Previous studies have suggested that women may be at higher risk of death after ST-segment elevation myocardial infarction (STEMI). We studied potential associations of gender and age with in-hospital mortality using a registry of 31,689 consecutive patients with STEMI aged ≥30 years (66.3% men, mean age 67.8 years) treated in 22 hospitals. Total in-hospital mortality rate of STEMI was 11.2%. Women had higher unadjusted mortality rate compared with men (17.5% vs 8.0%; hazard ratio 1.65; 95% confidence interval [CI] 1.54 to 1.76, p <0.0001). However, when adjusted for age and co-morbidities, there was no difference in mortality between genders overall (hazard ratio 1.04; 95% CI 0.97 to 1.12, p = 0.2303) or at any age group. Mortality rate was highly dependent of age with an estimated increase of 86% (95% CI 80% to 92%) per 10-year increase in age (p <0.0001). Chronic coronary, peripheral, or cerebral artery disease, diabetes, renal insufficiency, malignancy, and severe infection were independent predictors of mortality in multivariate analysis. Atrial fibrillation was associated with survival in multivariate model. Anterior location of STEMI was not independently associated with in-hospital mortality. In conclusion, although women have higher total in-hospital mortality rate than men after STEMI, this difference does not appear to be caused by gender itself but to be due to of differences in age and co-morbidities.
Despite evolving treatments and shortening delays of reperfusion therapy, ST-segment elevation myocardial infarction (STEMI) still causes significant mortality. Presentation and complications of STEMI differ between genders because of yet unclear mechanisms. Previous studies have resulted in conflicting results on potential gender difference in mortality after STEMI. A number of studies have suggested women to be at higher risk of death after STEMI, whereas others have found no mortality difference between genders. Potential gender effect may be age dependent as women in the youngest age groups have been reported to have highest mortality excess compared with men. To further clarify the possible gender bias in STEMI mortality, we studied associations of gender and age with in-hospital mortality using a large-scale multihospital registry data.
Methods
Study population included 31,689 consecutive patients aged ≥30 years admitted to a participating hospital who had STEMI ( International Classification of Disease, Tenth Revision [ ICD-10 ] codes I21.0x, I21.1x, I21.2x, or I21.3x) as primary discharged diagnosis. Data were collected from all 22 Finnish hospitals with angiolaboratory using the Finnish Hospital Discharge Register, a nationwide database maintained by the Finnish National Institute for Health and Welfare. Admissions starting from April 29, 2000, to November 29, 2009, were included. The study was conducted according to the National Institute for Health and Welfare permission THL/1576/5.05.00/2010.
Categorical variables are presented as counts or percentages with 95% confidence interval (CI) as appropriate. Scale variables are presented as mean ± SD. In-hospital mortality was studied using the Cox regression model with exact method for failure time ties. Multivariate mortality model included patient characteristics associated with mortality at the level of p <0.05 in univariate analysis. Variables displayed in Table 1 in addition to age, study year, and gender were considered as potential predictors of in-hospital mortality. To control for potential interhospital differences, survival analyses were stratified by treating hospital. Gender differences in baseline characteristics were studied with log-binomial regression models adjusted for age and study year. Results of regression analyses are presented as hazard ratios (HRs) or relative risks; p values <0.05 were considered statistically significant. Statistical analyses were performed with the SAS System, version 9.3 (SAS Institute Inc., Cary, North Carolina).
| Occurrence | Women vs. men ∗ | ||||
|---|---|---|---|---|---|
| Total (n=31,689) | Women (n=10,668) | Men (n=21,021) | Relative risk (CI) | p | |
| Anterior STEMI | 16,377 (51.7%) | 5,786 (54.2%) | 10,591 (50.4%) | 1.03 (1.01-1.06) | 0.0055 |
| Chronic coronary artery disease | 4,423 (14.0%) | 1,418 (13.3%) | 3,005 (14.3%) | 0.87 (0.82-0.92) | <0.0001 |
| Heart failure | 2,887 (9.1%) | 1,330 (12.5%) | 1,557 (7.4%) | 1.23 (1.14-1.32) | <0.0001 |
| Diabetes | 2,285 (7.2%) | 889 (8.3%) | 1,396 (6.6%) | 1.23 (1.13-1.34) | <0.0001 |
| Atrial fibrillation | 1,419 (4.5%) | 651 (6.1%) | 768 (3.7%) | 1.07 (0.96-1.19) | 0.2050 |
| Septicemia or pneumonia | 926 (2.9%) | 345 (3.2%) | 581 (2.8%) | 0.77 (0.67-0.89) | 0.0003 |
| Peripheral or neurovascular disease | 647 (2.0%) | 270 (2.5%) | 377 (1.8%) | 1.04 (0.88-1.22) | 0.6562 |
| Chronic pulmonary disease | 586 (1.8%) | 185 (1.7%) | 401 (1.9%) | 0.69 (0.57-0.83) | <0.0001 |
| Ventricular arrhythmia | 476 (1.5%) | 99 (0.9%) | 377 (1.8%) | 0.62 (0.49-0.78) | <0.0001 |
| Malignancy | 295 (0.9%) | 95 (0.9%) | 200 (1.0%) | 0.66 (0.51-0.86) | 0.0018 |
| Systemic connective tissue disease † | 189 (0.6%) | 107 (1.0%) | 82 (0.4%) | 2.35 (1.72-3.19) | <0.0001 |
| Renal insufficiency | 185 (0.6%) | 66 (0.6%) | 119 (0.6%) | 0.74 (0.54-1.02) | 0.0674 |
∗ Adjusted for age and study year.
