help optimize overall care.
Jesper B. Ravn, MD and Justin L. Regner, MD contributed equally as senior authors.
12.1 Introduction
Penetrating and blunt cardiac injuries are by their very nature extremely lethal, and consequently only a fraction of patients with a cardiac wound will be alive when reaching the hospital [1–4]. Patients that do arrive to the ED with penetrating thoracic trauma can be divided broadly into three hemodynamic categories on a continuum of physiologic derangements from “in extremis” or near death (5 %) to unstable (15 %) to stable (80 %), and for the former category immediate surgery and often a massive blood transfusion is the only treatment modality that offers possible survival [5]. For patients that arrive without any sign of life, only a select group is eligible for an emergency department thoracotomy [6, 7]. While the decision to operate is readily made for unstable patients, stable patients with a possible cardiac wound, i.e., patients with a penetrating injury or high-energy blunt force to the precordium but presenting without any apparent physiologic abnormalities, can be challenging to correctly diagnose and treat in a safe, timely, and minimally invasive fashion. Patients with suspected cardiac and great vessel injuries in extremis should receive the standard ED thoracotomy via a left anterolateral thoracotomy. Different imaging modalities, such as focused assessment with sonography in trauma (FAST), echocardiography, and computed tomographic arteriogram (CTA), can assist the diagnosis, but if equivocal a pericardial window may be the only way of ruling out intrapericardial bleeding [2, 3, 8–10].
The majority of blunt cardiac injuries (BCI) are contusions to the myocardium that can be treated conservatively with telemetry and expectant management; however, severe BCI may cause myocardial defects or valvular injuries which may require surgical repair with cardiopulmonary bypass. Historically the frequency of injury to the heart chambers in penetrating injuries has been reported to be predominantly and evenly affecting the ventricles, and less frequently the atria, with the left atrium being the least frequent [11]; this of course is highly dependent on the mechanism of injury and the trajectory of the wounding object. Accordingly, efforts should be made to establish the forces involved in the injuring process, e.g., bullet caliber, range, and for stab wounds the length of the object, as this will assist the diagnostic process.
Blunt cardiac injury (BCI) can be the result of a high-energy impact to the thorax, crushing, or a rapid deceleration [2, 3]. In cases of rapid deceleration, the heart may suffer injuries where fixed structures attach to the freely suspended heart, predominantly at the atria-vena cava junction and pulmonary vein [2, 3]. BCI can also result due to cardiac squeezing or sudden changes in intrathoracic or intra-abdominal pressure and may include cardiac rupture – often right atrium, septal injury, or valvular insufficiency [2]. In cases involving a blunt mechanism of injury, e.g., a motor vehicle accident, the injury to the heart itself may be of a penetrating nature, due to sharp fragments of bone from a rib, sternum, or spinal fracture, and therefore might not be readily observable during initial inspection.
12.2 Anatomy and Physiology
12.2.1 Anatomy
Salvaging trauma patients with cardiac and great vessel injuries requires intimate knowledge of both anatomy and physiology. The surgical anatomy includes the anterior, middle, posterior, and superior mediastinum, its vasculature and nerves. Physiology includes cardiac tamponade, hemorrhagic shock, and projectile path.
The mediastinum is defined by the diaphragm inferiorly, the pleura laterally, the sternum anteriorly, and the vertebral column posteriorly. Surgically, the mediastinum should be evaluated from the perspective of what is injured in the pericardium versus what could be injured outside the pericardium. The pericardium is a robust fibrous sac that completely contains and protects the heart. Its strength forms the basis of tamponade. The pericardium contains the heart, proximal ascending aorta, pulmonary artery, pulmonary veins, and inferior portion of the superior vena cava. In addition to these structures, the phrenic nerves reside in the lateral middle mediastinum bilaterally.
The remainder of the mediastinal structures resides outside the pericardium. The anterior mediastinum is mainly a potential space between the pericardium and sternum. Bleeding in this area is usually self-limited if from sternal fractures, but occasionally arises from internal mammary or proximal intercostal artery injuries. The posterior mediastinum contains the esophagus, descending thoracic aorta, thoracic duct, vagus nerves, and azygous and hemiazygous veins. These structures are discussed in preceding chapters. The superior mediastinum is divided from the middle mediastinum by the pericardium. This division may serve as a road map of safety to gain initial control of superior mediastinal hemorrhage since hematomas in this area are relatively uncontained making dissection difficult. The superior mediastinum includes the aortic arch, innominate, left carotid, and left subclavian arteries; innominate vein; superior portion of the superior vena cava; and vagus, recurrent laryngeal, and phrenic nerves.
