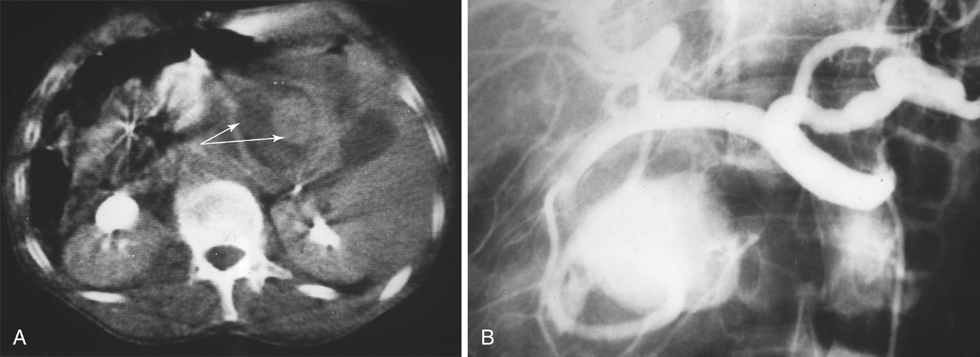
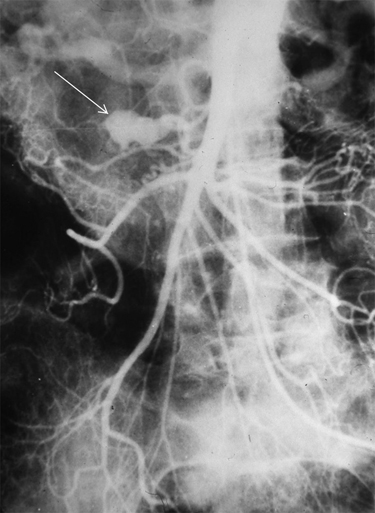
Approximately 50% of gastroduodenal and 30% of pancreaticoduodenal artery aneurysms are related to pancreatitis (Figures 1 and 2). Pseudoaneurysms of these arteries are most often a consequence of pancreatitis. Mechanisms of aneurysmal formation in this setting include acute or subacute vascular disruption by activated pancreatic enzymes and later chronic pseudocyst erosion into an adjacent artery. Traumatic aneurysms, especially as a result of iatrogenic injury associated with hepatobiliary and pancreatic operations, are uncommon, but when they do occur they most often involve the gastroduodenal artery. Septic emboli are a rare cause of pseudoaneurysms affecting these peripancreatic arteries.
Gastroduodenal and Pancreaticoduodenal Artery Aneurysms
Pseudoaneurysms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