Results
Majority of the patients were men (66.3%; 95% CI 65.5% to 67.3%). The mean age was 67.8 years (SD 12.9, range 30 to 102). Male patients were significantly younger (64.7 ± 12.4 years) than female patients (74.2 ± 11.7 years), p <0.0001. Average duration of admission for STEMI was 6.8 ± 5.2 days. Co-morbidities of patients are listed in Table 1 . Women with STEMI had heart failure, diabetes, and systemic connective tissue disease more frequently than men ( Table 1 ). Chronic coronary artery and pulmonary diseases, severe infection, renal insufficiency, ventricular arrhythmias, and malignancy were, however, more common in men ( Table 1 ).
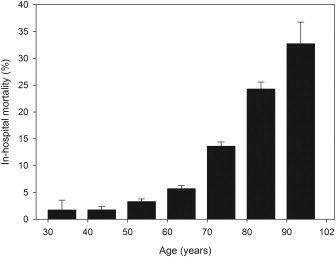
Overall in-hospital mortality rate of STEMI was 11.2% (95% CI 10.8% to 11.6%). Associations of patient features and co-morbidities with in-hospital mortality are listed in Table 2 . Mortality rate was highly dependent of age ( Figure 1 ), with an estimated gender and co-morbidity–adjusted increase of 86% (80% to 92%) per 10-year increase in age (p <0.0001). Women had higher unadjusted mortality rate compared with men (17.5%, 95% CI 16.7% to 18.4%, vs 8.0%, 95% CI 7.6% to 8.4%, respectively; HR 1.65, 95% CI 1.54 to 1.76; p <0.0001). However, when adjusted for age and co-morbidities ( Table 2 ), there was no difference in mortality between genders (HR 1.04, 95% CI 0.97 to 1.12; p = 0.2303). Furthermore, there was no gender-based difference in mortality at any age after adjustment for co-morbidities ( Figure 2 ). Known chronic atherosclerotic disease in either coronary, peripheral, or cerebral arteries was associated with death in both univariate and multivariate ( Table 2 ) analyses. Diabetes, renal insufficiency, malignant disease, and severe infection (septicemia or pneumonia) were also independently associated with in-hospital mortality ( Table 2 ). In contrast, atrial fibrillation (AF) predicted in-hospital survival in STEMI. Anterior location of STEMI was associated with mortality only in univariate analysis but was not an independent predictor of death in multivariate analysis. In-hospital mortality in STEMI reduced by estimated 3.8% (95% CI 2.6% to 5.0%) per year during 2000 to 2009 (p <0.0001).
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Hazard ratio (CI) | p | Hazard ratio (CI) | p | |
| Female gender | 1.65 (1.54-1.76) | <0.0001 | 1.04 (0.97-1.12) | 0.2303 |
| Age / 10-year increase | 1.86 (1.81-1.92) | <0.0001 | 1.86 (1.80-1.92) | <0.0001 |
| Chronic coronary artery disease | 2.82 (2.62-3.04) | <0.0001 | 2.84 (2.64-3.07) | <0.0001 |
| Peripheral or neurovascular disease | 2.17 (1.85-2.53) | <0.0001 | 1.93 (1.65-2.25) | <0.0001 |
| Diabetes | 1.15 (1.02-1.29) | 0.0186 | 1.24 (1.10-1.40) | 0.0003 |
| Renal insufficiency | 2.20 (1.70-2.85) | <0.0001 | 1.83 (1.41-2.37) | <0.0001 |
| Malignancy | 1.81 (1.43-2.30) | <0.0001 | 1.76 (1.38-2.23) | <0.0001 |
| Septicemia or pneumonia | 1.44 (1.25-1.65) | <0.0001 | 1.20 (1.04-1.38) | 0.0107 |
| Chronic pulmonary disease | 1.25 (1.02-1.55) | 0.0353 | 1.14 (0.92-1.41) | 0.2250 |
| Anterior STEMI | 1.09 (1.02-1.17) | 0.0083 | 1.02 (0.95-1.09) | 0.6007 |
| Atrial fibrillation | 0.60 (0.49-0.71) | <0.0001 | 0.47 (0.39-0.56) | <0.0001 |