Coronary artery bypass grafting (CABG) is commonly performed to treat ischemic heart disease, but long-term benefits are limited by failed patency of bypass grafts. Both statin medications and aspirin hold class I indications for all post-CABG patients and should be continued indefinitely unless contraindications exist. Unfortunately, there are limited data regarding long-term usage of these essential medications. We assessed the utilization rates of statins and aspirin among post-CABG patients referred for coronary angiography. Analysis of post-CABG patients presenting to Thomas Jefferson University for a cardiac catheterization procedure at least 3 years after surgery was performed. Inpatient and outpatient records were reviewed to assess prescribing patterns of these medications, as well as other pertinent clinical and laboratory data. The study population was 381 consecutive patients presenting at a mean of 11 ± 6 years from CABG. Mean age was 69 ± 11 years and 78% were men. A total 67% of patients were being prescribed a statin, whereas 75% were prescribed aspirin. Only 52% were prescribed both at the time of catheterization. Patients prescribed a statin had a significantly lower mean low-density lipoprotein (87 vs 106 [p <0.01]) and total cholesterol values (151 vs 162 [p <0.01]). A total of 35% of patients had low-density lipoprotein ≥100. Only 43% of saphenous vein grafts in the patients not on statin medications remained patent. In conclusion, long-term statin and aspirin use after CABG remains suboptimal despite clear guideline recommendations and clinical trial evidence of their effectiveness.
Coronary artery bypass grafting (CABG) remains an effective and essential therapy for ischemic heart disease. The long-term benefits, however, are limited by high rates of bypass graft stenosis and occlusion. The beneficial effects of statins and aspirin usage after CABG have been demonstrated by numerous trials. In the recently published American Heart Association scientific statement on secondary prevention after CABG surgery, the long-term use of statins and aspirin are class Ia indications. Although many randomized trials have focused on the effects of drug therapies on early postoperative graft patency, few studies have examined the utilization of these proven therapies in the longer term clinical setting. Accordingly, the present study was undertaken to assess the frequencies of statin and aspirin use in a consecutive series of patients who were referred for repeat cardiac catheterization after previous CABG.
Methods
We performed a retrospective analysis of the medical and electronic records in 381 consecutive patients with a history of previous CABG surgery who underwent a diagnostic cardiac catheterization at Thomas Jefferson University Hospital for the first time since their CABG. Patients were identified through the cardiac catheterization laboratory database. Data obtained included age, gender, a history of CABG, medical co-morbidities, smoking status, current medications (including statins and antiplatelet drugs), indication for catheterization, lipid panel, glomerular filtration rate and angiographic findings of the cardiac catheterization. Angiographic analysis defined graft status as patent (<50% stenosis), diseased (50% to 99% stenosis), and occluded (100% stenosis) based on visual estimation. Exclusion criteria constituted patients with CABG <3 years before the index cardiac catheterization, absence of a lipid panel within 30 days before or 7 days after the index cardiac catheterization, and incomplete diagnosis of graft status by cardiac catheterization. The Institutional Review Board of Thomas Jefferson University Hospital approved this study.
Continuous variables are presented as mean ± SD and were analyzed using factorial analysis of variance. Categorical variables are displayed as a percentage and were compared using chi-square statistics. We compared outcome variables between patients grouped by their overall status of grafted vessels and groups of grafted vessels. Statistical analysis was performed using SPSS software, version 19 (IBM, Armonk, NY). A p value <0.05 was considered significant.
Results
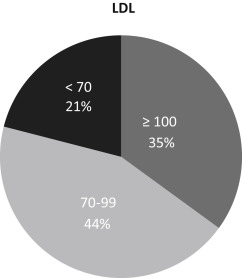
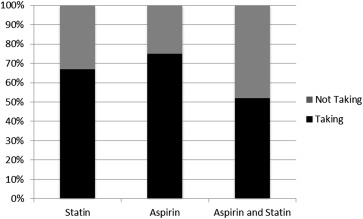
Baseline clinical characteristics are depicted in Table 1 . The mean age of the study population was 69 ± 11 years; 78% of patients were men and 43% were diabetic. The median CABG age was 11 ± 6 years; there were an average of 2.9 grafts per patient, with 67% of the grafts being saphenous vein grafts (SVGs). Indications for catheterization included unstable angina (37%), non–ST elevation myocardial infarction (26%), and abnormal stress test (13%; Table 1 ). Lipid analysis revealed a mean low-density lipoprotein (LDL) of 94 ± 36 mg/dl; 35% of patients had LDL values ≥100 mg/dl and only 21% had LDL <70 mg/dl ( Figure 1 ). Utilization rates of statins and aspirin are shown in Figure 2 . At the time of the catheterization, 67% of patients were taking a statin and 75% were taking aspirin ( Figure 2 ). Only 52% of patients were taking both aspirin and a statin. A total of 21% were taking both clopidogrel in addition to aspirin. Patient characteristics based on statin and aspirin status are presented in Tables 2 and 3 , respectively. The mean total cholesterol and LDL values were significantly lower in the patients on statin therapy ( Figure 3 and Table 2 ). Those not on statin therapy were more likely to have LDL values ≥100 mg/dl (53% vs 26%, p <0.001; Table 2 ).
| Variable | Mean ± SD or % |
|---|---|
| Age (years) | 69 ± 11 |
| Men | 297 (78%) |
| Diabetes mellitus | 164 (43%) |
| Hypertension | 282 (74%) |
| Current Smoker | 53 (14%) |
| Years Since Coronary Bypass | 11 ± 6 |
| Total Cholesterol (mg/dL) | 156 ± 43 |
| Low Density Lipoprotein (mg/dL) | 94 ± 36 |
| High Density Lipoprotein (mg/dL) | 37 ± 11 |
| Triglyceride (mg/dL) | 134 ± 89 |
| Glomerular Filtration Rate (mL/min/1.73 m 2 ) | 62 ± 23 |
| Statin Use | 255 (67%) |
| High Intensity | 59 (23%) |
| Moderate Intensity | 174 (68%) |
| Low Intensity | 22 (9%) |
| Prior Intolerance to Statin | 11 (3%) |
| Aspirin Use | 286 (75%) |
| Clopidogrel Use | 80 (21%) |
| Warfarin Use | 51 (13%) |
| Clinical Indication for Cardiac Catheterization | |
| ST-elevation Myocardial Infarction | 19 (5%) |
| Non-ST-elevation Myocardial Infarction | 100 (26%) |
| Unstable Angina Pectoris | 141 (37%) |
| Chronic Angina Pectoris | 36 (9%) |
| Abnormal Stress Test | 50 (13%) |
| Heart Failure | 30 (8%) |
| Aortic Valve Disease | 5 (1%) |
| Clinical Characteristic | Statin Use | ρ Value | |
|---|---|---|---|
| Yes (n=255) | No (n=126) | ||
| Mean Age (Years) | 69 ± 10 | 71 ± 9 | 0.265 |
| Men | 199 (78%) | 101 (80%) | 0.681 |
| Acute Coronary Syndrome | 161 (63%) | 69 (55%) | 0.175 |
| Diabetes mellitus | 120 (47%) | 47 (37%) | 0.127 |
| Hypertension | 194 (76%) | 88 (70%) | 0.276 |
| Tobacco use | 33 (13%) | 20 (16%) | 0.412 |
| Aspirin | 198 (78%) | 91 (72%) | 0.267 |
| Dual Antiplatelet Therapy ∗ | 91 (24%) | 20 (16%) | 0.150 |
| Mean Total Cholesterol (mg/dL) | 151 ± 35 | 162 ± 49 | 0.024 |
| Mean Low Density Lipoprotein (mg/dL) | 87 ± 28 | 106 ± 40 | <0.001 |
| Mean High Density Lipoprotein (mg/dL) | 37 ± 11 | 34 ± 11 | 0.091 |
| Mean Triglyceride (mg/dL) | 134 ± 80 | 118 ± 73 | 0.107 |
| Low Density Lipoprotein ≥100 (mg/dL) | 66 (26%) | 67 (53%) | <0.001 |
| Glomerular Filtration Rate (mL/min/1.73 m 2 ) | 62 ± 23 | 59 ± 26 | 0.398 |
| Percutaneous Coronary Intervention | 150 (59%) | 66 (52%) | 0.215 |
| Repeat CABG surgery | 8 (3%) | 4 (3%) | 0.632 |
| No Revascularization | 97 (38%) | 57 (45%) | 0.224 |
| Clinical Characteristic | Aspirin Use | ρ Value | |
|---|---|---|---|
| Yes (n=286) | No (n=95) | ||
| Mean Age (Years) | 70 ± 10 | 70 ± 9 | 0.868 |
| Men | 226 (79%) | 75 (79%) | 0.957 |
| Acute Coronary Syndrome | 174 (61%) | 56 (59%) | 0.873 |
| Diabetes mellitus | 126 (44%) | 41 (43%) | 0.906 |
| Hypertension | 215 (75%) | 66 (69%) | 0.320 |
| Tobacco use | 37 (13%) | 16 (17%) | 0.347 |
| Statin Use | 198 (69%) | 57 (60%) | 0.165 |
| Clopidogrel Use | 66 (23%) | 15 (16%) | 0.195 |
| Warfarin Use | 29 (10%) | 30 (32%) | 0.001 |
| Mean Total Cholesterol (mg/dL) | 155 ± 41 | 153 ± 38 | 0.620 |
| Mean Low Density Lipoprotein (mg/dL) | 93 ± 35 | 92 ± 31 | 0.776 |
| Mean High Density Lipoprotein (mg/dL) | 36 ± 12 | 35 ± 10 | 0.404 |
| Mean Triglyceride (mg/dL) | 130 ± 90 | 133 ± 78 | 0.800 |
| Low Density Lipoprotein ≥100 mg/dL | 103 (36%) | 29 (31%) | 0.517 |
| Glomerular Filtration Rate (mL/min/1.73 m 2 ) | 62 ± 24 | 57 ± 24 | 0.131 |
| Percutaneous Coronary Intervention | 166 (58%) | 49 (52%) | 0.334 |
| Repeat CABG | 9 (3%) | 3 (3%) | 0.611 |
| No Revascularization | 112 (39%) | 43 (45%) | 0.361 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


