Recent reports have described that hospitalizations for atrial fibrillation (AF) are continuing to increase. Given that hospitalizations are responsible for most of the economic burden associated with AF, the aim of this study was to characterize the impact of age and how changing procedural practices may be contributing to the increasing rates of AF hospitalizations. The annual age- and gender-specific incidence of hospitalizations for AF, electrical cardioversions, electrophysiologic studies, and radiofrequency ablation procedures in Australia were determined from 1993 to 2007 inclusive. Over this 15-year follow-up period spanning almost 300 million person-years, a total of 473,501 hospitalizations for AF were identified. There was a relative increase in AF hospitalizations of 203% over the study period, in contrast to an increase for all hospitalizations of only 71%. Whereas the gender-specific incidence of hospitalizations remained stable, the age-specific incidence increased significantly over the study period, particularly in older age groups. AF hospitalizations associated with electrical cardioversions decreased from 27% to 14% over the study period. Electrophysiologic studies and radiofrequency ablation procedures contributed minimally to the overall increase in AF hospitalizations observed. In conclusion, in addition to the growing prevalence of AF because of the aging population, there is an increasing age-specific incidence of hospitalizations for AF, particularly in older age groups. In contrast, changing procedural trends have contributed minimally to the increasing number of AF-associated hospitalizations. Greater attention to older patients with AF is required to develop strategies to prevent hospitalizations and contain the growing burden on health care systems.
A number of studies have suggested that the prevalence of atrial fibrillation (AF) and subsequent utilization of health care services are increasing. From a sample of hospitals in the United States, it has been estimated that hospitalizations for AF increased twofold to threefold from 1985 to 1999 and that these have been increasing more so than for any other heart rhythm disorder. European reports have likewise shown dramatic increases in the hospitalizations for AF, with Scotland also demonstrating a twofold to threefold increase between 1986 and 1996. Because most of the economic cost associated with AF is borne by hospital systems, the factors driving these trends are of paramount public health and clinical importance. We sought to explore how age and evolving interventional procedures might be contributing to the increasing rate of hospitalizations for AF.
Methods
Data were obtained from the National Hospital Morbidity Dataset, a source maintained by the Australian Institute of Health and Welfare that includes inpatient information at every hospital in Australia. The proportion of missing data is negligible, representing <0.004% of cases per year.
We identified hospitalizations with principal diagnoses of AF across a 15-year period from 1993 through 2007 inclusive. The International Classification of Diseases, Ninth Revision, Clinical Modification, and International Classification of Diseases, Tenth Revision, Australian Modification, were used for coding hospitalization diagnoses from 1993 to 1997 and from 1998 to 2007 respectively. Codes were derived from physicians’ diagnoses by trained clinical coders. AF was defined for patients with International Classification of Diseases, Ninth Revision, Clinical Modification, code 4273, and International Classification of Diseases, Tenth Revision, Australian Modification, code I48, codes that include AF and atrial flutter. We also calculated the total number of all hospitalizations for any diagnosis to characterize the relative burden of AF. Hospitalization data are presented for the number of hospitalizations, age grouping, length of stay, and total hospital bed utilization. We report data in age groupings of <50, 50 to 59, 60 to 69, 70 to 79, and ≥80 years. The prevalence of hospitalizations are expressed as the number per 10,000 population, and midyear population estimates were sourced from the Australian Bureau of Statistics.
To ascertain the impact of procedures on hospitalization trends for these conditions, we evaluated trends in direct-current electrical cardioversion, electrophysiologic studies, and radiofrequency ablation procedures to provide further insight into the factors driving AF hospitalizations. Data for electrical cardioversions, electrophysiologic studies, and radiofrequency ablation procedures were available from 2000. Given that data for radiofrequency ablation procedures were only available separately from other electrophysiologic studies from 2004, we studied trends in these procedures separately; electrophysiologic studies were analyzed from 2000 to 2003 and radiofrequency ablation procedures from 2004 to 2007.
Time trends in the yearly number of hospitalizations were assessed using negative binomial regression models. Comparisons were made within and between conditions and by age group and gender. Time trends in the yearly prevalence of hospitalizations, defined as the number of hospitalizations in a calendar year divided by midyear population estimates, were analyzed as described previously but with the logarithm of the population size included as an offset variable in the models. Prevalence rates were also investigated by directly standardizing yearly hospitalization counts to the age and gender structure of the Australian population in 2007. Finally, time trends in length of stay and bed days used were assessed using negative binomial regression models. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, North Carolina), and statistical significance was set at p <0.05.
