Follicular Bronchiolitis and Lymphoid Interstitial Pneumonia
Allen P. Burke, M.D.
Fabio R. Tavora, M.D., Ph.D.
Seth Kligerman, M.D.
Overview and Terminology
Follicular bronchiolitis and lymphoid interstitial pneumonia (LIP) are part of a spectrum of related inflammatory lung conditions, the former emphasizing airway and the latter, interstitial localization. Nodular lymphoid hyperplasia, inflammatory pseudotumor, Castleman disease, and IgG4-related disease in the lung are considered related entities.1
The term “lymphoid interstitial pneumonia” originates in the 1960s, with Liebow’s classification of interstitial pneumonias (see Chapter 16), whereas “follicular bronchiolitis” is somewhat more recent, with the first series published in the 1980s.2 Histologic features of both entities overlap, with the predominant pattern (bronchiolar vs. interstitial) dictating the proper designation.3 In fact, “LIP” is now considered rare4 and is even considered by some to be an obsolete term.5 The predisposing conditions to both entities are presented in Tables 36.1 and 36.2.
Follicular bronchiolitis is a reactive B-cell proliferation centered on small airways, and “LIP” is a diffuse interstitial process with a typical cystic appearance on chest CT scans.6 Both conditions are associated with immunodeficiency and autoimmune disorders and often overlap. However, peribronchiolar inflammation with germinal centers (the histologic definition of follicular bronchiolitis) may have a variety of causes and is seen as a minor histologic component in diverse diseases, whereas LIP is a more homogeneous clinicopathologic entity closely associated with autoimmune disorders (especially Sjögren disease) and HIV/AIDS.
Follicular Bronchiolitis
Clinical Features
From the time of Yousem et al.’s initial series in the 1980s, it was apparent that follicular bronchiolitis, as seen on lung biopsies, formed three clinicopathologic entities.2 The largest group was that associated with autoimmune collagen vascular disease, especially rheumatoid arthritis and Sjögren syndrome. A second important group comprised patients with inherited immunodeficiency syndromes. The third group is heterogeneous and includes hypersensitivity and infectious conditions causing reactive lymphoid hyperplasia in the small airways.2 In the largest recent series of biopsy-documented follicular bronchiolitis, 2 of 12 patients had connective tissue disorders (Sjögren syndrome and undifferentiated connective-tissue disease (CTD), respectively), two had common variable immunodeficiency (CVID) syndrome, and the remaining two-thirds had no apparent underlying condition.3 The latter finding highlights the nonspecificity of reactive follicles surrounding airways in biopsies of patients with clinically heterogeneous processes. Follicular bronchiolitis has also been described in patients with HIV,7 although the interstitial inflammatory component is typically emphasized in association with HIV (LIP).
TABLE 36.1 Conditions Associated with Lymphoid Interstitial Pneumonia | |||||
|---|---|---|---|---|---|
|
Clinically, patients typically have frequent pulmonary infections. Most patients have some degree of dyspnea and cough, and abnormal chest radiographs are common. Bronchoscopic findings are usually nondiagnostic. Respiratory function tests show variable results, but a restrictive pattern may be present. By CT scan, nodular or micronodular lung densities with prominent, thickened distal airways, often with areas of ground-glass opacities or consolidation, are present.3
Microscopic Findings
Follicular bronchiolitis is largely a descriptive diagnosis. By definition, only distal cartilaginous bronchi and bronchioles are involved; reactive hyperplasia around more proximal bronchiectatic airways or follicular lymphoid hyperplasia in the context of prominent acute or necrotizing inflammation is not considered follicular bronchiolitis.
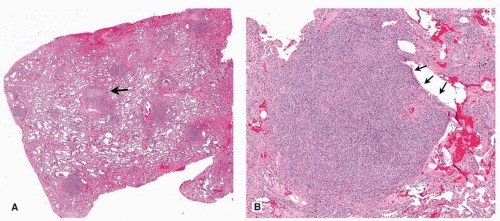
Histologically, follicular bronchiolitis is characterized by lymphoid follicular hyperplasia of small airways, often with reactive germinal centers that may coalesce (Figs. 36.1, 36.2, 36.3).2 Other findings and diagnoses may be present, depending on the clinical setting, including emphysema, respiratory bronchiolitis, carcinoid tumors, and granulomas.3 In general, acute inflammation is minimal, unless there is superimposed infection.
Differential Diagnosis
Lymphoid follicles, typically without germinal centers, are not uncommon in diffuse interstitial lung diseases, such as usual or nonspecific interstitial pneumonia, as well as localized inflammatory processes. Lymphoid follicles may occur in proximal airways and occasionally result in masses (Figs. 36.4 and 36.5).
The major clinicopathologic entity in the differential diagnosis is LIP, which is often considered part of the same disease (see below). The most important entity in the histologic differential diagnosis is marginal zone B-cell lymphoma and nodular lymphoid hyperplasia. Although lymphoepithelial lesions are characteristic of lymphoma, they may also be seen in reactive processes (Fig. 36.6). Immunohistochemical studies and flow cytometry are required to exclude low-grade lymphoma.8 In general, lymphomas demonstrate a single or few dominant masses, in
contrast to follicular bronchiolitis, in which there is diffuse small airway involvement with a dominant lesion. Follicular bronchiolitis may occur as the pulmonary manifestation of Castleman disease.9
contrast to follicular bronchiolitis, in which there is diffuse small airway involvement with a dominant lesion. Follicular bronchiolitis may occur as the pulmonary manifestation of Castleman disease.9
TABLE 36.2 Conditions Associated with Follicular Bronchiolitis | |
|---|---|
|
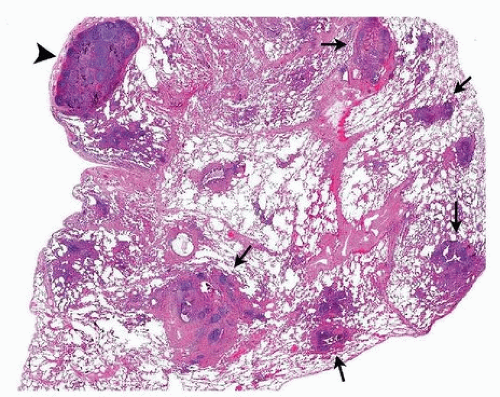 FIGURE 36.2 ▲ Follicular bronchiolitis. A low magnification demonstrates peribronchiolar lymphoid hyperplasia (arrows) and a subpleural intraparenchymal lymph node with reactive changes (arrowhead). The patient had recurrent Moraxella infection and some clinical features of immunodeficiency.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|