Methamphetamine is one of the most commonly abused illegal drugs in the United States. Health care providers are commonly faced with medical illness caused by methamphetamine. This study investigates the impact of methamphetamine use on the severity of cardiomyopathy and heart failure in young adults. This retrospective study analyzed patients seen at Arrowhead Regional Medical Center from 2008 to 2012. Patients were between 18 and 50 years old. All patients had a discharge diagnosis of cardiomyopathy or heart failure. The severity of disease was quantified by left ventricular systolic dysfunction: heart failure with preserved ejection fraction to mildly reduced if ejection fraction was >40% and moderate to severely depressed if ejection fraction was ≤40%. Methamphetamine abuse was determined by a positive urine drug screen or per documented history. Of the 590 patients, 223 (37.8%) had a history of methamphetamine use. More than half the population was men (n = 389, 62.3%); 41% was Hispanic (n = 243), 25.8% was Caucasian (n = 152), and 27.8% was African-American (n = 164); 60.9% were in the age range of 41 to 50 years (n = 359). Patients with a history of methamphetamine use had increased odds (odds ratio = 1.80, 95% confidence interval 1.27 to 2.57) of having a moderately or severely reduced ejection fraction. Additionally, men were more likely (odds ratio 3.13, 95% confidence interval 2.14 to 4.56) to have worse left ventricular systolic dysfunction. In conclusion, methamphetamine use was associated with an increased severity of cardiomyopathy in young adults.
Although there are extensive published reports on the cardiovascular pathophysiology, psychological effects, and behavioral effects of methamphetamine use, there is limited evidence pertaining to the development of early heart failure among users. We investigate the association of methamphetamine use and a diagnosis of cardiomyopathy or heart failure in adults ≤50 years. To our knowledge, this is the largest clinical study investigating this association. A previous study described this association in native Hawaiian and Pacific Islander populations and showed methamphetamine use to be an independent risk factor for cardiomyopathy or heart failure. The ethnic demographics for that study population was largely limited by geography.
This study includes a large sample size and a diverse demographic in an urban tertiary care center located in San Bernardino County, California.
Methods
This study was approved by the Institutional Review Board at the Arrowhead Regional Medical Center (ARMC) and was a retrospective chart review study. ARMC is a 456-bed acute care teaching facility and one of the 2 American College of Surgeons–certified level II trauma centers located in San Bernardino County, California. San Bernardino County is the largest county in the contiguous United States and has an estimated population of 2,091,618 in 2014. The predominant ethnicity is Latino at 51%. Among non-Latino residents, 31% are white, 8% are African-American, 7% are Asian or Pacific Islander, and 3% reported as ≥2 races or American Indian/Alaska Native or other.
Emergency department patients seen at ARMC from January 2008 to December 2012 were analyzed for inclusion in this study. Patients were selected from both genders and all ethnicities. Patients were included if they were 18 to 50 years old and had a discharge diagnosis of cardiomyopathy or heart failure. International Classification of Diseases, Ninth Revision ( ICD-9 ) codes were used to select patients with a diagnosis of cardiomyopathy ( ICD-9 : 425.2 to 425.9) or heart failure ( ICD-9 : 428.0 to 428.9). Methamphetamine use was determined by a positive urine drug screen or by documentation in the patient’s chart by the physician. Patients with a history of coronary artery disease or valvular heart disease were excluded from the multivariate logistic regression. Among women, patients who were suspected to have peripartum cardiomyopathy were excluded regardless of methamphetamine use. For patients with multiple admissions, only data from the initial visit were recorded and repeat hospitalizations were excluded.
The primary outcome was the severity of LV systolic dysfunction as characterized by ejection fraction (EF) reduction. For study purposes, EF reduction severity, as determined by an echocardiogram, was categorized as follows: heart failure with preserved ejection fraction (HFpEF) to mildly reduced EF >40% and moderately to severely reduced EF ≤40%. Selection of ≤40% as a baseline for clinically significant LV systolic dysfunction was based on its predictive value of cardiovascular outcome and indication for specific treatment protocols.
Analyzed predictors included age, ethnicity, methamphetamine use, tobacco use, alcohol use, cocaine use, marijuana use, diabetes, hypertension, and dyslipidemia. Ethnicity was further categorized into 4 groups: Hispanic, Caucasian, African-American, and other. Substance use history and the presence of diabetes, hypertension, and dyslipidemia were obtained through chart review.
All data were analyzed using the SAS software for Windows, version 9.3 (Cary, North Carolina). Descriptive statistics were presented as frequencies and proportions for categorical variables. A chi-square crosstab analysis was conducted to assess the association between predictors and severity of EF reduction (mild vs moderate to severe). A logistic regression was conducted using PROC LOGISTIC to identify factors associated with the severity of EF reduction (mildly vs moderately to severely reduced EF). The possible predictor included in the logistic regression included all the significant variables identified by the crosstab analysis. All statistical analyses were 2 sided; p value <0.05 was considered statistically significant.
