Chapter contents
5.1 Positioning the patient 46
5.2 Locating the radial artery 47
5.3 Locating the pulse positions for assessment 49
5.4 Practitioner positioning 51
5.5 Assessing the parameters 51
5.6 Locating the pulse depth 53
5.7 The normal pulse 56
5.8 Assessing health by the pulse 57
5.9 Channel, organ and levels of depth 58
5.10 Comparison of the overall force of the left and right radial pulse 58
5.11 Pulse method 59
5.12 Other considerations when assessing the pulse and interpreting the findings 61
5.13 Summary 68
Although an objective terminology is essential for radial pulse diagnosis, it is equally imperative to have reliable procedures and a consistent method when palpating the pulse. Pulse procedures refers to the processes preceding pulse assessment as well as the actual techniques used during this process. These procedures encompass:
• Positioning of the patient and practitioner
• Procedure for locating the three pulse positions
• Techniques for locating and assessing the different levels of depth
• Assessment of the arterial structure and pulse wave contour.
The ordering of these techniques and procedures is described as the pulse method. As we established in Chapter 4, pulse method refers to:
• How and when to apply the pulse taking
• The order of gathering information from the pulse using the different techniques (depth, length, strength of application) and required body part (pulse position)
• The consistent application of the pulse method and techniques used in the same way every time.
Identification of many of the specific CM pulse qualities depends on the measurement of pulse parameters in specific positions, so a consistent method is of vital importance. The objective for developing and using a consistent method of pulse palpation is to limit the variance of pulse findings attributable to technique. Once such variances are controlled, then any findings with palpation can be confidently attributed to the occurrence of actual pulse differences.
This chapter focuses extensively on the first stage of the pulse diagnosis process — the application of correct technique and procedures. A further stage of the pulse diagnosis process, interpreting pulse assessment findings diagnostically, is dealt with extensively in Chapter 6 and Chapter 7. We also investigate the organization of the techniques and procedures and their order of application, and discuss the benefits of developing a pulse method that is systematic in its application.
5.1. Positioning the patient
Before the pulse is assessed, the patient needs to be positioned appropriately. Appropriate patient positioning allows the practitioner maximal access to the radial artery for assessment purposes while preventing any postural changes that may affect blood flow. For example, if the patient slouches, their respiration will be poor and this will cause a corresponding decrease in pulse strength. Postural slouching and arterial compression from poor arrangement of the upper limbs impede blood flow from the central arteries into the peripheral arteries, limiting the propulsion effect that the pressure wave has on moving blood. In this situation any assessment of the pulse will be inaccurate and unreliable.
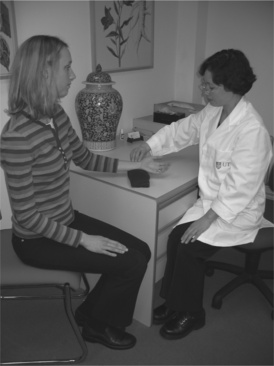
The pulse is most commonly taken when the patient is seated, but assessment can also occur when the patient is lying supine (Box 5.1). Irrespective of the positioning approach used, the arm is always placed at the level of the patient’s heart. Holding the arm lower or higher than the heart level affects the pulse pressure, causing changes in the pulse wave. Ensuring that the arm is level will minimise these postural related pressure differences. Pulse examination is undertaken on both the left and right arms (Fig. 5.4).