Results
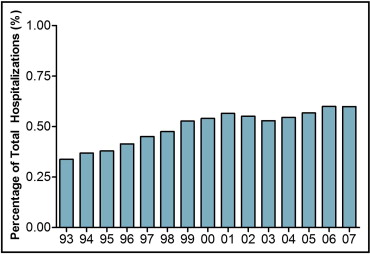
Over a 15-year period from 1993 to 2007, there were a total of 93,029,656 hospitalizations for any diagnosis in Australia (representing a follow-up period of almost 300 million person-years). There were a total of 473,501 hospitalizations for AF. There was a relative increase of 203% in the number of AF hospitalizations (7.9% annually, rate ratio [RR] 1.079, 95% confidence interval [CI] 1.069 to 1.088, p <0.001; Table 1 ). This was in contrast to a relative increase in the number of all hospitalizations of only 71% or an estimated 3.7% per year (RR 1.037, 95% CI 1.036 to 1.039, p <0.001). As a result, AF as a percentage of all hospitalizations increased by an estimated 4.0% per year (RR 1.040, 95% CI 1.031 to 1.050, p <0.001; Figure 1 ). These trends were additionally associated with a decrease in average length of stay (1.8% annually, RR 0.982, 95% CI 0.978 to 0.987, p <0.001) and an increase in total bed days used (5.9% annually, RR 1.059, 95% CI 1.055 to 1.063, p <0.001).
| Year | Number of Hospitalizations | Incidence of Hospitalizations (per 10,000 Population) | Average Length of Stay (days) | Total Bed Days Used (days) |
|---|---|---|---|---|
| 1993 | 15,555 | 8.8 | 4.2 | 64,608 |
| 1994 | 17,995 | 10.1 | 4.0 | 71,367 |
| 1995 | 19,601 | 10.9 | 3.8 | 74,496 |
| 1996 | 22,055 | 12.0 | 3.6 | 80,263 |
| 1997 | 25,096 | 13.6 | 3.5 | 87,536 |
| 1998 | 27,245 | 14.6 | 3.3 | 90,520 |
| 1999 | 31,109 | 16.4 | 3.2 | 99,867 |
| 2000 | 32,248 | 17.4 | 3.1 | 104,152 |
| 2001 | 36,156 | 18.6 | 3.1 | 112,984 |
| 2002 | 36,654 | 18.6 | 3.3 | 119,285 |
| 2003 | 36,191 | 18.2 | 3.3 | 117,723 |
| 2004 | 38,286 | 19.0 | 3.2 | 122,193 |
| 2005 | 41,510 | 20.4 | 3.2 | 134,405 |
| 2006 | 45,618 | 22.0 | 3.2 | 144,476 |
| 2007 | 47,164 | 22.4 | 3.1 | 145,200 |
| Relative increase, 1993–2007 ⁎ (%) | 203.2 | 155.0 | −26.2 | 124.7 |
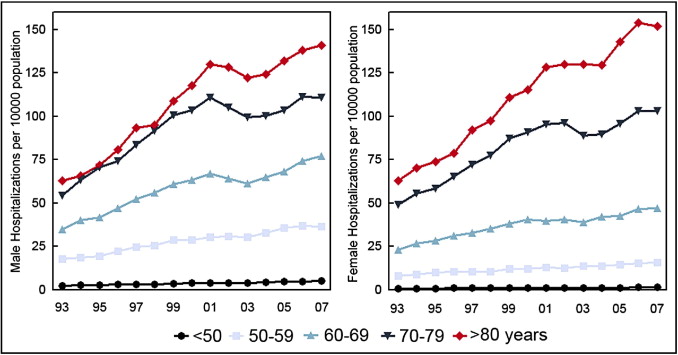
The proportions of AF hospitalizations for men and women were relatively steady over the study period, with men accounting for an average of 54.8% of hospitalizations and women for an average of 45.2%. Figure 2 shows the age- and gender-specific incidence of hospitalizations for AF from 1993 to 2007. The incidence of hospitalizations was higher in older age groups for every year. The proportion of patients hospitalized with AF and aged ≥80 years increased from 10% to 16% in men and from 25% to 34% in women.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


