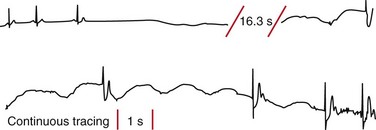
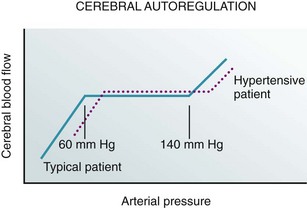
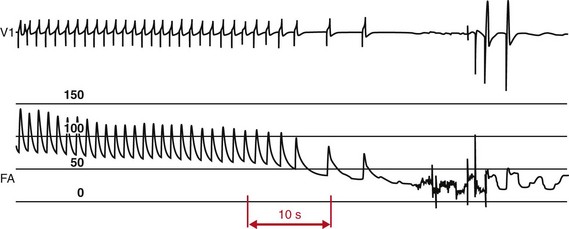
66 Transient Loss of Consciousness and Syncope Pathophysiology of Loss of Consciousness Approach to the Syncope Diagnosis Physiological Impact of Upright Posture Pathophysiology of Vasovagal Syncope Pathophysiology of Orthostatic Hypotension Orthostatic Provocation for Assessing Susceptibility to Vasovagal Syncope and Orthostatic Hypotension: Rationale and Methods Head-up tilt table has been used for longer than half a century by physiologists and physicians to study heart rate and blood pressure adaptations to changes in position, to model responses to hemorrhage, to assess the characteristics of orthostatic hypotension, and to evaluate hemodynamic and neuroendocrine responses in congestive heart failure, autonomic dysfunction, and hypertension. During the course of such studies, incidental observations noted that some test subjects experienced total or near-total transient loss of consciousness as a result of systemic hypotension.1–5 Furthermore, in some cases hypotension was associated with impressive degrees of bradycardia, including prolonged self-terminating periods of asystole (Figure 66-1). However, these early studies did not incorporate a more formal assessment of the diagnostic utility of this observation at the time. Figure 66-1 Electrocardiographic (ECG) monitor recording obtained during a spontaneous vasovagal faint, illustrating a self-terminating prolonged asystolic pause. The patient was deemed to have cardioinhibitory syncope. Concomitant vasodepressor (vasodilatation) also was probably present but could not be documented by current ambulatory technology. The concept of head-up tilt table provocation as a diagnostic test for reflex syncope began to evolve only after the landmark report by Kenny and colleagues in 1986.6 At first, prolonged periods (up to 2 h) of passive head-up posture with the patient resting on a tilt table (at 40° to 60°) were used as the sole means of provoking vasovagal events. Subsequently, additional interventions were introduced in an attempt to improve the sensitivity of the test, although at some detriment to specificity. These interventions included pharmacologic provocation (primarily isoproterenol or nitroglycerin, but also adenosine, edrophonium, and clomipramine). Furthermore, certain physical maneuvers including carotid sinus massage (at times in conjunction with edrophonium) were used in some laboratories. Currently, isoproterenol and nitroglycerin remain the most widely used pharmacologic provocative agents in diagnostic tilt table testing laboratories. In a recent survey, nitroglycerin was more widely used in Europe, and isoproterenol was preferred in North America. Although the utility of tilt table testing remains controversial, the test has nonetheless become widely accepted as a valuable tool for the evaluation of susceptibility to vasovagal syncope.7 This chapter summarizes the rationale for and current status of head-up tilt table testing as principally applied to evaluation of the vasovagal faint. Syncope is a clinical syndrome, not a specific diagnosis; it is characterized by a transient and self-terminating interruption of normal global cerebral activity with associated loss of consciousness and postural tone. The underlying cause is a relatively brief period (a minute or two at the most) of inadequate delivery of oxygen, glucose, and other nutrients to brain tissues.7,8 Although syncope is the most common basis for transient loss of consciousness (TLOC), it is but one of many conditions that must be considered when a patient presents with an apparent collapse. Consequently, before the evaluation proceeds to assessment of possible underlying causes in a patient with presumed syncope, careful consideration must be given to distinguishing the presenting complaint from the many other forms of TLOC or TLOC mimics (e.g., seizures, concussion, psychogenic pseudosyncope, malingering). Unfortunately, physicians often are uncertain about this distinction, with confusion exacerbated by imprecise writing in the medical literature, as has been highlighted recently.9,10 Neuronal tissue has limited energy storage capability. Consequently, a well-maintained flow of oxygenated blood to the brain is crucial; the autoregulation of cerebrovascular blood flow is crucial in this regard. In healthy young persons, cerebral blood flow ranges from 50 to 60 mL per 100 g of brain tissue/min, representing about 12% to 15% of resting cardiac output. A flow of this magnitude easily meets minimum oxygen (O2) requirements to sustain consciousness (approximately 3.0 to 3.5 mL O2/100 g tissue/min).11,12 However, the safety factor for oxygen delivery may be markedly impaired in older individuals; in individuals with diseases such as hypertension, diabetes mellitus, or heart failure; and in those in a hypoxemic state (e.g., chronic pulmonary disease) (Figure 66-2). Figure 66-2 Schematic graph illustrating the