Box 5.1
Positioning the patient for assessing the pulse
• Arm level with the heart
• Patient’s legs uncrossed
• Patient should be sitting upright or lying supine
• Support the wrist when extended with a towel or cushion
 |
| Figure 5.4Bilateral hand palpation. The practitioner’s left hand is palpating the right pulse and the right hand is palpating the left hand the pulse. |
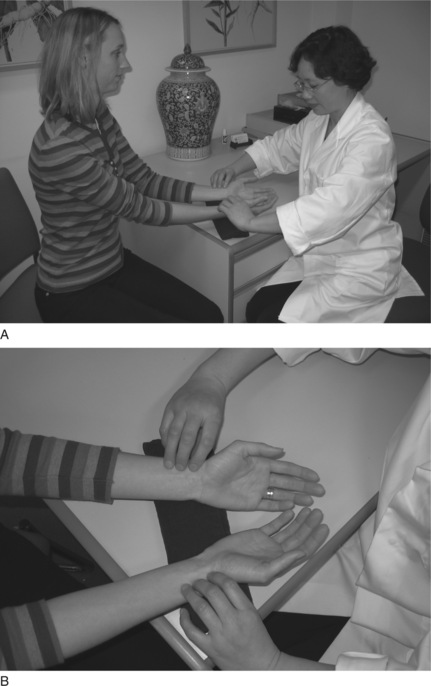
If sitting, the patient’s legs should be uncrossed with feet placed flat on the floor. Their posture should be relaxed but upright so that the thorax region is not constricted during respiration, allowing the lungs to expand and contract freely. The wrist should be extended straight with the palm facing upwards (Fig. 5.1). Similarly, when lying supine, the patient should have their legs uncrossed, wrist extended with the palm facing upwards (Fig. 5.2).
 |
| Figure 5.1Positioning of the practitioner taking the pulse when the patient is sitting. The patient’s legs uncrossed, feet flat on floor, with palms upwards. The patient should be in a comfortable upright position and their wrists supported. |
 |
| Figure 5.2Positioning of the practitioner taking the pulse when the patient is supine. Note that the patient’s arm is by their side and the wrist is supported for maximal access to the artery. |
A folded towel or small cushion can be used to support the wrist if necessary in either the supine or sitting positions. This ensures that the radial artery is easily accessible and that the blood flow is unimpeded. Additionally, such support limits any movement in the wrist that maybe introduced by the practitioner when applying finger pressure to assess the pulse at different levels of depth.
5.1.1. Speaking
Ideally there should be no speaking between the practitioner and patient during the pulse assessment process. When the patient speaks this will change their respiration, position of the diaphragm and oxygen requirements, also changing the pulse contour and pulse rate.
When the practitioner speaks during the pulse assessment, this often is a sign that they are not focused on the assessment process. Occasionally, speaking is required and is usually done in response to further elucidation of any pulse findings. For example, the presence of missed beats requires further questioning to determine whether the patient was aware of this. This should be kept to relevant questions if concurrently assessing the pulse.
Once the patient and wrist region are appropriately positioned, the next step is to locate the artery, andin particular, the radial pulse sites used for pulse examination. As described in Chapter 2, the radial artery is located on the lateral portion of the anterior forearm. It extends from the elbow, where the brachial artery bifurcates, to the wrist crease, at which point the radial divides further into other arterial segments. (When seen from the perspective of channel physiology, the radial artery follows the course of the Lung channel.) The CM pulse sites used for pulse assessment are located in the wrist portion of the artery only. At this region, the radial artery is usually quite easily palpated because of its close proximity to the skin surface and its position over a hard surface — in this case the radial bone. The radial bone provides a firm support to the radial artery when external pressure is applied. If there were no support then it would be difficult to clearly distinguish the pulse parameters or apply different levels of pressure without the artery moving.
