Fig. 27.1
Necessary equipments for the pleura-videoscopy: (a) The pleura-videoscope (a rigid thoracoscope with a bidirectional flexible tip – length: 52 cm, caliber: 7.0 mm) (black arrow) and alligator jaw-type flexible biopsy forceps through the working channel (white arrows). (b) The pleura-videoscope inserted through the flexible trocar. (c) The tip of the pleura-videoscope (on the left) and a view of the working channel (2.8 mm) for biopsy forceps or suction catheter (on the right)
The sterile, disposable flexible trocar (MAJ-1058; Olympus) designed for the flexi-rigid thoracoscope is 8 mm in diameter. It is not airtight. There are two types of flexible biopsy forceps available, one without a needle (FB-36C-1; Olympus) and the other with needle between the alligator jaws (FB-55CR-1; Olympus).
27.5 Techniques
27.5.1 Thoracoscopic Procedure
The technique is described in Fig. 27.2. The flexi-rigid thoracoscopy can be performed under general anaesthesia; however, in this chapter we describe our method, the flexi-rigid thoracoscope under local anaesthesia without sedation. The procedure can be performed in the operating room, in the endoscopy suite, or at the bedside in a general ward. Patients are placed in the lateral decubitus position, involved side up. We ask patients to hold a pillow to keep their arms upward and to maintain an adequate intercostal space. The entry point is determined by ultrasonography, usually in the midaxillary line at the fifth to seventh intercostal space. The patients are premedicated with 25 mg hydroxyzine and 15 mg pentazocine given intramuscularly. Supplemental oxygen is administered via a nasal cannula, usually 3–5 l/min. Pulse, blood pressure, and oxygen saturation are continuously monitored. The patient’s skin is disinfected, and the physician and assistant clean their hands and put on a sterile gown and gloves. The physician stands on one side of the patient and the assistant is on the other side. The main operator usually faces the patient. Local anaesthesia with 10–15 ml of 1 % lidocaine is instilled to the chest wall at the previously marked site of entry. Entry into the pleural cavity is confirmed by the drawing back of fluid or air into the syringe. A 10-mm incision is made to the skin and subcutaneous tissues with a scalpel, followed by blunt dissection to the pleural space. The 8.0-mm flexible trocar should be held firmly in the palm of the hand and inserted until a release of resistance is felt. If the trocar doesn’t enter the pleural cavity easily, the physician should perform further blunt dissection. After the flexible trocar is placed, the flexi-rigid thoracoscope is inserted into the pleural cavity. Initially the physician cannot see anything clearly due to the pleural fluid. The fluid is aspirated through the working channel of the scope until the physician obtains sufficient examination space.
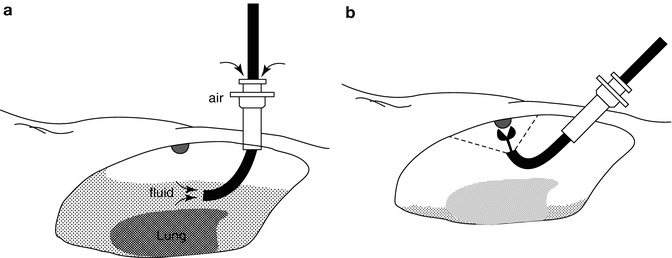
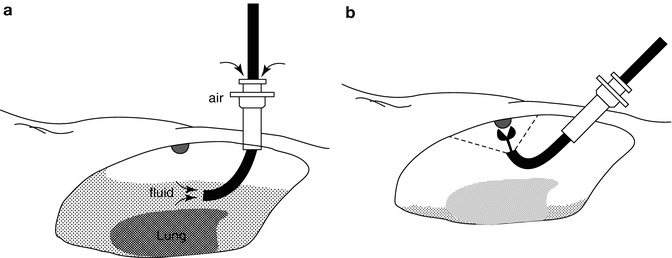
Fig. 27.2
The schema of pleura-videoscopy. (a) Pleural fluid is drained through the working channel, and atmospheric air is introduced via a trocar allowing the lung to collapse away from the chest wall. (b) Biopsy is performed through the working channel
27.5.2 Pleural Biopsy Techniques
The parietal and visceral pleura and diaphragm are carefully inspected. Biopsy specimens are obtained from suspicious-looking areas on the parietal pleura or diaphragm using flexible biopsy forceps under direct visual control. Usually 5–10 biopsy specimens are stored in 10 % formalin solution for histologic examination, and 2–4 specimens are stored in normal saline for bacteriological examination.