relation between cerebral blood flow (ordinate) and systemic arterial pressure (abscissa) in a “typical” patient and a hypertensive patient. Cerebral flow is “autoregulated” over a wide pressure range (i.e., does not vary over this pressure range). The range is influenced by concomitant disease conditions such as hypertension, as indicated here. Below approximately 60 mm Hg, blood flow falls, which may lead to loss of consciousness. In general, sudden cessation of cerebral blood flow for 10 seconds or longer is usually sufficient to cause complete loss of consciousness. Furthermore, whatever the heart rate, either a decrease in systolic blood pressure to below 60 mm Hg or a fall of as little as 20% in cerebral oxygen delivery may trigger syncope (see Figure 66-2). Many conditions may cause physiological disturbances leading to syncope; neurally mediated reflex syncope, orthostatic hypotension, and tachyarrhythmias or bradyarrhythmias are among the more frequent causes. Vasovagal syncope is the most frequent form of the neurally mediated reflex faints (Box 66-1), and is the most common of all causes of syncope across all age groups. Accordingly, its recognition (and, if necessary, preventive treatment) is a problem often encountered by a wide range of medical practitioners. In the case of vasovagal syncope, the diagnosis can usually be established by the medical history without further testing, although the history taking may need to include observations made by eyewitnesses.7,8 When events surrounding the faint(s) are “atypical,” however, even an experienced history taker may not be certain of the diagnosis. Furthermore, often it is not possible to obtain an adequate history (especially in the elderly or the very young). In some of these latter instances, absence of reliable facts may be due to the patient’s lack of insight, or (especially in the elderly) to retrograde amnesia for premonitory events.13 Furthermore, eyewitnesses may not have been present, or their reports may not be sufficiently detailed to establish a diagnosis of the cause of the syncope. In such cases, the availability of diagnostic tests becomes important. Upright posture elicits an orthostatic stress caused by the effects of gravity on the distribution of circulating blood volume in the body.1,2,4,6–8,11 Initially, as upright posture is achieved, the effects of gravity result in shifting of approximately 500 to 1000 mL of blood to the lower part of the body and particularly into the highly compliant splanchnic bed.11,14 Most of this redistribution occurs in the first 10 seconds of upright posture. Subsequently, in normal persons, an additional 700 mL of protein-free fluid is filtered into the interstitial space in the next 10 min.11 The result of these two shifts of fluid within and outside of the vascular space is marked reduction of venous return and stroke volume. Humans attempt to compensate for diminution of stroke volume during movement to upright posture by both increasing heart rate and constricting resistance and capacitance vessels.11 Heart rate increase alone, however, is usually insufficient to maintain cardiac output and cerebral blood flow during these circumstances. Vasoconstriction of systemic blood vessels is crucial to maintenance of arterial blood pressure. Prevention of syncope requires that the compensatory cardiovascular response maintains arterial pressure (in particular, systemic pressure at the level of the carotid arteries) at a value at least equal to the minimum value needed to guarantee adequate cerebral blood flow (approximately 60 mm Hg).12 Failure of compensatory adjustments to orthostatic stress may, in the absence of preexisting volume overload, result in inability to maintain central volume (the heart cannot pump what it does not receive), reduction of systemic arterial pressure, and inadequate cerebrovascular blood flow. If the deficits are sufficiently severe, the ultimate outcome is nearly complete or complete loss of consciousness caused by systemic hypotension. The outcome, when principally due to inadequate maintenance of blood pressure in the face of gravitational stress is usually termed orthostatic hypotension or orthostatic syncope. In addition, however, in susceptible persons, an inappropriate set of neural reflex responses may be triggered: vasodilatation and severe or “relative” bradycardia—the vasovagal response.7,11,15 The vasovagal reflex in humans appears to have a long evolutionary history,16 but the basis for the reflex remains uncertain. In this regard, several theories have developed, two of which may be based on early protective mechanisms. The first relates to protection from predators by means of “playing dead” (perhaps a particular advantage for human noncombatants such as women and children)—a strategy that is presumed to buy time and set up an opportunity for later escape. A second, the so-called “clotting hypothesis,” may have been a means of reducing severity of hemorrhage by reducing blood pressure and flow. Other theories