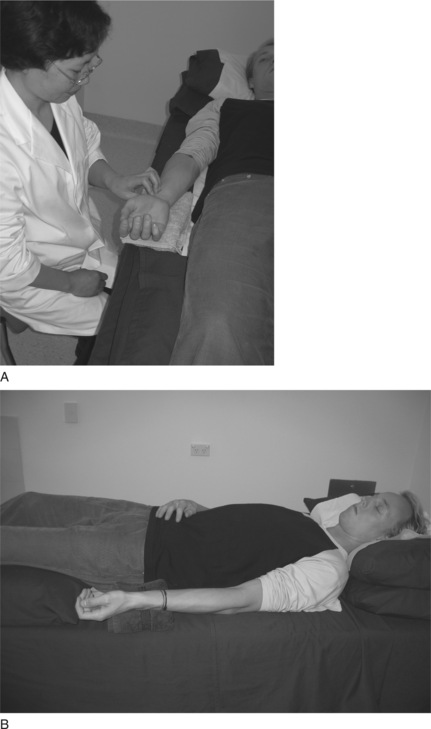
The portion of the radial pulse used for assessment is located proximal to the wrist crease directly above the pulsation of the radial artery adjacent to the styloid process of the radius. This is known as the Cun Kou pulse, and from the time of the Nan Jing it was considered to be the convergence point of movement through all the conduit vessels. The Second Difficult Issue in the Nan Jing discusses the length of the Cun Kou position, describing it as 1.9 Cun in length. Proportionally, this is about one sixth of the area between the transverse elbow crease and the wrist crease, assuming the length of the forearm is 12 Cun (or anatomical units) (see Fig. 5.3). In metric measurement this is approximately 3–5 cm. However, exact measurements are not necessarily applied because locating the pulse positions primarily depends on the location of the styloid process and the relative size of the patient.
 |
| Figure 5.3Styloid process, the radial artery and location of the three pulse positions Cun, Guan and Chi and other related anatomical structures. The Cun (inch) measurements indicate the portion of the artery used for pulse assessment. |
5.2.1. Deviated artery: abnormalities of the radial artery
In a small percentage of people the radial artery is anatomically deviated from the anterior to the lateral portion of the arm as it nears the wrist. In these individuals the artery winds laterally around the styloid process and travels on the posterior side of the wrist (in the anatomical position) as if following the path of the Large Intestine channel through the anatomical snuffbox rather than the path of the Lung channel. This is termed a Fan Guan Mai or simply a ‘pulse on the back of the wrist’ pulse by Wiseman & Ye (1998: p. 473, p. 470).
5.2.2. When to look for a deviated radial artery
If the pulse appears to be absent or extremely faint, look for the presence of a pulsation on the posterior or lateral part of the wrist, in the vicinity of the radial styloid process. If there is a significant pulsation, this indicates a deviated radial artery. In this case, the radial artery runs very superficially and both the artery and pulsations can be easily observed. When the artery is located at this region, the pulse cannot be used for palpation purposes except for assessing rate and rhythm.
A deviated arterial artery is not considered pathological from either a CM or a biomedical perspective. Such deviations represent normal individual variation. However, if the pulsation is not felt in the Cun Kou area or an alternative position, then this may be perceived as pathological. The Cun Kou area should be re-examined, with particular attention to the deep level of depth.
5.2.3. Other abnormalities
Other ‘abnormalities’ that can similarly affect the presentation of the arterial pulsation include:
• Ganglions
• Bone spurs and growths
• Surgical procedures for carpal tunnel syndrome rearranging soft tissue structures
• Other surgical procedures for arthritis in which carpal bones can be removed
• Scarring, especially keloid tissue
• Inflammatory conditions of the tendons.
5.3. Locating the pulse positions for assessment
Once the Cun Kou region of the artery proximal to the wrist is located, the pulse positions used for pulse assessment must be identified. There are three of these positions, and they are found by dividing the Cun Kou region into three portions using the styloid process of the radius as a guide. The three positions are:
• Cun (inch): Located proximal (or closest) to the wrist crease
• Guan (bar): Located medial to the styloid process of the radius
• Chi (cubit): Most distal (furthermost) position from wrist crease.
Because the three pulse positions are determined proportionally according to an individual’s size, this means that the same procedure needs to be followed every time to ensure exact location of these positions within the same physique and between different physiques (Box 5.2). Of the three positions Cun, Guan and Chi, it is the central position Guan which is associated with a specific surface anatomical landmark; the styloid process. For this reason, the Guan position should always be located first as the locations of the Cun and Chi positions depend on the initial location of Guan.