The nerves of the mediastinum are easy to injure and difficult to locate in trauma. Bilateral phrenic nerves arise from cervical roots 3–5. The right runs inferiorly on the anterior border of the anterior scalene and enters the thoracic cavity anterior to the second portion of the subclavian artery but posterior to the subclavian vein. It then proceeds caudally to the inferior vena cava hiatus in the diaphragm by passing anterior to both the right atria and the right pulmonary hilum. The left phrenic nerve descends along the anterior scalene and passes into the thoracic cavity anterior to the first portion of the subclavian artery, posterior to the vein. It then passes anterior to the left pulmonary hilum and over the pericardium of the left ventricle to the left diaphragm. The left vagus nerve descends to the thoracic cavity in the carotid sheath. It passes anterior to the aortic arch between the left carotid and subclavian arteries. At the level of the aortic arch, it branches into the vagus and left recurrent laryngeal nerve. The left recurrent laryngeal nerve ascends superiorly to the larynx in the tracheoesophageal groove. The vagus descends into the abdomen posterior to the left pulmonary hilum to become the anterior vagus of the stomach as it exits the esophageal hiatus. The right vagus nerve descends in the carotid sheath and passes anterior to the right subclavian artery to divide into the recurrent laryngeal and the vagus. The right vagus then descends posterior to the pulmonary hilum to the esophageal hiatus to become the posterior vagus of the stomach.
12.2.2 Physiology
Cardiac and great vessel injuries create hemodynamic instability and death due to either cardiac tamponade or hemorrhagic shock. Cardiac tamponade is similar to the Monroe Doctrine of brain injury. The pericardium is a fairly fixed container divided into two separate spaces, intracardiac and extracardiac. Increases in one space force corresponding decreases in the other. With traumatic cardiac tamponade, the time to cardiac failure is based on the etiology of the blood source. If it is an atrial injury or partial ventricular injury, it can be hours. Eventually the extracardiac pressure begins to approximate or exceed the atrial filling pressure with resultant hypotension and venous congestion. This hypotension can initially be overcome with increased preload, but is only a temporization. Cardiac tamponade left untreated will eventually result in cardiac failure with equalization of the extracardiac and intracardiac (both atrial and ventricular) pressures.
Hemorrhagic shock by its very nature requires blood loss; however, the source of shock may not be evident at first. Penetrating thoracic trauma to the heart and great vessels can hemorrhage directly from the entry and exit wounds or into an adjacent body cavity. However, these intrathoracic injuries may actually be tangential with the source of hemorrhage from another organ and body cavity. Historically the frequency of injury to the heart chambers with penetrating mechanisms has been reported predominantly affecting the ventricles, and less frequently the atria, with the left atrium being the least frequent [10]; this is highly dependent on the mechanism of injury and the trajectory of the wounding object. Accordingly, efforts should be made to establish the forces and vector involved in the injuring process, e.g., bullet caliber, range, and for stab wounds the length of the object, as this will assist in diagnosing. Cardiac injuries typically present with tamponade or direct bleeding. Great vessel injuries, on the other hand, can be more insidious. These superior mediastinal contents may suffer blast effect or contusion, tangential injuries, partial wall injury with pseudoaneurysm formation, or branch vessel injury. This difference in injury pattern accounts for the range of hemodynamic profiles present with this patient population.
12.3 Clinical Assessment and Diagnostic Testing
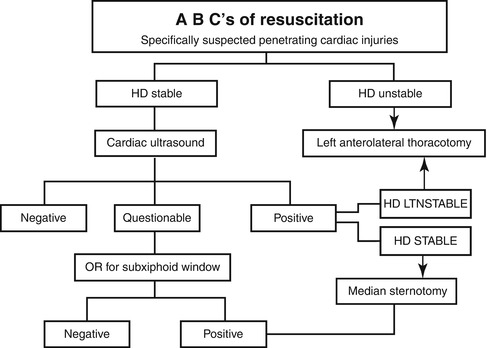
The aim of this section is to discuss the advantages and shortcomings of clinical signs, imaging modalities, and other diagnostic procedures in evaluating cardiac, great vessel, and hilar injuries. It must be emphasized again that emergent thoracotomy should not be delayed by diagnostic procedures in hemodynamically unstable patients and especially patients “in extremis.” A simple and direct algorithm was developed by Mattox in 2000 and remains applicable today (Fig. 12.1).
Any patient with a penetrating mechanism, specifically a projectile, is at risk of a cardiac injury with subsequent cardiac tamponade or hemorrhage [2, 9, 12]. Traditionally, trauma surgeons have been taught to expect a cardiac injury when an exterior wound was located in “the box” (Fig. 12.2). However, with current military and civilian ballistics, cardiac injury can occur from any entry point into the body. The earliest signs of hemorrhage are due to sympathetic nervous system surge with increases in heart rate, respiratory rate, and peripheral vascular resistance, i.e., narrowed pulse pressure. On exam, these patients will have pallor, agitation, or anxiety [11–13]. If blood is collecting in the pericardium rather than being drained either externally or into the thoracic cavity, a cardiac tamponade can occur. Awake patients early in tamponade physiology will not be comfortable in the supine position as this compromises their venous return and right heart cardiac output. Many of the classical signs of tamponade or Beck’s triad, i.e., muffled heart sounds, distension of jugular veins, and hypotension will often be absent or difficult to observe in the trauma bay [12]. Frequently trauma patients early in the tamponade physiology may not present with any symptoms of cardiac injury and yet later succumb to cardiac tamponade or exsanguinating wounds. In fact, an increased mortality from cardiac trauma has been reported in large case series when the exterior wound was located away rather than inside the precordium, possibly due to a lower-level of suspicion and attention from the clinical team [9].