attribute the vasovagal reflex as being (1) the human equivalent of the “alarm” reaction in some animals that is marked by heart rate slowing and reduced blood pressure; or (2) a means of cardioprotection under conditions of extreme stress.16 Whatever the origins of the vasovagal reflex, it is thought to be triggered at least in part by excessive stretch of central mechanoreceptors (including those residing in the atria and possibly in the left ventricle) as intrathoracic circulating volume falls. Of note, however, although this mechanism may contribute to vasovagal faints triggered by upright posture, other common triggers (e.g., pain, emotional upset) are not readily accounted for by this explanation. In any event, it is the upright posture–triggered reflex that forms the basis for the use of tilt table testing in the evaluation of patients with suspected vasovagal syncope.6,7,17,18 Vasovagal syncope is the most frequently occurring form of a larger group of neurally mediated reflex faints that also include carotid sinus syndrome and postmicturition syncope (see Box 66-1). In terms of pathophysiology, carotid sinus syndrome (CSS) is perhaps the best understood of the neurally mediated reflex syncope syndromes.19 In CSS, excessive stretch of carotid baroreceptors (perhaps initiated by abrupt neck movements or tight collars) provides an increase in afferent signals to the central nervous system. Central processing of these signals ultimately causes an efferent neural reflex response, resulting in heart rate slowing and vascular dilatation to compensate for a perceived increase in central arterial pressure. In many cases, concomitant denervation of afferent proprioceptive nerves is thought to occur, thereby depriving the central nervous system of critical information indicating that neck movement was in fact the instigating trigger.19,20 Presumably, on the basis of the latter additional information, the central response to the afferent signals would be modified. As noted earlier, the pathophysiology of the vasovagal form of neurally mediated reflex syncope remains incompletely understood. However, it can be considered in terms of four basic elements: (1) the afferent limb; (2) central nervous system processing; (3) the efferent limb; and (4) feedback loops.18 In brief, central and peripheral mechanoreceptors (see earlier) and occasionally chemoreceptors (e.g., in the presence of myocardial ischemia) are presumed to initiate afferent sensory nerve traffic to the cardiovascular modulation center in the brain stem. The manner in which sensory processing results in inappropriate vasodilatation and/or bradycardia is unknown, but may in part relate to lack of concordance among several afferent inputs, analogous to the situation described earlier for CSS. In any event, systemic hypotension (ultimately leading to a vasovagal faint, if severe) is primarily the result of vasodilatation triggered by a marked reduction in sympathetic vasoconstrictor outflow to blood vessels in skeletal muscles and substantial increase in venous capacitance, particularly in the splanchnic bed.14 Parasympathetically mediated bradycardia (severe, or “relative,” with respect to the severity of hypotension) contributes to the process but plays a lesser role, except when prolonged asystole occurs. A poorly understood failure of baroreceptor feedback to recognize and interrupt this process also appears to be important in facilitating development of hypotension.21 Impaired cerebral autoregulatory responses also may contribute to the development of vasovagal responses in some patients. It has been reported that cerebral blood flow velocity can decline before arterial pressure and cerebral vasoconstriction, and that in some cases, cerebral hypoxia may occur in the absence of systemic hypotension. The role of cerebrovascular spasm as a mechanism for transiently inadequate cerebral perfusion has been raised, but its frequency and importance are unclear.22 Several observations suggest that symptomatic hypotension-bradycardia associated with a positive result on head-up tilt table testing is comparable with spontaneous neural reflex–mediated vasovagal syncope. First, both spontaneous and induced syncopal episodes tend to be associated with similar premonitory symptoms (e.g., nausea, diaphoresis) and signs (e.g., preceding tachycardia followed by relative or marked heart rate slowing, marked pallor, loss of postural tone). Second, the temporal sequence of blood pressure and heart rate changes during tilt-induced syncopal spells parallels that reported for spontaneous episodes (Figure 66-3). Finally, measurements of plasma catecholamines before and during spontaneous and tilt-induced syncope exhibit important similarities. In particular, premonitory increases in circulating catecholamines, epinephrine more than norepinephrine (i.e., before evident systemic hypotension), appear to characterize both the spontaneous vasovagal faint and tilt-induced hypotension-bradycardia.18,23 Figure 66-3 Laboratory