Box 5.2
Locating the three positions
• Index finger is placed at the Cun position
• Middle finger is placed at the Guan position
• Ringer finger is placed at the Chi position
• Thumb is placed on the underside of the wrist
5.3.1. Locating Guan
The Guan position is found first as it is easily located adjacent to the styloid process of the radius. The styloid process is a flaring of the radial bone, and can be identified as a bony protuberance on the lateral side of the wrist, proximal to the wrist crease (in the anatomical position). To locate the styloid process it is best to palpate the bone as it is not always easy to identify this landmark by observation alone. By gently running the index finger over the region a distinct ‘bump’ can be felt where the styloid process flares away from the shaft of the radius. The styloid process can also be clearer to palpate with radial/ulnar deviation, causing the soft tissue to stretch and expose the bone. Once it is located, the practitioner moves directly medial towards the soft skin of the anterior wrist above the radial artery. The arterial pulsations are often felt most distinctly in this position, and the outer border of the styloid process may be felt at the margin of the finger when positioned on the artery. This is the Guan position. When the middle finger is placed on the Guan position, the other two fingers should fall naturally into their positions: the index finger on Cun, located adjacent to the scaphoid bone, and the ring finger on Chi, proximal to Guan.
The actual finger placement is proportional to the size of the wrist: on a tall person the wrist is larger, and so the three positions and fingers are spaced further apart. Conversely, on a shorter person the wrist is proportionally smaller and so the three fingers are positioned closer together. However, for all patients the positioning of the fingers on the pulse should always be undertaken in reference to the styloid process and the location of the Guan position. Using either the Cun or the Chi position for this purpose will lead to incorrect placement of the fingers. (This doesn’t work with children.)
With the practitioner’s thumb resting lightly on the back of the patient’s wrist the fingers should be arranged so that the tips are level with one another. It is the tips of the fingers which should be used for palpation, exerting equal pressure to feel the three pulse positions simultaneously. The fingers can be used:
• Simultaneously to palpate all three pulse positions on one arm
• For comparative purposes, assessing the overall pulse in one side with the other
• Individually to assess pulse positions at different levels of depth.
5.3.2. Placement of the thumb
In the process of placing the fingers on the appropriate pulse positions and undertaking assessment, the thumb is of particular importance. The thumb is used to stabilise the wrist against movement that may occur when different pressures are applied by the fingers to the pulse. If the patient’s wrist moves during palpation this will render the reliability of the findings questionable. For example, if a particular amount of strength is used to move the fingers into the deep level of depth, but the wrist is unsupported, then the wrist may move so that rather than palpating the deep level the practitioner may assess only the middle level of depth without realising this is the case. For this reason, the thumb is placed on the posterior wrist region to provide support to the wrist and leverage for the fingers when palpating the pulse.
5.3.3. The anatomy of the radius and support of the radial artery
Because of the shape of the radial bone and the depression formed between it and the styloid process, the support provided by the styloid to the radial artery at the wrist varies. For example, at the Guan position the pulse wave and arterial structure are both felt more distinctly than at the Cun or Chi position alone. Because of the support offered by the styloid bone at the Guan position, the artery sits relatively superficial. Less skin, and thinner epidermal/fasciae layers, mean a ‘clearer’ pulse image when palpating and facilitates better detection of arterial parameters such as tension.
At the Chi position the radial bone sinks away from the surface with the artery similarly becoming deeper. In order to detect pulses clearly it is often necessary to provide support under the artery. Having the artery supported means it can be compressed and so the pulse is detectable for diagnostic purposes. If no support is provided then the artery and pulses remain indistinct. For this reason palpation of the Chi positions often results in a pulse that is felt deeper or less strongly when compared to the pulse at the Guan positions. It is only after pressure is applied and the artery is supported by the bone that the pulse is felt distinctly. Sometimes the direction of finger pressure needs to be adjusted to ensure that the artery is being compressed into a firm surface, such as the tendons located medially to the radial artery. (This may account for the traditional description of the pulse at this position, the Kidney pulse, being located like a ‘pebble at the bottom of a stream’ or described as ‘insects crawling around the bone’.)