Results
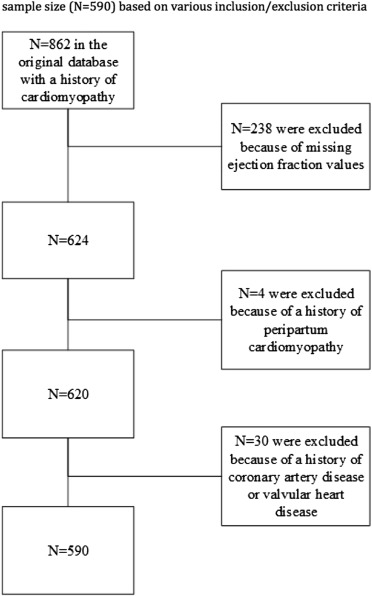
A total of 862 patients with a discharge diagnosis of cardiomyopathy or heart failure were identified and assessed for inclusion in the study. Patients who lacked a noted EF in their chart (n = 238), who had a history of peripartum cardiomyopathy (n = 4), and who had a history of CAD or valvular heart disease (n = 30) were excluded; 590 patients were included in the final analysis ( Figure 1 for patients flow chart). The demographic information is presented in Table 1 . More than half the population were men (61%); they were Hispanic (41%), Caucasian (26%), or African-American (27%) and within the age range of 41 to 50 (61%).
| Variable | Frequency (N=590) | Percent |
|---|---|---|
| Female | 228 | (39%) |
| Male | 362 | (61%) |
| Black | 164 | (28%) |
| Hispanic | 242 | (41%) |
| Other | 32 | (5%) |
| White | 152 | (26%) |
| Age (years) | ||
| 18-30 | 57 | (10%) |
| 31-40 | 174 | (30%) |
| 41-50 | 359 | (61%) |
| Methamphetamine Use | 223 | (38%) |
| Tobacco Use | 313 | (53%) |
| Alcohol Use | 254 | (43%) |
| Cocaine Use | 50 | (9%) |
| Marijuana Use | 98 | (17%) |
| Diabetes Mellitus | 216 | (37%) |
| Hypertension | 452 | (77%) |
| Dyslipidemia | 255 | (43%) |
| Ejection Fraction | ||
| >40% | 367 | (62%) |
| ≤40% | 223 | (38%) |
Of the 590 patients, 223 had associated methamphetamine use, which represented 38% of our study population. There was a significant correlation between the prevalence of methamphetamine use and ethnicity ( Table 2 ). Patients aged 41 to 50 years were the most likely to use methamphetamine. Men were more likely than women to use methamphetamine. More than half (61%) of the Caucasians in the study population were methamphetamine users, followed by Hispanics and African-Americans.
| Variable | Methamphetamine Use | P-value | |
|---|---|---|---|
| No (n=367) | Yes (n=223) | ||
| Age (years) | 0.0667 | ||
| 18-30 | 38 (67%) | 19 (33%) | |
| 31-40 | 119 (68%) | 55 (32%) | |
| 41-50 | 210 (59%) | 149 (42%) | |
| 0.2815 | |||
| Female | 148 (65%) | 80 (35%) | |
| Male | 219 (61%) | 143 (40%) | |
| <.0001 | |||
| Black | 128 (78%) | 36 (22%) | |
| Hispanic | 153 (63%) | 89 (37%) | |
| Other | 27 (84%) | 5 (16%) | |
| White | 59 (39%) | 93 (61%) | |
∗ The total row percentage may not add up to 100% due to rounding.
Table 3 presents the analysis of various factors associated with the severity of cardiomyopathy among these patients. Patients with a history of methamphetamine use were at a greater risk of having a moderate to severely reduced EF (47% vs 32%, p = 0.0006). Additionally, men were more likely to have moderate to severely reduced EF compared with women (48% vs 22%, p <0.0001). Tobacco users in comparison with non-tobacco users had a moderate to severely reduced EF (44% vs 31%, p = 0.0026). Other factors, including ethnicity, age, alcohol use, cocaine use, marijuana use, diabetes, hypertension, and dyslipidemia, were not statistically significantly associated with EF severity among the cardiomyopathy patients.
| Variable | Left Ventricular Ejection Fraction | P-value | |
|---|---|---|---|
| >40% (n=367) | ≤40% (n=223) | ||
| <.0001 | |||
| Female | 177 (78%) | 51 (22%) | |
| Male | 190 (53%) | 172 (48%) | |
| 0.8295 | |||
| Black | 98 (60%) | 66 (40%) | |
| Hispanic | 155 (64%) | 87 (36%) | |
| Other | 19 (59%) | 13 (41%) | |
| White | 95 (63%) | 57 (38%) | |
| Age (years) | 0.2925 | ||
| 18-30 | 30 (53%) | 27 (47%) | |
| 31-40 | 110 (63%) | 64 (37%) | |
| 41-50 | 227 (63%) | 132 (37%) | |
| Methamphetamine Use | 119 (53%) | 104 (47%) | 0.0006 |
| Tobacco Use | 177 (57%) | 136 (44%) | 0.0026 |
| Alcohol Use | 151 (60%) | 103 (41%) | 0.2302 |
| Cocaine Use | 31 (62%) | 19 (38%) | 0.9753 |
| Marijuana Use | 58 (59%) | 40 (41%) | 0.4996 |
| Diabetes Mellitus | 131 (61%) | 85 (39%) | 0.5538 |
| Hypertension | 285 (63%) | 167 (37%) | 0.4411 |
| Dyslipidemia | 163 (64%) | 92 (36%) | 0.4527 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


