Focal Tracheobronchial Wall Thickening
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Mucus
Bronchial Neoplasm
Less Common
Airway Stenosis
Carcinoid
Rare but Important
Metastasis
Foreign Body
Tracheal Neoplasm
Infection
Wegener Granulomatosis
Fibrosing Mediastinitis
Broncholith
Tracheobronchial Amyloidosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Review focuses on diseases causing solitary/segmental wall thickening or nodularity
Age of patient, smoking history, and history of malignancy are important considerations
Helpful Clues for Common Diagnoses
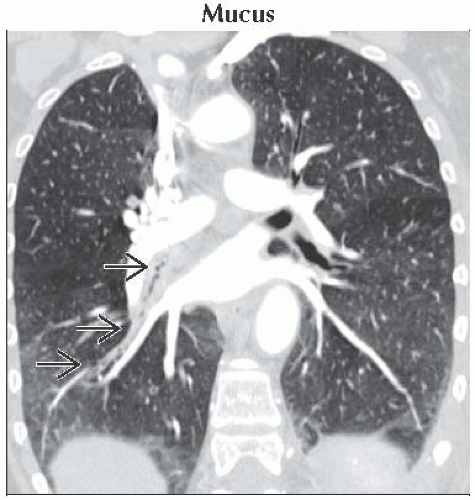
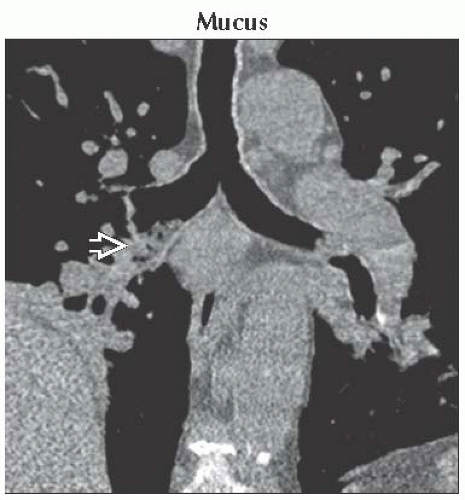
Mucus
Common in emphysema, asthma, bronchitis, or cystic fibrosis
“Bubbly” or solid appearance on CT
Gravity-dependent location
Repeat CT after vigorous coughing helpful to differentiate from tumor
Bronchial Neoplasm
Bronchogenic carcinoma
Polypoid nodule with endobronchial and extraluminal components
Postobstructive pneumonia/atelectasis
± mediastinal and hilar lymphadenopathy
± history of recurrent pneumonia
Hamartoma
Round and smooth nodule
≤ 2 cm in diameter
± internal fat
± “popcorn” calcifications
Mucoepidermoid carcinoma
Intraluminal nodule
50% of patients are ≤ 30 years old
Difficult to differentiate radiographically from carcinoid and bronchogenic carcinoma
Helpful Clues for Less Common Diagnoses
Airway Stenosis
Progressive dyspnea following extubation or tracheostomy tube placement
Focal airway narrowing with circumferential wall thickening
Hourglass appearance
Prolonged endotracheal intubation
Subglottic narrowing at balloon cuff site
Tracheostomy tube
Stenosis at stoma site
Complete cartilaginous tracheal ring is an anomaly
Sarcoidosis; look for other typical features
Carcinoid
Round or ovoid lobulated nodule
Occurs in lobar or segmental bronchi
± intense contrast enhancement
25% demonstrate chunky calcification
80% are “typical”
Benign and slow growing
Metastases and carcinoid syndrome rare
Helpful Clues for Rare Diagnoses
Metastasis
Invasion or compression from lymphoma, bronchogenic, thyroid, or esophageal carcinoma
Adjacent airway mass readily apparent
Hematogenous metastases from melanoma, breast, colon, or renal cell carcinoma
± solitary or multiple endobronchial nodules
Lymph node metastases may cause airway compression
Foreign Body
Most are radiolucent on radiographs
Easily mistaken for malignancy
History of aspiration and recurrent pneumonia
Tracheal Neoplasm
Squamous cell carcinoma
Most common primary tracheal neoplasm
33% have mediastinal or pulmonary metastases at diagnosis
40% with past, present, or future carcinoma of oropharynx, larynx, or lung
Irregular-shaped polypoid or sessile lesion
Predominates in lower trachea
Adenoid cystic carcinoma
Submucosal or circumferential wall thickening
± long tracheal segment involvement
Disease recurs locally
Metastases are rare
Infection
Tuberculosis
Distal trachea and proximal bronchi
Irregular circumferential wall thickening
Tracheal narrowing
Secondary to “endobronchial spread” or extension from involved lymph nodes
Infection rarely isolated to trachea
Histoplasmosis
Endobronchial nodule or mass
± calcified mediastinal lymph nodes
± apical cavitary nodules
Rhinoscleroma
Endemic in Central America, Africa, and India
95% have nasal polyps and soft tissue thickening
Paranasal sinuses spared
Concentric or nodular subglottic tracheal narrowing in 25%
Air-filled tracheal crypts nearly diagnostic
Wegener Granulomatosis
25% have airway involvement
Circumferential subglottic tracheal wall thickening
± luminal narrowing
± cavitary lung nodules
± pan-sinus disease
Laboratory evidence of glomerulonephritis (microscopic hematuria, red cell casts, and proteinuria)
Fibrosing Mediastinitis
Common associations
Histoplasmosis, tuberculosis, or sarcoidosis (unilateral)
Retroperitoneal fibrosis, drugs, or autoimmune disorders (bilateral)
Mediastinal fat replaced by fibrous tissue
Encases and narrows adjacent structures
Superior vena cava, mainstem bronchi, pulmonary artery, or esophagus
± mediastinal or hilar lymph node calcification
Broncholith
Irregularly shaped calcified material within airway arising from adjacent calcified lymph node
± extraluminal air
Right middle and upper lobe bronchi
No contrast enhancement
Tracheobronchial Amyloidosis
Most common presentation is multifocal nodular deposits throughout central airways
Single submucosal nodule is extremely rare
Image Gallery
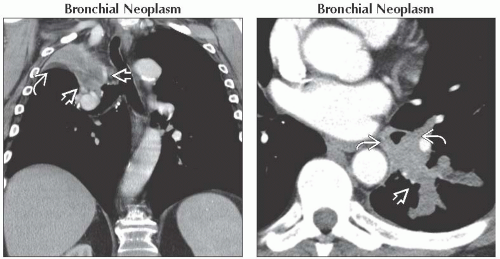 (Left) Coronal CECT shows a collapsed right upper lobe with ipsilateral tracheal deviation and occlusion of the right upper lobe bronchus by tumor
 , which has a lower density than atelectatic lung , which has a lower density than atelectatic lung  . (Right) Axial CECT shows concentric asymmetric thickening of the left lower lobe bronchus . (Right) Axial CECT shows concentric asymmetric thickening of the left lower lobe bronchus  in this patient with adenoid cystic carcinoma. Note partial collapse of a portion of the left lower lobe posterior segment in this patient with adenoid cystic carcinoma. Note partial collapse of a portion of the left lower lobe posterior segment  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|