The Cun pulse positions are in a depression between two bony structures. These structures are the styloid process and the scaphoid bone. For this reason, the pulse and artery are less supported at the Cun position than at the Guan position, but are felt more distinctly than the Chi positions because of the stabilisation offered to the artery by these bones. However, as at the Chi position, the lack of direct underlying support under the cun positions often means the pulse and artery are not felt as distinctly at the Guan position, but are not as deeply located as the Chi position.
When taking the pulse the practitioner should sit opposite or next to the patient. Using the tips of the fingers (Box 5.3), the practitioner’s left hand is used to feel the pulses of the patient’s right hand and the practitioner’s right hand is used to feel the pulses on the patient’s left (Box 5.4). Similarly, if the practitioner were to palpate their own pulses on the right wrist, the practitioner’s left hand wraps under the wrist with the index, middle and ring fingers sequentially falling on the three pulse positions Cun, Guan and Chi. This is reversed if feeling the left hand pulses. This ensures that the same fingers are always used to palate the same pulse positions (Fig. 5.4). For example, the right index finger is always placed on the left Cun position, irrespective of whether the practitioner is palpating someone else’s pulse or their own. This will assist in ensuring that a level of sensitivity and a reference range of pulses are built up for that particular finger and this in turn assists with reliable identification and assessment of any changes in the pulse parameters at the related pulse site.
Box 5.3
Fingertips and fingernails
• The fingertips are the most sensitive regions of the finger. Individuals who play the guitar will find that the skin thickens at the tips of the fingers and for this reason, sensitivity to the pulse is often substantially lessened, if not absent. In such instances the finger pads rather than the tips should be used for assessing the pulse.
• The length of the fingernails can also prevent the use of the fingertips for pulse assessment. In such circumstances, the finger pads can be used or the nails regularly trimmed.
Box 5.4
• The fingers of the right hand are used to palpate the left wrist pulse.
• The fingers of the left hand are used to palpate the right wrist pulse.
5.5. Assessing the parameters
Once the pulse positions are located, the fingers are moved in different directions and depths to assess the pulse wave and the anatomy of the arterial wall at each of the positions. In particular, discrete increments of pressure are applied by the fingers to feel the three levels of pulse depth. The fingers are also moved from side to side to assess the width and tension of the arterial wall, and longitudinally to assess pulse length. Of the three movements, depth assessment is particularly important in CM, as each pulse site can be further divided into different levels of depth with each level theoretically reflecting a different region of the body.
Assessment of pulse depth is discussed in greater detail below, and this requires a specific technique to locate the levels of depth. Lateral and longitude assessment of the pulse are respectively discussed in Chapter 6 in the section on assessing the pulse parameter length and in Chapter 7 in relation to assessment of the pulse parameter arterial wall tension.
5.5.1. Relevance of the different pulse positions
In CM, each of the three pulse positions is used to assess the overall pulse, as is done in biomedical practice, but each of the three positions is also viewed as reflecting a specific function or region of the body. Because of this, the pulse at each position is sometimes viewed as three distinctly different pulses, in spite of the three pulse positions being located on the same arterial segment and with the same blood flowing through them. The Cun positions are often ascribed to the upper region of the torso, the thoracic cavity, and changes in the pulse specifically at these two positions (the left and right Cun) indicate dysfunction of this region. Similarly, the Guan and Chi positions are ascribed respectively to the abdominal and pelvic cavities and the pulses are said to infer the function of these regions. The thoracic, abdominal and pelvic cavities are termed the upper, middle and lower Heaters (or Jiao) respectively. The pulse positions Cun, Guan and Chi also are simultaneously assigned to different channels, organs or regions of the body depending on the system used for interpreting the pulse information. In this sense then, the left Cun position for example is associated with the Heart and Small Intestine channel, the anatomical region of the chest, as well as reflecting the upper Jiao when paired with the right Cun position (Fig. 5.5). Besides associating each position to specific organ and channel entities, the three pulse positions are used for assessing the overall pulse qualities. These qualities include specific changes in the pulse wave and arterial structure that often occur across the three positions and are used to infer the nature of an illness and the effect it is having on the body.
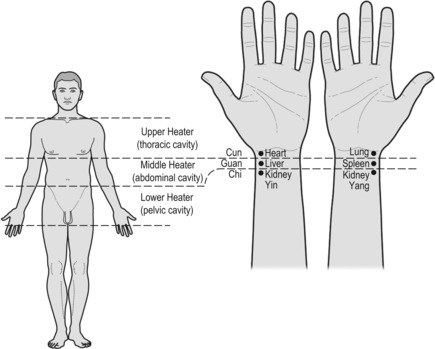 |
| Figure 5.5Association of the three pulse positions to the three regions of the body and their relationship to the organs. |
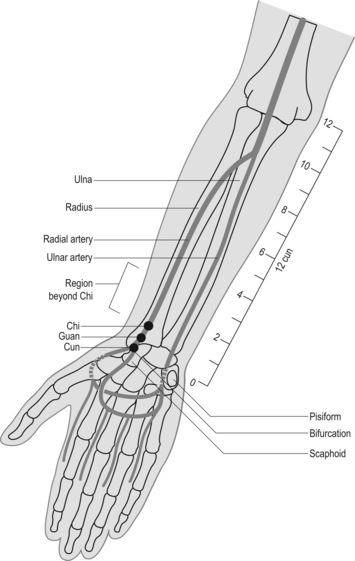
A consistent technique for correct location of the levels of depth is just as important in pulse diagnosis as correct anatomical location of the Cun, Guan and Chi pulse positions. Each pulse/position site can be further divided into two levels (superficial and deep) of depth or three (superficial, middle and deep), depending on the theoretical CM model used. For example, in Five Phase pulse diagnosis, only the superficial and deep levels of depth are assessed (Fig. 5.6). In determining overall pulse qualities as presented in the Mai Jing and Bin Hue Mai Xue, three levels of depth are often required for pulse assessment. There are even systems of pulse assessment based on the writings of the Nan Jing that palpate up to five levels of depth, and other systems state up to eight levels of depth (Hammer 2001), but these systems are not widely used. There are three commonly used levels of depth: superficial, middle and deep.
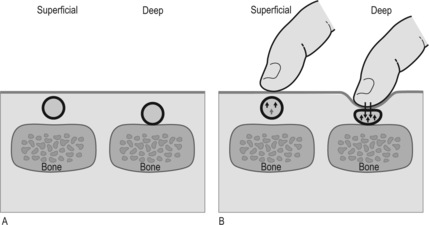 |
| Figure 5.6Radial artery, the pulse and assessment of pulse depth. The pulse depth relates to either the physical presence of the artery situated superficially or deep (A) or can be classified by the degree of finger pressure required to feel the strongest pulsation between the three levels of depth (B). Two examples are shown. One where the pulse is strongest at the superficial level of depth the other where the pulse is felt strongest at the deep level of depth. |
The parameter of pulse depth may be interpreted in two ways. Firstly, it refers to the level of depth where the radial arterial pulsation is found to be the strongest, regardless of the overall intensity of the pulsation. That is, we need to determine the relative strength of each level of depth. An integral part of determining pulse depth involves examination of the effect on radial pulsation of differing amounts of pressure exerted on the radial artery.
Secondly, pulse depth can refer to the level of depth at which the radial artery is physically located. This may be the result of anatomical structural variations within the subcutaneous layer of tissue overlying the radial artery, or the anatomical variations in the musculature and tendinous insertions around the forearm and wrist area. Diagnostically, the level of depth may be affected by pathological processes occurring within the body, resulting in either a pulse that can be felt strongest at the superficial or deep level of depth, or perhaps equally strong at all three levels of depth. Other factors affecting where the pulse can be felt include the strength of cardiac contraction.
5.6.1. Locating the three levels of depth
The three levels of depth should always be examined during pulse taking to determine the level at which the pulsations are strongest overall. This process is repeated as many times as necessary to correctly identify the strongest level. This is achieved by using consistent pressure across all three fingers to palpate to each of the three levels of depth; the superficial level of depth initially, followed by the deep and then middle levels of depth. Pulses at the three depths are found as follows.
• Deep: This level of depth is found by occluding the radial artery (pressing the artery firmly against the radial bone) and then releasing the pressure gently until the pulse can be felt again. (The Mai Jing states ‘press to the bone and then release the pressure’ to feel this level of depth; alternatively, the pressure required is greater than the weight of 12 soybeans (Wang, Yang trans 1997).) This approach creates an initial rush in the blood flow when pressure is released slightly after occluding the pulse. A few seconds should be allowed to enable the pulse to equalise before assessment. It is important to take care not to release so much pressure as to move the fingers into the middle level of depth (Fig. 5.7).
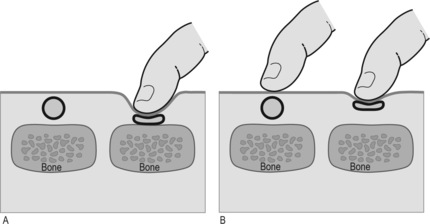 |
| Figure 5.7Compression of the artery by finger pressure to assess the ease of pulse occlusion. In (A) compression of the artery occurs only when heavy pressure is applied by the finger, where the bone provides a stabllising support against which to occlude the artery. In (B) the artery is easily compressed at a more superficial level because of the lack of arterial pressure due to vacuity (deficiency) patterns of Qi or Blood. |
Note: With some pulses it may seem extremely difficult to occlude the artery, with the pulse still felt beyond Chi. When this occurs, it is not a failure to occlude the pulse but rather it is the continuing presence of pulse waves moving from the heart to the periphery and hitting into the side of the palpating finger. When pulses are detected on the side of the finger during pulse occlusion, this is usually a sign of strength in the pulse. Whether the pulse strength reflects health or illness requires further assessment. When enough pressure is applied to stop movement of the pulse under the fingers then the pulse is considered to be occluded whether or not the pulse continues to be felt at the side of the ring finger.
• Middle: This level of depth is found by applying a moderate pressure to the radial artery (not sufficient to occlude it), somewhere between superficial and deep. It is detected by exerting more pressure than required to palpate the superficial level but not enough to occlude the pulse. The middle level is located after initially locating the superficial and deep levels, which are found first in order to ascertain the amount of pressure required to palpate to the middle level. This level is an estimate of the halfway point between the two pulse depth extremes.
The order of finding the levels of depth is important to ensure that assessment is occurring at the correct level of depth. It is relatively easy to observe whether assessment is occurring at the superficial level of depth but difficult to locate the middle level of depth, located at the ‘halfway mark’, without first knowing the degree of strength required to find the deep level. As the pulse taker moves from the superficial level to deeper within the pulse, believing that they are at the deep level of depth, they may in fact only be in the middle level of depth. This can occur because no baseline has been established to give a context to both the middle and deeper levels of depth.
5.6.2. Defining a pulse by the level of depth
Different pulses are often described as being felt strongest at a particular level of depth. When a pulse is described as being located at the deep level of depth this can mean one of two things:
• The pulse is felt strongest at this level of depth; it may still be felt with less finger pressure at the other levels of depth, superficial and middle, it is just less strong
• The pulse cannot be felt at middle or superficial and only felt at the deep level of depth.
In these scenarios, the level of depth of a pulse is the level at which the pulse is felt strongest. Several pulse qualities are defined or identified in this manner. For example, the Floating pulse is defined by the fact that it is felt strongest at the superficial level of depth and sequentially less at the other levels of depth when finger pressure is increased. In this way the Floating pulse is determined not only by the presence at the superficial level of depth but also by its diminishing strength at deeper levels. With other pulse qualities, too, it is both the presence of strength at one level of depth and the absence of strength or a detectable pulse at another level of depth that is used for identifying that particular pulse. Another example is the Scallion Stalk (Hollow) pulse which is also felt strongest at the superficial level of depth and is absent at the middle and deep level of depth when further finger pressure is applied. (Note, however, that for the Scallion Stalk pulse other parameters in addition to depth assessment are of equal importance in defining the pulse.) The level of depth where the pulse is felt strongest is also often the level of depth where the arterial wall and pulse contour are clearly felt as well.
5.6.3. Diagnostic meaning of the levels of depth
5.6.3.1. Superficial and deep level of depth
In a CM context a pulse felt strongest at the superficial level of depth is broadly categorised Yang and a pulse felt strongest at the deep level of depth is categorised Yin. When the fingers move from the superficial to the deep level of depth, so the pulse progressively moves from reflecting Yang to reflecting Yin. This is reversed when palpating from the deep to the superficial levels of depth, when the pulse progressively reflects Yang.
If the pulse is viewed from an anatomical or pressure wave perspective, then the superficial pulse indicates an artery located near the skin surface or a pulse with sufficient force for the flow wave to expand the blood vessel. A pulse felt strongest at the deep level of depth can also indicate either an artery obscured by the skin and overlying tissue, or an artery with insufficient support, or simply a pulse that is strongest at the deep level. This may reflect a poor pulse force, which does not allow the flow wave to expand the vessel; and this may be due to a poor heart function or dilution of pulse strength through other factors such as arterial dilatation (see Chapter 2). The vessel wall can also constrict or be compressed by the surrounding connective tissue, restricting clear expansion of the pulse wave. From these examples, it can be seen that probably a number of different mechanisms are involved in the formation of a deep pulse. However, irrespective of why a deep pulse occurs, a pulse felt strongest at the deep level of depth is broadly categorised as Yin. The Eight Principles (Ba Gang) approach to pulse assessment in particular categorises pulse in this way, categorising a pulse as either Yin or Yang.
5.6.3.2. Meaning of the middle level of depth
Located between the deep and superficial levels of depth, the middle level of depth can be viewed from a CM perspective as the point of interchange between Yin and Yang, the fluxing between the two ‘poles’ of form (deep level) and function (superficial level) (Box 5.5). When the pulse is felt strongest at the middle level of depth this is viewed as a sign of balance between Yang or function (Qi) and the interplay with Yin or form (Blood). The middle level of depth is where the pulse should be felt strongest on most individuals. When the pulse is felt strongest only at the superficial or only at the deep levels of depth then this more than likely reflects ill health, dysfunction or maybe a prognostic sign inferring ill health. In this scenario, a pulse occurring strongest at the superficial level of depth reflects Yang-type illnesses or conditions that have caused Yang to become hyperactive. This is seen in cases of febrile conditions producing delirium, or in conditions with dream-filled restless sleep. Similarly, a pulse occurring strongest at the deep level of depth reflects Yin-type illnesses or conditions that have constrained or depleted the Yang, causing the pulse to contract into the deeper regions of the artery. Yin conditions often involve organ dysfunction.
Box 5.5
• Superficial level of depth reflects Yang: exterior
• Deep level of depth reflects Yin: interior
• Middle level of depth reflects the balanced interplay between Qi (function) and Blood (form)
In their simplest form, the overall CM pulse qualities in the literature are used in this context, identifying the nature and location of an illness, whether Yin or Yang. In this way, the superficial level of depth reflects the Yang, the middle level of depth the action of Qi with Blood, and the deep level of depth the organs/Yin.
5.6.3.3. Combining depth assessment with the other parameters
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