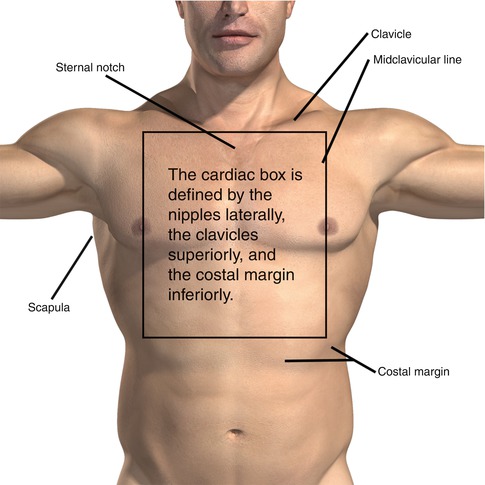
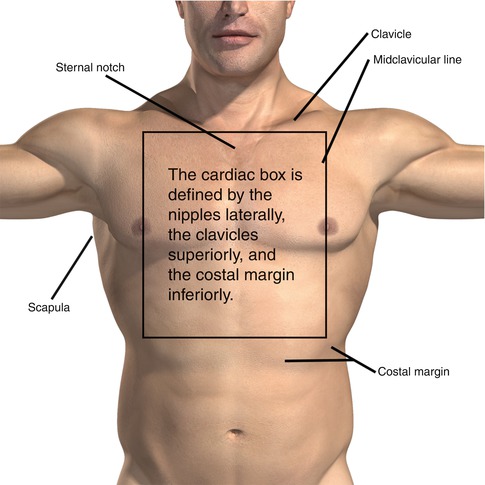
Fig. 12.2
The mediastinum is defined by the diaphragm inferiorly, the pleura laterally, the sternum anteriorly, and the vertebral column posteriorly
Evaluation of the trauma patient and specifically the unstable patient occurs best with a regimented approach. Blunt injury to the pericardium can be evaluated in the same manner as penetrating. Portable chest radiographs remain the best initial film to assess the thorax for injury and ballistic vector. The FAST exam or ultrasound is the trauma surgeon’s best friend in evaluating for internal bleeding [14]. All unstable blunt trauma patients once the initial ABC’s of trauma are complete require a FAST exam [14, 15]. Patients with penetrating thoracic trauma require a focused cardiac ultrasound to evaluate for pericardial effusion [16, 17].
The FAST is specific and sensitive for intra-abdominal and cardiac injuries with a sensitivity for intra-abdominal fluid of 81–88 %, 99 % specificity, and 97 % accuracy and sensitivity of pericardial fluid approaching 100 % [14–16]. The ultrasound can also evaluate pneumo- and hemothorax with excellent sensitivity assuming the patient does not have subcutaneous emphysema [16, 18]. If the patient is stable and the penetrating mechanism crosses the mediastinum without evidence of cardiac injury on ultrasound, then these patients require evaluation of their mediastinum for injuries. Multi-detector CTA of the chest provides excellent evaluation of the superior mediastinal vascular structures [19]. In addition, these images will assist with surgical planning, incision choice, and evaluation of other injuries. If concern remains regarding middle mediastinal injury, then the subxiphoid pericardial window should be considered the gold standard for detecting blood in the pericardium [8, 12]. For the most part penetrating cardiac and great vessel injuries will be diagnosed by either exsanguinating hemorrhage, ultrasound of the pericardium, CTA or angiography of the chest, or subxiphoid window.
Video-assisted thoracic surgery (VATS) is being introduced to evaluate hemodynamically stable patients for intrapericardial injuries [20]. We recommend a modified VATS approach, using only partial pulmonary deflation, and limiting the deflation to a few respiratory cycles, as well as reserving this diagnostic approach for the completely stable patients as not all patients will tolerate the periprocedural reduction in pulmonary capacity. This approach could be combined with an otherwise indicated chest tube placement. Unstable patients should be evaluated by TTE or TEE at the bedside or in the operating theater for the detection of complex cardiac injuries such as cardiac wall and septal defects, valvular insufficiency, or injuries to the pulmonary artery and vein [20]. For stable patients, a chest X-ray and 12-lead ECG should be obtained to screen patients suspected of myocardial ischemia or contusion, conduction abnormalities, or arrhythmias that may be present in BCI [2, 21]. Biomarkers of myocardial cell damage are generally not used to estimate the seriousness of injury as they can be either normal or elevated in the presence of significant cardiac injury [3]. However in blunt trauma, the combination of a normal ECG, normal chest X-ray, and normal levels of troponin I has a very high negative predictive value [22, 23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree