To investigate gender differences in lipid goal attainment, we conducted a retrospective analysis of outpatient electronic health records from a large cardiology practice from September 2008 to September 2009. The most recent lipid profile and lipid-lowering medications and doses were extracted from electronic medical record. We identified 9,950 patients with coronary artery disease of whom 3,366 (34%) were women. Women were less likely to achieve a low-density lipoprotein (LDL) cholesterol goal of <70 mg/dl compared with men (30.6% vs 38.4%, p <0.001) and less likely to achieve a non–high-density lipoprotein cholesterol goal of <100 mg/dl (37.1% vs 48.2%, p <0.001). Irrespective of age, women were less likely to achieve their LDL cholesterol goals. Compared with men, women were more likely to be on no statin (16.9% vs 11.6%, p <0.001) or any lipid-lowering therapy (12.8% vs 7.8%, p <0.001) and less likely to be on high-potency statin (14.9% vs 18.0%, p <0.001) or combination therapy (22.2% vs 30.1%, p <0.001). There exists a major difference in the use of lipid-lowering therapy between men and women with coronary artery disease. In conclusion, women with coronary artery disease are prescribed insufficient doses of statins and combination lipid-lowering therapy and are less likely to achieve their optimal LDL and non–high-density lipoprotein cholesterol goals.
The purpose of this study was to investigate gender differences in optimal lipid goal attainment in patients with coronary artery disease, in a community practice setting.
Methods
The study site was Cardiology Consultants of Philadelphia, a large cardiology subspecialty practice in the Philadelphia area. Using an electronic health record (EHR), we identified 23,408 patients with a history of coronary artery disease who had been seen in 1 of 18 outpatient offices over a 12-month period from September 2008 to September 2009. Patients were excluded if they did not have a complete lipid panel within the EHR flow sheet or had not been seen in the office at least once within the study period. In patients with >1 complete lipid panel, the most recent lipid panel was used. We identified 9,950 patients with coronary artery disease who met the study criteria. Age, gender, history of current cigarette smoking, type 2 diabetes, hypertension, current lipid-lowering medications and doses, and patient and physician demographics were extracted from the EHR. Median annual household income was based on residence zip codes from data from the United States Census. The Institutional Review Board of Drexel University College of Medicine approved the study.
The primary outcome measures were the percent of patients who achieved a low-density lipoprotein (LDL) cholesterol goal of <70 mg/dl and a non–high-density lipoprotein cholesterol goal of <100 mg/dl. Statin potency was categorized as low, moderate, or high. High-potency statins included atorvastatin (40 or 80 mg), rosuvastatin (20 or 40 mg), or simvastatin (80 mg). Moderate-potency statins included atorvastatin (10 or 20 mg), rosuvastatin (10 mg), simvastatin (40 mg), lovastatin (80 mg), or pravastatin (80 mg). All other doses were considered as low-potency statins. Nonstatin lipid-lowering drugs were also documented, including ezetimibe, bile acid sequestrants, prescription formulation omega-3 polyunsaturated fatty acids, fibrates, and niacin compounds. Combination therapy was defined as any statin plus a nonstatin lipid-lowering drug.
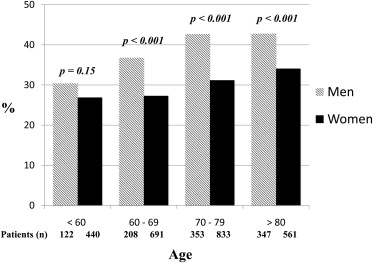
Characteristics of the study participants are described using means and standard deviations or median and interquartile range for continuous variables, and the number (%) for categorical data. Independent t testing or Wilcoxon nonparametric test for continuous variables and chi-square test for categorical variables analyzed comparisons between men and women. Each lipid-lowering therapy was assessed independently, so that men and women were compared for each particular therapy. Odds of achieving the LDL cholesterol goal of <70 mg/dl for various lipid-lowering therapies were assessed using logistic regression. Logistic regression was executed on the total group and then stratified by gender (separately for men and women). This model was adjusted for age, diabetic status, and provider. A multinomial logistic regression model was used to assess the odds of being on each individual therapy for women versus men. This model was adjusted for age, diabetes, obesity, median income, LDL cholesterol level at the time of the study, and provider. When analyzing for age, patients were divided into the following age groups: age <60, 60 to 69, 70 to 79, and ≥80 years.
Results
There were 3,366 women and 6,584 men in the study population ( Table 1 ). Women were less likely to achieve an LDL cholesterol goal of <70 mg/dl compared with men (30.6% vs 38.4%, p <0.001) and less likely to achieve a non–high-density lipoprotein cholesterol goal of <100 mg/dl (37.1% vs 48.2%, p <0.001). Women were older than men, had more hypertension, and had similar rates of diabetes, smoking, and obesity. Irrespective of age, women were less likely to achieve their LDL cholesterol goals ( Figure 1 ). Women were more likely to be treated by a younger aged cardiologist, a female cardiologist, and a clinical cardiologist compared with men. Women were also more likely to be treated at an urban practice site compared with men.
| Variable | Overall (n = 9,950) | Women (n = 3,366) | Men (n = 6,584) | p Value |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age (yrs) | 70.6 ± 11.5 | 73.2 ± 11.3 | 69.4 ± 11.4 | <0.001 |
| Current smoker | 859 (8.6) | 287 (8.5) | 572 (8.7) | 0.79 |
| Hypertension | 6,669 (67.0) | 2,490 (74.0) | 4,179 (63.5) | <0.001 |
| Diabetes mellitus | 2,650 (26.6) | 904 (26.9) | 1,746 (26.5) | 0.72 |
| BMI >30 kg/m 2 | 4,644 (46.9) | 1,574 (47.0) | 3,070 (46.8) | 0.87 |
| Insurance provider | ||||
| Commercial | 3,787 (38.1) | 1,342 (39.9) | 2,445 (37.1) | 0.008 |
| Medicare | 5,691 (57.2) | 1,839 (54.6) | 3,852 (58.5) | <0.001 |
| Medicaid | 347 (3.5) | 134 (4.0) | 213 (3.2) | 0.06 |
| None | 125 (1.3) | 51 (1.5) | 74 (1.1) | 0.10 |
| Median income ∗ | 54 (39–62) | 53 (37–61) | 57 (43–62) | <0.001 |
| LDL cholesterol <70 mg/dl | 3,555 (35.7) | 1,030 (30.6) | 2,525 (38.4) | <0.001 |
| Non-HDL cholesterol <100 mg/dl | 4,422 (44.4) | 1,249 (37.1) | 3,173 (48.2) | <0.001 |
| LDL cholesterol (mg/dl) | 82.0 ± 29.2 | 87.8 ± 33.0 | 79.1 ± 26.5 | <0.001 |
| HDL cholesterol (mg/dl) | 48.8 ± 14.1 | 55.0 ± 15.7 | 45.6 ± 12.0 | <0.001 |
| Triglycerides (mg/dl) | 132.9 ± 64.2 | 136.7 ± 62.8 | 131.0 ± 64.9 | <0.001 |
| Non-HDL cholesterol (mg/dl) | 108.6 ± 33.4 | 115.2 ± 36.9 | 105.2± 30.9 | <0.001 |
| Physician characteristics | ||||
| Age >50 yrs | 7,892 (79.3) | 2,558 (76.0) | 5,334 (81.0) | <0.001 |
| Women | 893 (9.0) | 465 (13.8) | 428 (6.5) | <0.001 |
| Clinical cardiologist | 8,181 (82.2) | 2,852 (84.7) | 5,329 (80.9) | <0.001 |
| Interventional cardiologist | 1,769 (17.8) | 514 (15.3) | 1,255 (19.1) | <0.001 |
| Community hospital affiliation | 6,141 (61.7) | 2,107 (62.6) | 4,034 (61.3) | 0.20 |
| Tertiary care hospital affiliation | 3,809 (38.3) | 1,259 (37.4) | 2,550 (38.7) | 0.20 |
| Urban office location | 2,714 (27.3) | 1,001 (29.7) | 1,713 (26.0) | <0.001 |
| Suburban office location | 7,236 (72.7) | 2,365 (70.3) | 4,871 (74.0) | <0.001 |
Women were more likely not to be treated with a statin (16.9% vs 11.6%, p <0.001) and more likely to be on no lipid-lowering therapy at all (12.8% vs 7.8%, p <0.001) compared with men ( Table 2 ). In patients treated with a statin alone, women were more likely to be on a low-potency statin and less likely to be on a high-potency statin. This finding that women were more likely to treated with a lower potency statin compared with men persisted when patients on a statin in combination with another lipid-lowering drug were included in the analysis. Women were also less likely to be treated with a statin in combination with another lipid-lowering drug (22.2% vs 30.1%, p <0.001) compared with men. This finding was primarily driven by less use of fibrates and niacin in women compared with men. The use of ezetimibe was similar in men and women. The number of patients on a bile acid sequestrant or prescription omega-3 polyunsaturated fatty acids was very low.
| Lipid-Lowering Medication | Overall (n = 9,950) | Women (n = 3,366) | Men (n = 6,584) | p Value |
|---|---|---|---|---|
| Statin monotherapy | 5,885 (59.1) | 2,049 (60.9) | 3,836 (58.3) | 0.01 |
| High potency | 1,691 (17.0) | 503 (14.9) | 1,188 (18.0) | <0.001 |
| Moderate potency | 2,326 (23.4) | 794 (23.6) | 1,532 (23.3) | 0.72 |
| Low potency | 1,868 (18.8) | 752 (22.3) | 1,116 (17.0) | <0.001 |
| Combination therapy | 2,730 (27.4) | 747 (22.2) | 1,983 (30.1) | <0.001 |
| No statin | 1,335 (13.4) | 570 (16.9) | 765 (11.6) | <0.001 |
| No lipid-lowering therapy | 946 (9.5) | 431 (12.8) | 515 (7.8) | <0.001 |
| Other lipid-lowering drugs | ||||
| Ezetimibe | 1,564 (15.7) | 538 (16.0) | 1,026 (15.6) | 0.60 |
| Niacin | 1,036 (10.4) | 162 (4.8) | 874 (13.3) | <0.001 |
| Fibrates | 885 (8.9) | 258 (7.7) | 627 (9.5) | 0.002 |
| Bile acid sequestrant | 85 (0.9) | 38 (1.1) | 47 (0.7) | 0.03 |
| Prescription omega-3 PUFA | 83 (0.8) | 23 (0.7) | 60 (0.9) | 0.24 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


