Focal Lung Opacity
Jonathan H. Chung, MD
DIFFERENTIAL DIAGNOSIS
Common
Pneumonia
Aspiration
Pulmonary Abscess
Subsegmental Atelectasis
Lung Cancer
Metastatic Disease
Less Common
Pulmonary Hemorrhage
Radiation Pneumonitis
Progressive Massive Fibrosis
Sarcoidosis
Pulmonary Infarct
Pulmonary AVM
Rare but Important
Lymphoma
Lipoid Pneumonia
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
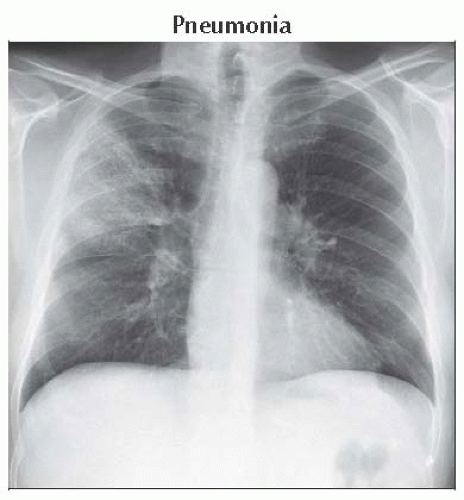
Pneumonia
Airspace opacities: Ground-glass opacity to dense consolidation
Reactive lymphadenopathy; very large lymph nodes unusual
Parapneumonic pleural effusion or empyema
Correlation with sputum, WBC count, and clinical presentation paramount
Consider fungal agents and PCP in the correct clinical setting
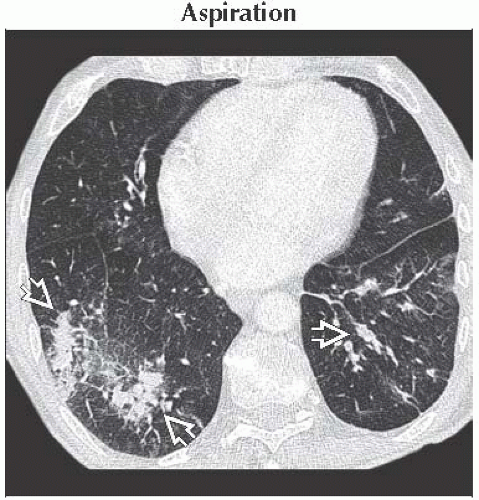
Aspiration
Consolidation in gravity-dependent portions of lungs
Predisposed patients (alcoholism, epilepsy, hiatal hernia, esophageal dysmotility or obstruction, neuromuscular disorders)
Supine: Superior segments of lower lobes and posterior segments of upper lobes
Upright: Basilar segments of lower lobes
Centrilobular or tree in bud opacities common on CT
May progress to necrotizing pneumonia or pulmonary abscess without treatment
Pulmonary Abscess
Gas-filled cavity arising from focal pneumonia (usually due to aspiration)
Abscess 1-2 weeks after development of pneumonia
Gas-fluid level or smaller foci of gas
Empyema and bronchopleural fistula
May be difficult to differentiate from empyema
Abscess: Round, thick walls, acute margins with chest wall
Empyema: Elliptical, thin walls, obtuse margins with chest wall; atelectasis of adjacent lung
Subsegmental Atelectasis
Discoid or plate-shaped
Usually in dependent aspects of lower lobes or in basilar aspects of right middle lobe or lingula
Crosses pulmonary segments
Often touches visceral pleura
Lung Cancer
Most common in upper lung zone (2/3 of primary lung cancers)
Spiculated or irregular margins; pleural tail
Thick-walled or nodular cavitation
Large hilar &/or mediastinal lymphadenopathy (> 2 cm)
Concomitant emphysema and smoking history
Metastatic Disease
Variable-sized, well-marginated pulmonary nodules preferentially in peripheral and lower lungs
Feeding artery sign: Pulmonary artery branches extend to nodules, implying hematogenous spread
Solitary metastasis: Renal cell carcinoma, colon cancer, breast cancer, sarcomas, melanoma
Helpful Clues for Less Common Diagnoses
Pulmonary Hemorrhage
Ground-glass opacities > consolidation; may be diffuse, patchy, lobular, or centrilobular
Increased interlobular and intralobular septal thickening over 1-2 days
Rapid resolution in days; not as rapid as in cardiogenic pulmonary edema or bland aspiration
Radiation Pneumonitis
Pulmonary opacities corresponding to radiation ports
Pulmonary ground-glass opacities and consolidation (radiation pneumonitis) appears 6-8 weeks after initial treatment
Radiation pneumonitis peaks 3 months after end of treatment
Evolution of pulmonary opacities into lung fibrosis from 3-18 months after end of treatment
From 18 months after end of treatment and onward lung fibrosis stable
Progressive Massive Fibrosis
Nodules from silicosis or coal worker’s pneumoconiosis coalesce into biapical mass-like consolidation, ± cavitation
Lateral margin parallels chest wall, sharply defined
Hilar and mediastinal lymphadenopathy, ± eggshell calcification
Sarcoidosis
Perilymphatic nodules with symmetric mediastinal and hilar lymphadenopathy
Small nodules may coalesce into focal opacity (alveolar sarcoidosis)
Tiny nodules around a larger dominant nodule (galaxy sign)
Interlobular septal thickening
Pulmonary Infarct
Lower lung predominant, peripheral/subpleural, wedge-shaped consolidation
In setting of acute pulmonary arterial thromboembolism
Reverse halo configuration (central ground-glass opacity and peripheral rim of consolidation)
Often in setting of superimposed cardiac dysfunction (cardiomyopathy, congestive heart failure)
Both pulmonary and bronchial arterial supply to lung reduced
Pulmonary AVM
Single or multiple nodules with feeding artery and vein
Lower and medial lungs
History of hereditary hemorrhagic telangiectasia
Helpful Clues for Rare Diagnoses
Lymphoma
Multiple ill-defined nodules that may cavitate
May occur in association with nodal disease or primarily in lungs
Lipoid Pneumonia
Exogenous aspiration of fatty material
Nodular or mass-like consolidation often with fatty CT attenuation
Fat density may not be evident because of inflammation and scarring
Irregular margins, may mimic bronchogenic carcinoma
Gravity-dependent portions of lungs
Supine: Superior segments of lower lobes and posterior segments of upper lobes
Upright: Basilar segments of lower lobes
Image Gallery
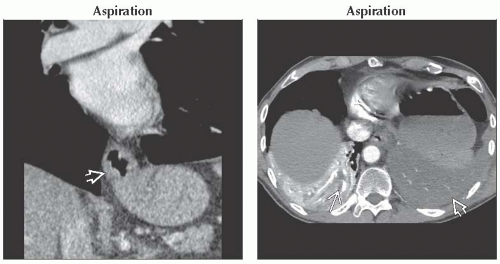 (Left) Coronal CECT shows a typical sliding-type hiatal hernia
 , which puts this patient at risk for aspiration. (Right) Axial CECT shows diffuse low density , which puts this patient at risk for aspiration. (Right) Axial CECT shows diffuse low density  within the atelectatic left lower lobe compared to the normally enhancing atelectatic right lower lobe in this patient with left lower lobe aspiration pneumonia. Tubular regions of low density within the atelectatic left lower lobe compared to the normally enhancing atelectatic right lower lobe in this patient with left lower lobe aspiration pneumonia. Tubular regions of low density  in the right lower lobe may represent aspirated material or retained secretions. in the right lower lobe may represent aspirated material or retained secretions.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|