27.5.3 Talc Pleurodesis
After completely removing the fluid, sterile talc (Steritalc; Novatech; France) is insufflated into the pleural space through the working channel of the pleura-videoscope (Fig. 27.3) or through the 2-mm Boutin pleural puncture needle (Boutin Trocar; Novatech) placed as the second site of entry. At the end of the procedure, the distribution of the talc on the pleura is confirmed by flexi-rigid thoracoscopy.
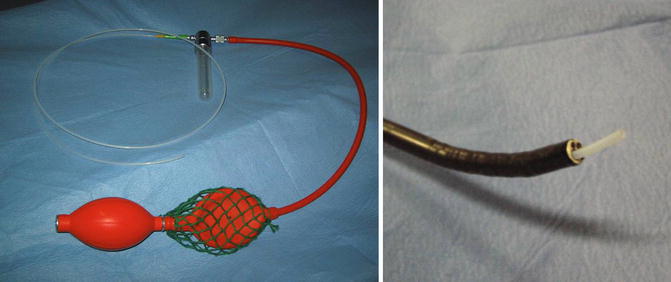
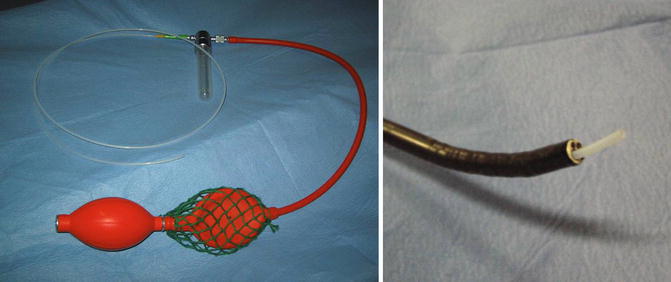
Fig. 27.3
Using a double balloon insufflator, sterile talc (Steritalc®; Novatech; France) is spread into the pleural space through the working channel of the pleura-videoscope
27.5.4 Post Procedure
After every procedure, a 20-Fr chest tube is inserted through the same incision used for the flexi-rigid thoracoscope and attached to an aspiration device. A chest roentgenogram is performed following the procedure. For pleural biopsy alone, the chest tube is removed when complete lung reexpansion is confirmed on chest roentgenogram. The chest drain can be removed on the same day. In cases where talc pleurodesis was performed, negative pressure, usually −20-cm H2O, should commence immediately after the procedure and be maintained for at least 48 h after the procedure until the fluid drainage is less than 200 ml/day.
27.6 Efficacy
The flexi-rigid thoracoscopy has been used for diagnostic purpose (Munavvar et al. 2007; Ishida et al. 2004, 2005) and talc pleurodesis (Ernst et al. 2002). The diagnostic yield of thoracoscopy using a thoracofiberscope was first reported as 81 % for malignant pleural diseases (McLean et al. 1998). The latest model, the flexi-rigid thoracoscope, provides better diagnostic yields ranging from 89 to 91 % (Munavvar et al. 2007; Ishida et al. 2004, 2005). In addition Ernst (Ernst et al. 2002) and Munavvar (Munavvar et al. 2007) have reported that the flexi-rigid thoracoscope was easy to handle and the image quality was excellent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