recording illustrating typical heart rate (upper panel) and blood pressure (lower panel) changes associated with head-up tilt table–induced vasovagal syncope. Blood pressure from the femoral artery (FA) is indicated in mm Hg. From a clinical perspective, most vasovagal fainters exhibit mixed cardioinhibitory and vasodepressor responses (Box 66-2).24,25 In some patients, however, the observed response will be predominantly cardioinhibitory, with hypotension caused by a prolonged asystolic pause. On rare occasions, a pure vasodepressor response may be observed, although even in these cases the concomitant tachycardia is less than that expected for the severity of hypotension. Classification of the various types of vasovagal responses is difficult, and its clinical usefulness is doubtful; as was demonstrated in the International Study on Syncope of Uncertain Etiology (ISSUE), heart rate–blood pressure features recorded during tilt table observations only infrequently coincide with those accompanying spontaneous faints in a specific patient.25 In any case, the most widely accepted classification is that derived from the Vasovagal Syncope International Study (VASIS) (see Box 66-2).24,25 By definition, a pure cardioinhibitory response manifests as an abrupt heart rate decrease to rates less than 40 beats/min with or without asystole, and depressed atrioventricular (AV) conduction, with accompanying blood pressure decrease. A vasodepressor response is defined as a significant blood pressure decrease, usually abrupt, and independent of heart rate changes (<10% from baseline). Mixed vasovagal response may be predominantly cardioinhibitory or vasodepressor in nature. The physiological impact of movement to upright posture was summarized earlier. Fortunately, frank syncope induced by moving from a supine or seated to an upright posture is uncommon in healthy persons (although “near-syncope” or “gray-out” is common), but becomes a very important problem in elderly and less physically fit individuals, and in patients who are volume depleted (including excessively diuresed heart failure patients). Two basic forms of orthostatic hypotension (OH) are recognized.7,8,26 The first, so-called “immediate OH,” occurs almost immediately upon standing and is usually brief and benign. The affected individual may be of any age and level of fitness. The symptoms are those of “graying-out.” Postural tone is not typically lost; generally the patient holds on to a chair or some other nearby object, and within 10 to 15 seconds, the symptoms pass. The second is the “classic” or “delayed” form of OH. This is a more serious problem, as the symptoms are delayed and may not occur for several minutes after change of posture. In some cases, a very delayed form of OH occurs; this may develop 10 to 15 min or even later after a postural change. At this time, the patient may be taken entirely unaware, no longer capable of self-protection. The fact that syncope does not occur more often during prolonged periods of upright posture, or when one moves from sitting or supine position to standing, suggests that skeletal muscle pump activity and vasoconstrictor neural control networks are highly efficient in health. However, they may become less effective under a variety of conditions.7,8,15 For example, healthy individuals returning from a weightless environment (e.g., astronauts) and others who experience prolonged bed rest (e.g., hospitalization) may exhibit OH induced by presumed “deconditioning” of autonomic nervous system responsiveness. Similarly, disease states (e.g., parkinsonism, pure autonomic failure, diabetes, chronic alcohol abuse) may act to diminish nervous system response. Additionally, in many patients, particularly the elderly, the effectiveness of the autonomic nervous system response may be undermined by medication for concomitant conditions (e.g., hypertension, ischemic heart disease, psychiatric problems). Finally, inadequate fluid intake, especially by older persons who have diminished thirst drive, is an important consideration.15,27 Although imperfect, head-up tilt table testing is the laboratory technique of choice for unmasking susceptibility to vasovagal faint in patients with unexplained syncope.7 Applications and indications for testing are summarized in Box 66-3. On the other hand, active standing appears to be preferred for eliciting susceptibility to OH and orthostatic syncope, presumably because of the engagement of skeletal muscle activity with blood flow that such activity demands. In either case, beat-to-beat heart rate and blood pressure monitoring is preferred.
Head-up Tilt Table Testing
Historical Background
Transient Loss of Consciousness and Syncope
Pathophysiology of Loss of Consciousness
Approach to the Syncope Diagnosis
Physiological Impact of Upright Posture
Pathophysiology of Vasovagal Syncope
Pathophysiology of Orthostatic Hypotension
Orthostatic Provocation for Assessing Susceptibility to Vasovagal Syncope and Orthostatic Hypotension: Rationale and Methods



